Case study 1: NNP II
advertisement

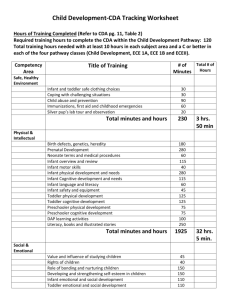
Running head: CASE STUDY 1: NNP II 1 Case study 1: NNP II Marissa Hampton and Gabriela Olivas University of Texas Medical Branch at Galveston School of Nursing Neonatal Nurse Practitioner II GNRS 5623 Dr. Debra Armentrout PhD, RN, MSN, NNP-BC And Dr. Leigh Ann Cates PhD, APRN, NNP-BC, RRT-NPS, CHSE June 23, 2014 CASE STUDY 1: NNP II 2 Case study 1: NNP II Case Study #1: [12 points] Michael Washington is a 715 gram, 27 week African American male infant born by emergency caesarean section (C/S) secondary to significant fetal distress after a failed attempt to stop preterm labor. Post delivery, baby Washington was intubated, received positive pressure ventilation with 22/5x 40 FIO2 1.00 via Neo puff, and given tactile stimulation. APGARS were 4,5,8 at 1, 5, 10 minutes respectively. Baby Washington was admitted to the NICU and placed on SIMV with a PIP of 22, PEEP of 5, rate 40, I-time 0.30. Maternal history is significant for the development of preterm labor at 26 weeks. Mrs. Washington had been hospitalized 3 days prior to delivery with tocolytics and bedrest. The tocolytics were discontinued at 27 weeks due to maternal fever, leaking membranes, meconium-stained fluid, and fetal heart rate decelerations. An emergency C/S was performed as above. 1. Would you have done anything differently in the delivery room? Why, why not? In the delivery room, if the infant did not initially cry, then I would ensue with intubation. In a delivery with meconium stained fluid intubation and suctioning below the vocal cords infant is the recommended practice for an infant who is not vigorous (Pappas & Walker, 2010). If the infant cried after delivery, then I would have deep suctioned and continued positive pressure ventilation per neonatal resuscitation guidelines. A vigorous infant with meconium stained fluid requires clearing of fluid from mouth, even if it is wiping while drying (Pappas & Walker, 2010). With either treatment modality, resuscitation would have begun at room air. With the use of a portable pulse oximetery, we could determine if our intervention was effective. If the infant did not have a change in oxygen saturation, then I would gradually increase the FiO2, remembering that infants may initially have a lower preductal oxygen saturation according to minutes old (Gomella, Cunningham, Eyal, 2014). If the infant continued to have poor or no respiratory effort then I would consider intubation. Once intubation was successful, I would have immediately tried to wean our FiO2. If infant was unable to wean or still continued to have difficulty exchanging gas, then I would consider administering a dose of surfactant to the infant. Early prophylactic surfactant administration helps restore pulmonary function and helps prevent further tissue injury (Gomella, et al, 2014). I would have administered… 2. What are your admitting diagnoses? 27 week African American preterm male, appropriate for gestational age (AGA), day of life (DOL) 1 Respiratory distress syndrome Suspected sepsis Suspected meconium aspiration syndrome 3. What are your differential diagnoses for the respiratory distress? Suspected meconium aspiration syndrome Suspected hyaline membrane disease CASE STUDY 1: NNP II 4. Write your admitting orders (if you would place on different respiratory support from that provided in the scenario, please write for that). Admit infant to NICU. Place infant in isolette. Initiate humidity at 70 percent, after 2 weeks may decrease humidity by 10 percent each day until reach 40 %, then off. Admission vital signs every (q) 15 minutes x 4, then q 30 minutes x 4, then hourly x 4, then q 3 hours. Admission weight, length and occipital frontal circumference (FOC). Admission four point blood pressures (bp), then hourly bp. Daily weight and weekly FOC. Strict intake and output (I&O’s). Intubate with 2.5 endotracheal tube (ETT). Ventilator settings: SIMV rate of 40 breaths per minute (bpm), peak inspiratory pressure (PIP) of 22, (PEEP) Of 5, inspiratory time of 0.30 seconds. Blood gases Q 6 hours. STAT chest x ray for ETT and umbilical line placement. Infasurf 2.1 ml via ETT x1 (in delivery room, 3ml/kg) Hold suctioning by ETT for 6 hours. Nothing by mouth (NPO). Place orogastric tube (OGT). Place umbilical arterial/venous catheters (UAC/UVC). Infuse clear IVF of 4 mEq of Na Acetate in sterile water + 0.25 units heparin/ml at rate of 0.5ml/hr (~15 ml/kg/day) Infuse D10% + 2 g/kg protein +1 meq KCl/100 + 2 mEq NaCl/ 100 +0.25 units heparin/ml at a rate of 2 ml/hr (~65 ml/kg/day, GIR 4.5) Admission laboratory: Admission blood culture Complete blood count (CBC), Arterial blood gas Type and screen Bedside glucose. In am obtain: CBC C reactive protein (CRP) Complete metabolic panel (CMP) Begin antibiotics: Ampicillin 50 mg/kg/day q 12 hours.. Gentamicin 5 mg/kg/dose Q 48 hours. . Admission medications: Erythromycin ointment both eyes(OU) x 1 Vitamin K IM injection 0.25 mg x 1 Caffiene citrate Loading dose: 8.9 mg IV q 12 hours times 2 doses (25 mg/kg/day) 3 CASE STUDY 1: NNP II 4 Maintence dose: 3.6 mg IV q 24 hours (5 mg/kg/day) AM chest/ abdominal xray Initial CXR to left. Initial CBC reveals a low WBC with an increased number of immature to mature neutrophils. 