Sample Case Checklist – Jenny Jones
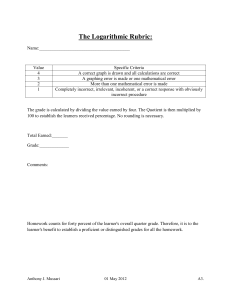
advertisement

Jenny Jones - Sample EOF Checklist 2015 (Needs H&P and complains of chest pain) SP Master Interview Rating Scale revised 2015 (MIRS) 1. Item 1: Opening () () () () () 5 4 3 2 1 Notes: The Learner opened by introducing themselves (including their last name), clarifying their role, and greeting the patient. The greeting should include good eye contact and a smile. 2. Item 4: Eliciting the Narrative Thread () () () () () 5 4 3 2 1 Notes: The Learner encouraged and let the patient talk about the patient's problem(s). The Learner did not stop the patient or introduce new information. 3. Item 5: Timeline () () () () () 5 4 3 2 1 Notes: The Learner obtained sufficient information so that a chronology of the chief complaint and history of the present illness can be established. The chronology of any associated symptoms is also established. 4. Item 6: Questioning Skills--Types of Questions () () () () () 5 4 3 2 1 Notes: The Learner begins information gathering with more than one openended question. This is followed up by more specific or direct questions. Each major line of questioning is begun with an openended question. No poor question types are used. 5. Item 8: Lack of Jargon () () () () () 5 4 3 2 1 Notes: The interviewer asks questions and provides information in language that is easily understood; content is free of difficult medical terms and jargon. Words are IMMEDIATELY DEFINED for the patient. Language is used that is appropriate to the patient's level of education. 6. Item 13: Verbal Facilitation Skills and Encouragement () () () () () 5 4 3 2 1 Notes: The Learner used facilitation skills throughout the interview. Verbal encouragement, use of short statements, and echoing were used when appropriate. 7. Item 14: Non-Verbal Facilitation Skills Notes: The Learner put the patient at ease and facilitated communication by using good eye contact; relaxed, open body language; and appropriate () () () () () 5 4 3 2 1 facial expressions; and by eliminating physical barriers. Physical contact was made with the patient, as appropriate. 8. Item 16: Encouragement of Questions () () () () () 5 4 3 2 1 Notes: The Learner encouraged the patient to ask questions about the topics discussed. The Learner also gives the patient the opportunity to bring up additional topics or points not covered in the interview (e.g., "We've discussed many things. Are there any questions you might like to ask concerning your problem?" Is there anything else at all you'd like to talk about?") This is particularly important at the end of the interview. 9. Comments: Exam Etiquette Revised 2015 (EE) 10. Learner is cleansing hands when he/she enters the room or tells you they have cleaned their hands or washes hands at any point prior to the physical exam () () Yes No 11. Drapes appropriately and protects modesty while examining you appropriately (not through gown or clothing) () () Yes No Notes: Lowers gown from above to just above nipple line to inspect and palpate upper chest. Raises gown from below to just below nipple line to palpate and auscultate lower chest. For abdomen raises gown and lowers sheet to expose all of abdomen down to top of pubic hair. For straight leg raising places sheet between legs before doing straight leg raising. 12. Learner describes physical exam or procedures to you () () Yes No Notes: Learner should tell patient that he/she is going to do a physical exam. Should explain in general terms each body system exam (I'm going to examine your heart now, I'm going to examine your abdomen now, etc.). 13. Learner considers your comfort during exam () () Yes No Notes: Pulls out foot rest when patient is laying down; avoids unnecessary position changes, helps or offers to help patient sit/stand up, is not unnecessarily rough with physical exam. 14. Learner closes visit properly. Notes: Learner indicates that visit is over gracefully and professionally. 15. Comments: () () Yes No Patient Satisfaction (PS) 16. Is this a doctor you would ( ) Definitely ( ) Probably ( ) Not see again in the future? Yes Yes Sure ( ) Probably ( ) Definitely No No 17. Comments: Pre-Encounter Learner Door Information (Door Info) Patient Door Chart: Name: Jenny Jones Age: Ask Your Patient Setting: Primary Care Physician's Office Chief Complaint: Needs an annual physical exam & complaining of chest discomfort BP 128/72 HR 84 RR 16 T 100.2 Learner Instructions (LII) Learner Instructions: You have 45 minutes to: 1. 2. 