5. What are your differential diagnoses? Respiratory distress syndrome Pneumonia Sepsis of the newborn Situs Inversus 6. Based on the concerns for sepsis, would you order any additional diagnostic tests at this point? If so, what; if not, why not? Serial CRPs: will identify worsening sepsis. Increased CRP is elevated in 50-90 % of septic infants and usually peaks within 24 hours (Gomella et al, 2013). Serial CRPs may be helpful in determining duration of antibiotic therapy. Tracheal aspirate: Obtaining a tracheal aspirate may help identify our suspicion for pneumonia. Tracheal aspirate will use a gram stain to identify if any bacterial organisms exist and may therefore guide in determining antibiotic therapy and duration. Additionally, I would like to obtain mothers prenatal labs. These labs will identify any positive bacterial or viral infections, and if appropriate treatment was given. Case Study #2: [26 points] Lily Jones was born at 34 5/7 weeks (BW 2 kg) following an uncomplicated vaginal delivery. Pregnancy was complicated by premature labor and an upper respiratory infection 2 days prior to delivery. A maternal throat culture was done but results are unavailable. Lily was admitted to the Level II nursery for observation and was tolerating bottle feedings. She was noted to be jaundiced on DOL 1 and lab studies were ordered with the following results: Hct 43%; BBT B+/Direct Coombs negative; Bili T/D 12.8/0.7 @ 24 hours. 7. Based on the above information, what preliminary admission diagnoses would you consider for this infant? 34 week preterm AGA female infant DOL1 Hyperbilirubinemia Suspected hemolytic disease of the newborn Suspected sepsis 8. What additional diagnostic tests, if any, would you order at this time, and why? Mothers blood type Blood culture CBC with differential Reticulocyte count Liver function tests Q 4 hour T/D bilirubin levels Peripheral red blood smear Indirect coombs test ( pg 404) CASE STUDY 1: NNP II 9. 5 Briefly describe the bilirubin production cycle. Bilirubin is the product of erythrocyte destruction (Stokowski, 2011). More specifically, bilirubin is derived from the degradation of heme contained in the red blood cells (Wong, DeSandre, Sibley & Stevenson, 2011). When destruction of the red blood cell occurs, hemoglobin is released. Hemoglobin further breaks down and yields heme as a byproduct. Heme is then oxidized to biliverdin by enzymes. Bilirubin binds to albumin as is transported to the liver as unconjugated bilirubin. Transportation occurs as the molecule binds to albumin. While in the liver, bilirubin travels to hepatic cell membranes. Conjugation takes place here. Liver enzymes conjugate bilirubin, therefore making it water soluable for excretion. Conjugated bilirubin is then excreted into the bile, and exits the body via the intestines and kidneys during normal elimination patterns. Bilirubin that is not excreted may be reabsorbed and may revert to unconjugated bilirubin. Reabsoprtion occurs as unconjugated bilirubin enters the blood and recirculates for uptake back into the liver. This cycle is known as enterohepatic circulation and may cause an influx in unconjugated bilirubin levels (Stokowski, 2011). 10. What is the difference between physiologic jaundice, conjugated, and unconjugated jaundice? Physiologic jaundice is a progressive increase of serum unconjugated bilirubin levels that occur gradually over the first week of life. Increase in bilirubin levels typically occur after the first 24 hours of life. Normal red blood cell destruction in infants occurs 2-3 times that of adults. Decreased transport, enterohepatic circulation and breastfeeding are also contributing factors to physiologic jaundice. Conjugated jaundice is a measurement of direct bilirubin that is at least 20% of the total bilirubin value. An increased level of direct bilirubin level is a biochemical marker of cholestasis or hepatobiliary dysfunction (Gomella et al, 2013). Increased levels of direct bilirubin are not normal and are less common than physiological unconjugated bilirubinemia. Risk factors of conjugated jaundice include congenital infections, sepsis, neonatal hepatitis, ABO incompatibility and using total parenteral nutrition (Gomella et al, 2013). Infant clinically presents with prolonged jaundice, pale stools and darkened urine (Gomella et al, 2013). Unconjugated jaundice reflects the value of total serum bilirubin (TSB); that is the value of both indirect and direct circulating serum bilirubin level. Unconjugated bilirubin is derived from byproducts of hemoglobin metabolism. Conjugation in the liver must occur in order for the bilirubin to be excreted and for a decline in the overall TSB level. Depending on age, an increase in TSB levels may describe the disease process. 11. Interpret the following normal CBC and differential. Briefly discuss the significance of each parameter. WBC 7.6 RBC 5.6 Hgb 17.8 Hct 55% MCV 99 MCH 33 MCHC 33 Retic 1-3 Plts 213,000 Segs 55 Bands 0 Lymphs 9 Eos 2 Monos 5 CASE STUDY 1: NNP II 6 WBC- normal WBC has a wide range; 5,000- 30,000/mm3. Values lower than 5,000 may be indicative of leukopenia. Leukopenia is a significant finding in sepsis or pregnancy induced hypertension (PIH) (Lott, 2010). RBC- normal RBC range is 4-6 mm3. Total RBC equal production or destruction of circulating cells. RBCs are lower for earlier gestational age (Diehl-Jones & Askin, 2010). Hgb- Hemoglobin values depend on gestational age. Hemoglobin levels can be increased by delayed cord clamping and are typically highest in the first week after birth. Hemoglobin values are significant because this is the major iron containing component of the RBC. Hemoglobin carries oxygen to the tissues (Diehl-Jones & Askin, 2010). Hemoglobin levels are usually one -third of the hematocrit. Hct- Adequate hematocrit levels should be maintained to promote oxygenation to the tissues. Values usually rise soon after birth, then decline. Depending on current respiratory needs/ disease p rocess higher hematocrit levels may need to maintained. Normal hematocrit values are 40-55%. Higher hematocrit values (>65%) are indicative of polycythemia. MCV- Mean corpuscle volume- This is the average size and volume of a single RBC (Diehl-Jones & Askin, 2010). Either increase or decrease in values characteristically describes the size of the RBC. This value may be indicative of specific types of anemia. MCH- Mean Corpuscle Hemoglobin are average hemoglobin molecules in each RBC(Diehl-Jones & Askin, 2010). This values is also indicative of specific types of anemia. MCHC- Mean Corpuscle Hemoglobin Concentration is the concentration of hemoglobin in each RBC(Diehl-Jones & Askin, 2010). Helps identify anemia. Reticulocyte count- Measurement of how fast red blood cells are made from bone marrow fro replacement back into blood supply. Normal ranges of term infants are lower (4-5%) as opposed to preterm infants (up to 10%). Increased ranges above these levels may indicate hemolytic anemia (Gomella et al, 2013). Platelets- Normal range is 150,000-400,000/mm3 although total counts may be lower in infants who are small for gestational age. Lower platelet count prolongs bleeding times. Platelets may also be lowered due to maternal disease such as PIH and autoimmune diseases, such as lupus. Neonatal conditions that have significantly low platelet counts include alloimmune thrombocytopenia, sepsis, DIC or birth asphyxia (Diehl-Jones & Askin, 2010). WBC smear o Overall relevance of WBC differential determines the presence of infection using the I:T ratio. This ratio calculates the amount of immature WBC over the total WBC. The presence of increased immature WBC indicates infection, specifically a value over 0.2. Increased presence of immature WBC demonstrates the mature WBC pool is depleted due to decreased production or use. With lingering infection, the body must mount a response and does so with whatever kind of WBC is left, for example, immature cells. o Segs- Mature WBC responsible for inflammatory processes as seen with infection. o Bands-Immature WBC o Lymphs- T and B cell immunity o Monos- Immature WBC that macrophage invading cells. Monocytes are responsible for clearing old or invading cells from the circulation. o Eosinophils- CASE STUDY 1: NNP II 7 12 hours later, Lily suddenly became pale and voided a small quantity of burgundy colored urine. Vital signs were: HR 165; RR 45; BP 40/28; T 98.2. A UAC was placed and showed a MAP of 22 mmHg. Additional labs were done with the following results: Hgb Hct Retic Ct Peripheral smear D. Coombs Platelet count Prothrombin time (PT) Partial thrombo-plastin time (PTT) Thrombin time (TT) Fibrinogen Fibrin split products D-dimer Factor VIII Factor V Blood culture (prelim) 11.1 31% 17.1% Fragmented erythrocytes, decreased platelets Negative 35,000/mm 20.5 seconds 85.7 seconds 17.3 seconds 95 mg/dl 12 ug/ml 0.7 ug/mL 1.02 U/mL 0.99 U/mL Many Gm-positive organisms in clumps 12. What is the significance of the platelet count, PT, PTT, thrombin time, fibrinogen, fibrin split products, and d-dimer? Platelet count of 35,000 is significantly low. Normal platelet counts are between 150,000 to 400,000/ uL. Platelets provide a patchwork for intital blood vessel injury. A decreased platelet count inhibits the body’s ability to provide clot formation and therefore is unable to control bleeding. Risk factors for thrombocytopenia include infections, particularly TORCH or other bacterial/viral infections, disseminated intravascular coagulation (DIC), antiplatelet antibodies or situations that involve a considerable amount of hypoxemia. Pt level of 20.5 seconds is prolonged. Normal PT values are 10.6-16.2 seconds of an infant who is 30-36 weeks, DOL 1 (Nock & Patra, 2011). Prolonged PT levels indicate higher risk for bleeding. PTT level of 85.7 seconds is prolonged. Normal PTT values are 27.5-79.4 seconds for an infant who is 30-36 weeks on DOL 1 (Nock & Patra, 2011). Delayed PTT levels are also indicative of prolonged bleeding times due to decreased plasma levels of factors V to factor XI (Gomella et al, 2013). Thrombin times of 17.3 are prolonged. Normal ranges for thrombin times are 12-14 seconds. Thrombin times are significant because they help evaluate the level of fibrinogen present. If thrombin