3. Elicit a complete (complete) history including chief complaint, history of present illness, past history, medications, allergies, family history, social history & review of systems Perform a complete physical exam which includes examination of each body system Demonstrate appropriate communication skills, professionalism, and skills that promote patient comfort and understanding. You will then have 10 minutes to: 1. Receive feedback from the patient and a faculty member. Honor Code (HC) 18. It is considered a violation of the honor code to discuss (either by giving or receiving information) cases, feedback, your performance, the logistics of the exam or anything related to this exam with others, either before, during or following the exam. Please initial in the box to the right that you agree to abide by the honor code for this case. Please select "SUBMIT" at the bottom of this section before you enter the exam room. Please do NOT close the Learning Space software program. Faculty Observation and Narrative History of Present Illness (HPI) 19. Establishes or confirms the chief complaint or reason for the visit. () () Yes No 20. Location of pain () () Yes No 21. Other symptoms associated with the pain: () () Yes No 22. Character of pain. () () Yes No 23. Alleviating factors. () () Yes No 24. Aggravating factors. () () Yes No 25. Timing of pain. () () Yes No Notes: Including onset, constant or intermittent, getting worse since onset, etc. 26. Environment/context in which pain occurs. () () Yes No Notes: Setting in which pain occurs (food, time of day, activity etc.) 27. Severity () () Yes No Notes: For pain quantified on a 10 pt. scale. For other symptoms (fatigue, shortness of breath, etc. better quantified by a description of how much it interferes with ADLs (activities of daily living). 28. History of this pain before. 29. Comments: () () Yes No Past History (PH) 30. Past medical history () Yes ( ) No () Yes ( ) No Notes: chronic illnesses, hospitalizations, immunizations 31. Past surgical history Notes: surgeries, major trauma, fractures 32. Past ob/gyn history ( ) Yes ( ) No ( ) Not Applicable (males) Notes: pregnancies, live births, 33. Prescription Medications () Yes ( ) No 34. OTC medications () Yes ( ) No 35. Medication allergies () Yes ( ) No 36. Learner mentions history of screening/health maintenance/immunizations, etc. () Yes ( ) No Notes: vitamins, herbs, etc. Notes: Any one mention is sufficient to score "yes." 37. Comments: Family History (FHx) 38. Asks generally about Family History. () Yes () No () Yes () No () Yes () No () Yes () No Notes: any disease runs in your family?, etc. The SP will have a position answer to this question. 39. Establishes health status of father or age at and cause of death Notes: Is your father living? If yes, how old is he and does he have any health problems? If no, how old was he when he died and what did he die of? 40. Establishes health status of mother or age at and cause of death Notes: Is your mother living? If yes, how old is she and does she have any health problems? If no, how old was she when he died and what did she die of? 41. Establishes number of siblings and health status of each or age at and cause of death. Notes: Do you have any siblings? For each sibling ask: Is your sibling living? If yes, how old is he/she and does he/she have any health problems? If no, how old was he/she when he died and what did he/she die of? 42. Asks about specific Family History related to current chief complaint. () Yes () No Notes: Examples: "Has anyone in the family had a disease or symptoms like this?" "Are there any diseases in your family in this body system (would indicate specific system)." 43. Comments: Social History (SHx) 44. Relationship status. () () Yes No Notes: Typical question might be: Are you in a relationship with anyone? May or may not follow up on answer to get more information about the relationship for the purposes of this exam. 45. Employment status. () () Yes No Notes: At a minimum, must ask "what kind of work do you do" or a similar question. If retired, just ask "what kind or work did you do." 46. Living situation. () () Yes No Notes: Typically would find out whether patient lives in house or apartment (or is homeless), who with, etc. Any question is sufficient to score "yes." 47. Smoking history. () () Yes No Notes: If he/she has ever smoked need to find number of years and packs smoked per day. If prior smoker and has stopped need to find out how many years since he's smoked. 48. Alcohol intake. () () Yes No Notes: If yes, need to determine drinks/day (or week or month). 49. Recreational drug use. () () Yes No Notes: If yes, need to determine drug, quantity and frequency. 