times are prolonged, this indicates a decreased fibrinogen level or functionality, which ultimately means increased risk for bleeding or DIC(). Fibrinogen levels of 95 mg/dL are low. Normal values are 200-400 mg/dL. Fibrinogen levels are uses to determine blood clot formation. Fibrinogen converts into insoluable fibrin, which inevitably forms a clot. A decrease in fibrinogen level signifies an inability for clot formation, and therefore increases the likelihood of DIC(). CASE STUDY 1: NNP II 8 Fibrin split products also help determine clotting stages. A level of 12 mcg/mL signifies an increase in clotting time, and predisposes the infant to DIC. Normal ranges for fibrin split products are levels less than 10 mcg/mL(). D-dimer: Clinical test that estimates fibrin lysis by plasmin. D-dimer is a sensitive marker of coagulation activation, particularly DIC. Increased D dimer values indicate DIC (Gomella et al, 2013). Varying ranges of normal noted. 13. What is the significance of Factor VIII and Factor V in the clotting cycle? The F5 gene is responsible for the production of Factor V. Factor V plays a significant role, along with other coagulation factors, in clot formation. Hepatic cells are responsible for Factor V cell production. After production, these cells remain relatively inactive until the coagulation system is activated and there is a need for clot formation. When Factor V is activated, it works in conjunction with other clotting factors, to convert prothrombin to its active form, thrombin. Thrombin then converts fibrinogen to fibrin, which essentially allows clot formation (Genetics Home Reference a, 2014). Secondly, factor V, in conjunction with activated protein C (APC), also plays a self-limiting role in regulating clot formation. APC controls clot formation by further inactivating Factor V, once clot formation is established. This regulation controls the size of clot formation at the site of injury (Genetics Home Reference a, 2014). . Deficiency of Factor V results in inability of normal clotting cascade. Factor V Leiden is a specific clotting abnormality that slows the rate of APC production. Slowed APC production inadvertently causes prolonged circulation of Factor V and Factor VIII. Prolonged circulation of these factors will cause abnormal clot size and formation. Increased formation of blood clots may unintentionally block narrowed blood vessels in the circulation. This abnormality is known as thrombophilia (Genetics Home Reference a, 2014). Like Factor V, Factor VIII also plays a crucial role in clot formation. Liver is major site of factor VIII production. Factor VIII is bound to von Willebrand factor in the circulatory system, and remains dormant until the clotting cascade is activated. Once activated, Factor VIII separates from von Willebrand factor and begins to interact with Factor IX This process initiates clot formation. Abnormalities in Factor VIII lead to reduced protein levels that result in an inefficient clotting cascade. These abnormalities lead to inability to form clots and control bleeding processes. This inability is also referred to hemophilia. The severity of disease is related to abnormality in Factor VIII production (Genetics Home reference b, 2014). 14. List your differential diagnoses for Baby Jones at this point, with a brief rationale for each. 34.5 week preterm AGA female infant DOL 2 DIC: Diagnosis of DIC is related to Baby Jones thrombocytopenia, prolonged PT and PTT levels, reduced fibrinogen and elevated D dimer levels. Additionally, baby Jones intial Hct level was 43% at birth and then decreased to 31 % by 36 hours of age. Infant is also pale and has a decreased urine output. Hypotension: As evidenced by central bp with mean of 22 mmHg. Possible bleeding may have occurred due to DIC. Thrombocytopenia: Decreased platelet levels are due to DIC cascade. Anemia: Decrease in Hct level from 43% to 31% in 12 hours. CASE STUDY 1: NNP II 9 Hyperbilirubinemia: Increased T/D Bili level 12.8/0.7 at 24 hours of age. If bleed is suspected we can anticipate that this value will increase without the use of phototherapy. Suspected Viral infection: Due to mothers history of throat culture and upper respiratory infection 2 days prior to delivery. Suspected sepsis is eliminated due to many gram positive organisms in clumps as seen on the blood culture. Presence of clumps indicates contamination Suspected Pre-renal Failure: Due to decreased blood flow and perfusion to kidneys. Decreased blood flow maybe due to hemorrhage, hypoxia, and hypotension. Burgendy urine is a characterisitic finding. 15. Briefly discuss the etiology for the pathophysiological processes that underlie the primary problem(s) that Baby Girl Jones is experiencing. DIC is an inappropriate cascade of activation and dysregulation of clotting factors. In DIC, active coagulation and accelerated fibrinolysis occurs simultaneously. The patient experiences both bleeding and thrombosis at the same time. Thrombocytopenia is common as the body is depleted of platelets and clotting factors. Contributors to the disease include exposure of blood to tissue factor, vascular injury, liver disease, thrombosis, birth trauma, hypoxia, acidosis, tissue necrosis or sepsis (Luchtman-Jones, Schwartz & Wilson, 2011). In baby girl Jones case, viral illness or hypoxia maybe the underlying cause of DIC. Our suspicion is greater with suspected viral infection as the mother presented with an upper respiratory infection 2 days prior to delivery. Furthermore, Baby Jones delivery was uncomplicated, indicating that birth trauma, hypoxia and acidosis are unlikely causes. Further complications of DIC include inappropriate bleeding events, therefore contributing to the infant’s hypotension and suspected pre renal failure. As hemorrhage ensues, less blood remains in the intra vascular space, causing hypovolemia and hypotension. Decreases blood in the vascular system leads to poor circulation. As a result, hypotension and a diminished perfusion to the infant’s organs occur. Hyperbilirubinemia 16. What treatment modalities are indicated at this point, and why? Treatment for suspected Viral infection: Treatment for hypotension o Hydration. Will give replacement with platelets and FFP. Begin IVF. Total fluid volume of 100 ml/kg/day Through UVC infuse D10 + ¼ NS +1 mEq KCl/100+ 1 Meq NaCl/100 + 0.25 units heparin/ml to run at 5 ml/hr (~60 ml/kg/day) o Consider NS fluid bolus of 10 mg/kg over 1 hour if still hypotensive after FFP and platelet transfusion. o Monitor hourly bp with UAC. o Keep MAP between 30 to 45 mmHg. o Consider dopamine if have reached near total fluid volume for the day and still hypotensive with MAP under 30 mmHg. Treatment for hyperbilirubinemia: o Begin single bank phototherapy o Apply eye shields. CASE STUDY 1: NNP II 10 o Recheck serum T/D bilirubin level q 4 hours (as infant current is in high risk zone for age. Treatment modality for DIC: o Treat underlying disease o Type and Cross for blood product administration o Platelet transfusion for thrombocytopenia: 10ml/kg (20 ml) over 1 hour IV x 1 o Redraw platelets 1 hours after completed infusion. o Fresh Frozen Plasma transfusion: Infuse 20 mL/kg over 2 hours IV x 1 (40 ml/kg/day total fluid) o Redraw D-dimer, PT, PTT, fibrinogen levels Case Study #3: [15 points] Sarah Jane Hill is a former 23 week gestation infant (BW 543 gm) who is now 32 wks PCA. Her hospital course is notable for RDS treated with 2 doses of surfactant; and continued oxygen requirement/vent support with chronic lung changes apparent on CXR. Other problems thus far include: PDA treated with unsuccessfully with indocin; followed by ligation HUSs have been negative X2 Numerous sepsis “rule-outs” – none proven. Treated with either Amp/Gent or Vancomycin & Tobramicin Feedings were started at 10 days of life with EBM/Premature Enfamil 24. These have been interrupted several times for “feeding intolerance” with no evidence of NEC. Yesterday, DOL 62, Sarah Jane began having more apnea/bradycardia episodes, and developed temperature instability. A CBC showed a left shift and a full sepsis w/u was done; Baby Hill was started on Vancomycin & Tobramicin. Feedings were stopped overnight for a bilious residual and IVFs were begun. KUB at the time showed enlarged & dilated loops of bowel. Today is DOL #63, current wt = 1320 gm. Sarah Jane is on NCPAP 6 cm with FiO2 ranging from 0.35-0.60 with O2 sats 82-98%. There are 3 A’s and B’s recorded for the past 24 hours, one which required vigorous stimulation to reverse. On exam this AM, you note that she is arousable and cries with abdominal palpation. There are few, if any, BS present. Lungs have the “usual” fine crackles throughout, and there is no murmur. The remainder of the exam is unchanged from previous exams. Morning labs are still pending, but the blood culture report shows “budding yeast”. CSF and gram stain is negative so far. KUB this AM shows a gasless abdomen. 17. Discuss the significance of the above events, the PE, X-ray findings, and the lab results. Preterm infants at 30-32 weeks postconceptual age have increased risks for necrotizing enterocolitis (Gomella et al, 2013). Baby Hill is a former 23 week, chronic lung infant who is now 32 weeks. Her age and contributing factors of chronic lung disease place her at an increased susceptibility to NEC. Although premature, Baby Hill’s course was relatively stable. Initial warning signs of illness presented as increased events of A/B episodes, abdominal tenderness and feeding intolerance. First, worsening A/B episodes indicate a change in status, possibly sepsis. The development of CASE STUDY 1: NNP II 11 bilious residuals with abdominal distention and discomfort indicate feeding intolerance. Decreased bowel sounds indicate decreased perfusion to the gut, as well as altered functionality. This am, Baby Hill’s assessment along with xray studies provided progressive worsening bowel disease. Initial worrisome films include visible and dilated bowel loops. Normal KUB should reveal gas patterns, however the presence of dilation indicates a change in abdominal status. Furthermore, Baby Hills abdominal xray continued to progressively worsening by displaying a gasless pattern. Abnormal gas patterns visualized on abdominal xrays are supportive findings of NEC (Gomella et al, 2013). Pending morning labs may either show an increased or decreased WBC, decreased platelet level and a left shift. These laboratory values may provide clues to whether NEC was a result of bacterial infection. Blood culture with budding yeast suggests a systemic candida infection. Negative CSF and gram stain indicate that the infection has not reached the meninges, and therefore has not crossed the blood brain barrier to suggest meningitis. 