50. Sexual history. Notes: At a minimum should determine: () () Yes No 1. whether patient is sexually active 2. whether with men, women or both 3. is barrier protection used 51. Eating habits/diet. () () Yes No Notes: Any question about diet or eating habits will suffice. 52. Exercise/Activity () () Yes No Notes: Any question about exercise of level of activity will suffice. 53. Sources of stress. () () Yes No Notes: Any questions about whether patient experiences stress or whether there are stressors in his/her life will suffice. 54. Support systems. () () Yes No Notes: Any questions about support of friends and/or family, a support system, supportive environment or a question about being close to friends/family will suffice 55. Comments: Review of Systems (ROS) Scoring for ROS Student must ask at least 1 question for each system to score "yes." 56. General symptoms. () Yes () No () Yes () No () Yes () No () Yes () No () Yes () No () Yes () No Notes: e.g. weight loss, fatigue, fever, chills 57. HEENT symptoms Notes: e.g. blurry vision, sinus problems, sore throat 58. Breast symptoms. Notes: e.g. discharge, mass, skin changes 59. Endocrine symptoms. Notes: e.g. polyuria, polydipsia, polyphagia, heat/cold intolerance, history of thyroid issues 60. Pulmonary symptoms. Notes: e.g. hemoptysis, cough or dyspnea 61. Cardiovascular symptoms. Notes: e.g. chest pain, palpitations, syncope 62. Gastrointestinal symptoms. () Yes () No () Yes () No () Yes () No () Yes () No () Yes () No () Yes () No () Yes () No Notes: e.g. nausea or vomiting, change in bowel habits, diarrhea, black or tarry stools, trouble swallowing, change in appetite or diet 63. GU symptoms. Notes: e.g. dysuria, hematuria 64. Reproductive system symptoms Notes: e.g. post menopausal or last menstrual period and postmenopausal bleeding, pregnancy hx 65. Musculoskeletal symptoms. Notes: e.g. pain, stiffness, swelling 66. Neurologic symptoms. Notes: e.g. dizziness, numbness, weakness 67. Psychiatric symptoms. Notes: e.g. mood, depression 68. Lymphatic symptoms. Notes: e.g. swollen glands 69. Comments: Head, Ears, Eyes, Nose, Throat & Cerv Nodes (HEENT) 70. Palpates the frontal and maxillary sinuses. ( ) Correct Technique ( ) Incorrect Technique ( ) Not Done 71. Performs otoscopic examination. ( ) Correct Technique ( ) Incorrect Technique ( ) Not Done ( ) Correct Technique ( ) Incorrect Technique ( ) Not Done Notes: Uses otoscope correctly; retracts ear upward and back using the hand not holding the otoscope. 74. Performs fundoscopic examination. Notes: Must darken the room, hold the instrument correctly, get close enough to the patient, ask the patient to focus on a distant point and use the examiner's right eye to look at the patient's right eye (and examiner's left eye to look at the patient's left eye). If any of these items are omitted then the exam is not done "correctly." 75. Examines oropharynx. ( ) Correct Technique ( ) Incorrect Technique ( ) Not Done 76. Performs thyroid examination from behind the patient. ( ) Correct Technique Notes: Provides water for patient and asks him/her to swallow, palpates both sides of the neck one side at a time for lobes of thyroid ( ) Incorrect Technique ( ) Not Done Notes: Looks in the mouth with a light. 77. Palpates lymph nodes in the head and neck. If "piano" fingers used, learner does not score a check. [ ] Under chin/jaw [submental (under chin), submandibular (under angle of jaw) tonsillar] [ ] preauricular & postauricular (in front of and behind ear) [ ] occipital (base of skull) [ ] anterior & posterior cervical chain 78. Comments: Cardiovascular (CV) 79. Examines patient from the patient's right side ( ) Yes ( ) No 80. Auscultates carotids bilaterally. Must ask patient to hold breath. ( ) Correct Technique ( ) Incorrect ( ) Technique Not Done 81. Palpates carotids bilaterally one side at a time. ( ) Correct Technique ( ) Incorrect ( ) Technique Not Done ( ) Correct Technique ( ) Incorrect ( ) Technique Not Done ( ) Correct Technique ( ) Incorrect ( ) Technique Not Done ( ) Correct Technique ( ) Incorrect ( ) Technique Not Done Notes: If both are palpated simultaneously that is incorrect. If palpated before the carotids are auscultated, it is incorrect. 82. Assesses JVP Notes: Must raise the bed at least to a 30 degrees angle (or at angle where you can see top of neck veins), have the patient turn his/her head to the side and inspect the jugular venous pulse for height and wave patterns. This exam can be done with the patient turning his/her head away from or towards the examiner. 83. Exposes anterior chest sufficiently to inspect the anterior chest. Notes: Should be exposed from the nipple line upwards. 