18. Discuss your differential diagnosis and plan of care at this point. Former 23 week, now 32 week female infant AGA DOL 63 Chronic Lung disease Apnea of prematurity Necrotizing entercolitis Confirmed Candida Sepsis The culture ID comes back the later that afternoon as C. parapsilosis in the blood. CSF remains no growth thus far. 19. Briefly discuss the etiology, risk factors, and usual treatment for fungal infections. Etiology Risk factors for obtaining C. parapsilosis in the blood are extreme prematurity, colonization with candida, the use of more than 2 or long duration of antibiotic therapy, long term parenteral nutrition(>5 days) or lipid administration (>7 days), invasive indwelling catheters or extended NICU stay (Chow, Linden & Bliss, 2012). As pertains to antibiotic therapy, the use of third generation cephalosporins place the infant at increased risk for C. parapsilosis (Chow, Linden & Bliss, 2012). With long term antibiotic therapy, the use of Diflucan is used to prevent Candida infections in the neonate. Diflucan is a potent fungistatic medication, however it is most effective against C. albanis, rather than C. parapsilosis. For Candidad prophylaxis, 3-6 mg/kg/dose IV infusion twice weekly is administered to extremely low birth weight infants who are at a high risk for fungal infection (Gomella et al, 2013). Antifungal medication for treatment of C. parapsilosis is the use of caspofungin. Caspofungin is a fungicidal agent that acts by inhibiting synthesis of the cell wall. Caspofungin is particularly effective against invasive organisms or those who have been resistant to other antifungal agents. Preterm infants should receive 2 mg/kg/dose IV q 24 hours over at least one CASE STUDY 1: NNP II 12 hour. Length of therapy should consist of 14 days from the last positive blood culture result (Gomella et al, 2013). Final efforts for antifungal treatment include the use of Amphotericin B. Amphotericin B is an antifungal agent that acts by disrupting the fungal membrane. Its broad spectrum properties allow for activity against Candida and other fungal infections (Gomella et al, 2013). Initial dose is 0.5 mg/kg iver 2-6 hours and maintence administration is 1-1.5 mg/kg IV q 24 hours for 2-6 weeks or longer. Continued monitoring of electrolytes, renal function tests, CBC and liver panel are necessary due to the drugs toxic nature (Gomella et al, 2013). Sarah Jane is now on day #14 of the treatment for C. parapsilosis that you prescribed above. She again develops increasing A’s and B’s. Blood cultures X2 are drawn and a cathed urine specimen is obtained with some difficulty, there is only enough urine for a culture. A bagged specimen was sent for routine U/A, which showed: “yellow, clear. pH 6.5, Sp gr 1.025; 3-5 WBCs and 2-3 RBCs; few hyaline casts.” 20. Discuss your plan of care at this point, giving rationales. Our plan of care will be guided at treatment of a urinary tract infection (UTI). Presenting factors of UTIs include respiratory distress with A/B episodes, and nonspecific findings include lethargy, irritability and poor feeding (Gomella et al, 2013). Obtaining and following urine culture results will indicate if the infant has current UTI. Blood cultures will monitor if the infection has become systemic. Additionally we will order a CBC, CRP. Consideration of a lumbar puncture will be necessary if the blood cultures have a positive result. The urine analysis results report normal color, pH and specific gravity. Small WBC and RBC indicate the presence of either urinary tract or kidney infection. The few hyaline casts present in her urinary sample are normal. Treatment for the suspected UTI is warranted due to WBC/RBC presence. Broad spectrum antibiotic treatment is indicated until the urine culture identifies a bacteria. That afternoon, the urine culture is reported as growing “gram-negative rods in pairs”. 21. Giving rationales for each, discuss your: a. differential diagnosis at this point Former 23 week, now 34 week female infant AGA DOL 77 Urinary tract Infection with E coli. as indicated by the presence of gram-negative rods in pairs in the urine culture. Confirmed candida sepsis: Continuing treatment, no on Day 14 of treatment. b. plan of care, including pharmacotherapeutics and further diagnostic w/u, if warranted. Further lab work CBC now and in am x 2 CRP now and in am x 2 BMP now (to identify pyelonephritis) Renal function studies now Electrolytes now Blood sugar now CASE STUDY 1: NNP II 13 Monitor blood cultures and obtain LP if blood culture negative Antibiotic therapy Begin Gentamycin for gram negative coverage: 4 mg/kg/dose IV q 24 hours Begin Cefotaxime (third generation cephalosporin with bactericidal activity against gram negative organisms including E.Coli) 100 mg/kg/day divided q 6-8 hours for 7-10 days. Begin Cefoxitin (second generation cephalosporin for gram negative enteric organisms including E.coli) 100 mg/kg/day divided q 6-8 hours for 7-10 days. Case Study #4: [16 points] Johnny Fields was delivered by emergency cesarean section; Apgar scores were 7/8 at 1/5 minutes respectively. Birth weight 834 grams, ~26 weeks gestation on exam. Initially Johnny was dried, stimulated, and suctioned orally. He developed increased work of breathing requiring intubation and surfactant administration. On admission to the NICU, he is noted to be lethargic with only occasional spontaneous respiratory effort, tachycardic to 190 BPM, with a peripheral BP of 30/20, MAP 24, axillary temp of 35.8 C. He is cyanotic with poor peripheral perfusion. Umbilical lines are placed, IVFs started at 80 ml/kg. Blood cultures are drawn and he is started on appropriate doses of antibiotics. A blood glucose of 20 mg/dl is treated with an IV bolus of D10W (2 ml/kg). 22. Identify, per system, possible signs/symptoms of sepsis that Johnny is demonstrating. Neurology: lethargy Cardiovascular: tachycardic with HR up to 190bpm, peripheral blood pressur of 30/20 with MAP 24, poor perfusion Respiratory: Increased WOB requiring surfactant administration, occasional spontaneous respiratory effort, cyanotic GI/FEN: Initial blood sugar of 20 mg/dL Other: Axillary temp of 35.8 C 23. What laboratory information do you want to order? CBC Blood culture Blood gas Repeat blood glucose 30 minutes after IV bolus of D 10 Type and screen The initial CBC shows: Hemoglobin 15.3 g/dL Hematocrit 46% WBCs 5000/mm3 Neutrophils 26% Bands 22% Metamyelocytes 1% Myelocytes 1% Lymphocytes 40% Monocytes 10% nRBCs 20/100 WBCs Platelet count 149,000/mm3 CASE STUDY 1: NNP II 14 Blood cultures drawn at the time of the sepsis evaluation grew GBS. Subsequent blood cultures drawn at 24 and 48 hours following the initial culture grew GBS as well. A lumbar puncture (performed once stable) demonstrated 3 WBC/mm3, normal CSF chemistries, a negative gram stain, and no growth at 48 hrs. A CXR revealed a white-out with small lung volumes and the presence of air bronchograms. 24. Calculate Johnny's absolute neutrophil count and his immature to total neutrophil ratio (I:T). 25. How would you interpret the a) blood culture results; b.) CXR findings; c.) CSF results? 26. Which antibiotics did you order on admission? 27. Based on the above lab results, would you change the antibiotics – why, why not. If so, to what? How long do you plan to treat Johnny with antibiotics? 28. What other supportive therapies should Johnny receive? Address all body systems. Johnny's HUSs obtained during his hospitalization were reportedly normal. He weaned from the ventilator, doubled his birth weight in 2 months, and was ready for discharge at 3 months post birth. He was discharged to the care of his local pediatrician as well as the high risk follow-up program. 29. How would you counsel Johnny's parents regarding his prognosis? Case Study #5: [3 points] Carlos Villareal is a newborn term infant born to a 22 year old, AB positive, antibody screen negative, gravida 2 para 2 Hispanic mother via repeat cesarean section at 38 weeks gestation. The infant required blow-by oxygen and positive pressure ventilation for 30 seconds before spontaneous respirations occurred. Apgar scores were 6 at 1 minute and 7 at five minutes. Birth weight was 2710 grams. On physical examination heart rate was 178 bpm, respiratory rate 64, temperature 36.9, and blood pressure 58/34 mm Hg. Carlos was pale, not jaundiced, and in moderate respiratory distress. Oxygen saturation with NC at 1 LPM @ 35% was 98%. The cardiac examination reveals a 2/6 systolic ejection murmur over the lower left sternal border, a liver edge 3.5 cm below the right costal margin, and decreased pulses. The rest of the physical examination is normal. 30. Highlight which of the following diagnoses would be consistent with this clinical picture: A. Perinatal hypoxic injury B. Septic shock C. Acute hemorrhage D. Congenital heart disease 31. Highlight what your first step would be in Carlos' management: A. Transfuse with 10mL/kg type O negative PRBCs B. Obtain a blood gas analysis for acid-base and ventilation status C. Intubate and provide 100% oxygen D. Administer prostaglandins CASE STUDY 1: NNP II 15 A spun hematocrit is determined to be 16% and the CBC has a hematocrit of 14.8%, hemoglobin 5 g/dL, MCV 94 fL, MCHC 32 g/dL, RDW 21%. Carlos' CBG shows: pH 7.10, PCO2 32 mm Hg, PO2 41 mm Hg, bicarbonate 8, and base deficit 16. Further maternal information reveals that Carlos' mother had noted decreased fetal movement during the last 2 days prior to birth. External monitoring prior to the cesarean section showed a sinusoidal pattern. There was no evidence of abruption or trauma to the placenta or cord. 32. Which of the following maternal lab tests would you want to order and why? A. Peat antibody screen B. Maternal CBC and RBC indices C. Kleihauer-Betke (KB) test D. GBS status E. Maternal LFTs Case Study #6: [2 points] Megan Kubiak is a newborn infant born at 34 weeks gestation to a 29 year old Caucasian mother. Initial CBC shows a hematocrit 28%, hemoglobin 9.1 g/dL, MCV 102 fL, MCHC 33 g/dL, RDW 11%, and peripheral smear shows moderate polychromasia. On examination Megan appears pale and in moderate respiratory distress. Vital signs reveal: HR 170 bpm, RR 65, BP: 44/33 mm Hg. Cardiac exam is significant for quiet heart sounds, a 2/6 systolic murmur, and equal pulses. Lung sounds are slightly diminished bilaterally. Abdomen is slightly protuberant with a spleen palpable 1 cm below the left costal margin and a liver palpable 2 cm below the right costal margin. 