84. Palpates to the anterior upper left of the sternum for lifts, thrills, pulsations. Notes: Above nipple line. 85. Palpates apical impulse at the apex of the heart. ( ) Correct Technique ( ) Incorrect ( ) Technique Not Done ( ) Correct Technique ( ) Incorrect ( ) Technique Not Done 87. Auscultates heart with bell in the tricuspid and mitral area ( ) Correct Technique Notes: down the left sternal border (tricuspid) over the apex (mitral) ( ) Incorrect ( ) Technique Not Done Notes: In women the student or patient may need to displace breast. To do so the student should use the back of his/her hand or ask patient to do it herself. Women may also need to hold up the underwire or elastic of the bra. 86. Auscultates heart with the diaphragm in the correct 4 listening areas. Notes: right second interspace (aortic area) over left second interspace (pulmonic area), down the left sternal border (tricuspid) over the apex (mitral) 88. Palpates peripheral pulses bilaterally. [ ] brachial (elbow) [ ] radial (wrist) [ ] femoral (groin) [ ] popliteal (behind knee) [ ] posterior tibial (behind the inner ankle bone) [ ] dorsalis pedis (top of foot) 89. Checks for pedal edema by pressing on the patient's shin and/or ankles. ( ) Correct Technique ( ) Incorrect ( ) Technique Not Done 90. Comments: Pulmonary (Pul) 91. Auscultates posteriorly (in the back) ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done Notes: 3 locations on each side comparing left to right. Patient must be asked to breathe in and out through mouth or take deep breaths. Stethoscope must remain in contact with the skin throughout a full cycle of inspiration & expiration to score "correct." 92. Auscultates anteriorly bilaterally (upper chest above or below clavicles in front) Notes: Patient must be asked to take deep breaths or breathe in and out through mouth. Needs to listen at one place on each side (right/left). Stethoscope must remain in contact with the skin throughout a full cycle of inspiration & expiration to score "correct." 93. Auscultates the right middle lobe - laterally under right ( ) Correct arm pit or under R nipple/breast. Stethoscope must remain in Technique contact with the skin throughout a full cycle of inspiration & expiration to score "correct." ( ) Incorrect ( ) Not Technique Done 94. Comments: Abdomen & Inguinal Nodes (Abd) 95. Examines the abdomen standing at the patient's right side. 96. Auscultates the abdomen (for bowel sounds) ( ) Yes ( ) No ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done Notes: prior to percussion or palpation for full credit. Only needs to listen to one location. Cannot listen over gown for full credit. 97. Percusses all 4 quadrants of the abdomen Notes: Must be done after auscultation for full credit 98. Percusses the liver Notes: Must percuss upper border from above and lower border from below. Needs to start at the level of the umbilicus or below. 99. Percusses over the splenic area and has patient take a deep breath and tap long enough to determine whether the percussion note changes Notes: in the left 9th intercostal space between anterior axillary and mid axillary line 100. Palpates the abdomen Notes: Must do light and deep palpation in all 4 quadrants for full credit. Can do light and deep at each location OR do light at 4 quadrants then deep at 4 quadrants. 101. Palpates for hepatomegaly Notes: May push up under the ribs while looking at patient's head or hook under the ribs while facing the patient's feet. In either technique must ask the patient to take a deep breath. 102. Palpates for splenomegaly Notes: Can do one-handed with patient supine or can use both hands and place one hand under the patient's back and instructs patient to turn on right side and take a deep breath while the examiner feels under the left ribs. 103. Comments: Neuro Exam (Neuro) 104. CN II: Optic: fundoscopic ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done Notes: Must be in darkened room for full credit. Should ask patient to focus on a distant point. Must get close enough. All three criteria required for full credit. 105. CN II: Optic: visual fields by confrontation Notes: Has patient focus on nose or forehead; Keeps hands 2-3 ft away from patient's eyes; Check each central field with finger count (1,2,5) or finger wiggle in each quadrant; Tests each eye independently with patient covering one eye at a time. All instructions must be given to patient and all steps done correctly for full credit. 