33. Highlight which of the following statements are true: A. This infant has nonimmune hydrops fetalis B. This infant has immune-mediated hydrops fetalis C. This infant has evidence of hydrops fetalis D. Rh hemolytic disease is a common cause of immune-mediated hydrops E. Tachy arrhythmia can be a cause of nonimmune hydrops fetalis 34. Highlight which of the following you would ask Megan's mother's obstetrician to order: A. IgG and IgM for CMV B. PCR for parvovirus B 19 C. Cervical culture for GBS D. Rapid plasma reagin and rubella screen E. Sputum for RSV and influenza Case Study #7: [5 points] There is a Rubella outbreak in the community. Mrs. Trevino wants to know if you can give the MMR immunization early to her 8 month old son. 35. What is rubella? 36. What diagnostic features (history and physical) are associated with rubella? 37. How will you respond to Mrs. Trevino's request? Case Study #8: [10 points] CASE STUDY 1: NNP II 16 Fifteen month old Adelaide Stevens is due to receive a MMR vaccine; however, she received immune globulin 2 months ago. 38. What is immune globulin? 39. Under what circumstances might Adelaide have received immune globulin? 40. What is MMR and how is it administered? 41. Are the components of this vaccine ever given as separate vaccines? 42. Can Adelaide receive her MMR vaccine today? If not when? Need to wait 10 months to received MMR vaccine after receiving IVIG. Case Study #9: [1 point] Danny Houston was a normal newborn born at tem. For the first six months of life he was only fed a commercially available infant formula which he tolerated well. At 6 months of age Danny's mother introduced fruit juices into Danny's diet after which he developed jaundice, hepatomegaly, vomiting, lethargy, irritability, and seizures. Tests for reducing substances were positive. 43. Highlight which of the following likely explains Danny's condition: A. Tyrosinosis B. Galactosemia C. Fructosemia D. Alpha -1 - antitrypsin E. Glucose -6-phosphatase deficiency Case Study #10: [10 points] On a routine screen, 2 week old Mia Harden is noted to have sickle cell disease (SCD). 44. How would you confirm that Mia has SCD? 45. Describe the pathology associated with SCD. 46. What is the inheritance pattern of this disease? 47. What aspects of Mia's physical exam would be important to include and note in your findings? Provide rationale 48. What lab work would you order to establish a baseline for future comparison? Provide rationale 49. Would you recommend that Mia's parents start her on folic acid? If so why? 50. Would you recommend starting Mia on an antibiotic for prophylaxis? If so, why? If so, what antibiotic, what dose, how often? CASE STUDY 1: NNP II 17 References Chow, B. D., Linden, J. R., & Bliss, J. M. (2012). Candida parapsilosis and the neonate: epidemiology, virulence and host defense in a unique patient setting. Expert Review of Anti- Infective Therapy 10(8), 935-46. Doi: 10.1586/eri.12.74. Diehl-Jones, W. & Askin, D. F. (2010). Hematologic disorders. In M. T. Verklan, & M. Walden (Eds.), Core Curriculum for Neonatal Intensive Care Nursing (4th ed., pp. 91-109). St. Louis, MO: Saunders Elsevier. Genetics Home Reference a.(2014). F5. Retrieved from http://ghr.nlm.nih.gov/gene/F5 Genetics Home Reference b. (2014). F8. Retrieved from http://ghr.nlm.nih.gov/gene/F8 Gomella, T. L, Cunningham, M. D. & Eyal, F. G. (2013). Neonatology: Management, procedures, on-call problems, diseases and drugs (7th Ed.). New York: McGraw Hill Education Lott, J. W. (2010). Imunnology and infectious disease. In M. T. Verklan, & M. Walden (Eds.), Core Curriculum for Neonatal Intensive Care Nursing (4th ed., pp. 91-109). St. Louis, MO: Saunders Elsevier. Luchtman-Jones, L., Schwartz, A. L. & Wilson, D. B (2011). The blood and hematopoietic system. In R. J. Martin, A. A. Fanaroff, & M. C. Walsh (Eds.), Neonatal-Perinatal Medicine: Diseases of the fetus and infant (9th ed., pp.1287- 1356). Philadelphia: PA: Mosby Elsevier. Pappas, B. E., & Walker, B. (2010). Neonatal delivery room resuscitation. In M. T. Verklan, & M. Walden (Eds.), Core Curriculum for Neonatal Intensive Care Nursing (4th ed., pp. 91-109). St. Louis, MO: Saunders Elsevier. CASE STUDY 1: NNP II 18 Stokowski, L. A. (2011). Fundamentals of phototherarpy for neonatal jaundice. Advances in Neonatal Care, 11(5s), 10-21. http://dx.doi.org/10.1097/ANC.0b013e31822ee62c Wong, R. J., & DeSandre, G.H., Sibley, E., & Stevenson, D. K. (2011). Neonatal jaundice and liver disease. In R. J. Martin, A. A. Fanaroff, & M. C. Walsh (Eds.), Neonatal-Perinatal Medicine: Diseases of the fetus and infant (9th ed., pp. 1419-1465). Philadelphia: PA: Mosby Elsevier.