106. CN II & III: Optic & Oculomotor: direct and consensual pupil exam Notes: Must do both for full credit. In direct pupil contraction is noted when a light is shined that that eye. For consensual, pupil contraction is noted when a light is shined in the opposite eye. 107. CN III, IV, and VI: Oculomotor, Trochlear, and Abducens - Check EOMs Notes: The patient must be instructed to follow the examiner's finger or a light without moving the head. 108. CN III, IV, and VI: Oculomotor, Trochlear, and Abducens - Pupil reaction to accommodation. Notes: The patient must be told to focus on a distant object in the midline then on an object close to the patient's nose. 109. CN V: Trigeminal: Tests light touch (with cotton ball, q tip cotton or finger tip) or temperature (tuning fork is cold/must warm one side) using one modality on all three areas bilaterally. Notes: Must do bilaterally in all areas (temple, cheek, chin) for full credit. Must touch lightly and cannot rub area. 110. CN VII: Facial Test facial muscle strength: wrinkle forehead/grimace/show teeth/smile ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done 111. CN VIII: Acoustic: Checks hearing by finger rub or whisper. ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done 112. CN IX & X: Glossopharyngeal and Vagus: palatal elevation ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done Notes: Must do one for full credit. Notes: Have the patient say "ah" while looking at palate. The learners are instructed NOT to do gag reflex. Note that this may be combined with looking in the patient's mouth. 113. CN XI: Spinal Accessory: shrug shoulders and head turn against resistance Notes: Must do both for full credit. 114. CN XII: Hypoglossal: stick out tongue; push out tongue on each side and assess strength. Notes: Must do both for full credit. 115. Sensation: Light touch arms & legs. Notes: Must ask patient to close eyes. Must test bilaterally. Must test exact site (i.e. doesn't drag stimulus across) Must test both arms and legs. 116. Sensation: Sharp/dull arms & legs. Notes: Must ask patient to close eyes. Must test bilaterally asking “sharp or dull?” Must test exact site (i.e. doesn't drag stimulus across) Must test both arms and legs. 117. Sensation: Vibration hands & feet. Notes: Must ask patient to close eyes. Must determine that patient feels vibration and not simply touch. Must test bilaterally with tuning fork on a bony prominence. Must test both hands and feet. 118. Sensation: Joint position sense of big toe bilaterally. ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done ( ) Correct Technique ( ) Incorrect ( ) Not Technique Done Notes: Must ask patient to close eyes. Must grip toe laterally and avoid touching nearby digits which would give clues. Ask patient to identify position (up or down). Must test bilaterally. 119. Reflexes Notes: Must check all of the following bilaterally for full credit: Biceps, Triceps, Brachioradialis, Patellar (knee jerk), Achilles (ankle jerk) and Babinski (plantar) 120. Gait: regular gait, toe walking, heel walking, tandem gait Notes: must do all for full credit. Walking on toes and heels will also fulfill ankle dorsiflexion and ankle plantar flexion. 121. Romberg (Patient stands with eyes closed). Notes: Patient should be instructed to stand with feet together and eyes closed. Examiner should stand close to patient to prevent injury. Both are required for full credit. 122. Cerebellar function: dysmetria and ataxia: finger to nose AND heel to shin Notes: must be both bilaterally for full credit 123. Cerebellar function: dysdiadokinesia: rapidly alternating movements Notes: can do either one hand in the other or tap heel repetitively 124. Comments: Musculoskeletal Examination (PE-M/S) 125. Did the student palpate all joint [ ] fingers areas (for swelling, redness or warmth) [ ] hands by identifying joint spaces and [ ] wrists comparing side to side [ ] elbows [ ] shoulders [ ] hips [ ] knees [ ] ankles [ ] toes 126. Did the student assess active [ ] TMJ joint by opening/closing mouth and moving jaw range of motion of the following joints side to side bilaterally? [ ] C spine (flexion/extension, rotation, lateral bending to each side) [ ] Back (flexion/extension, rotation, lateral bending to each side) [ ] Shoulder (abduction, forward flexion, horizontal abduction, internal rotation, adduction, backward flexion (extension), horizontal adduction, and external rotation) [ ] Elbow (flexion/extension) [ ] Forearm (pronation/supination) [ ] Wrist (flexion/extension, abduction/adduction, ulnar/radial deviation) [ ] MCP (flexion/extension, abduction/adduction) metacarpophalangeal (knuckles) [ ] PIP/DIP (flexion/extension) - fingers [ ] HIP: (flexion/extension, internal/extension rotation, abduction/adduction) [ ] Knee: (flexion/extension, hyperextension) [ ] Ankles: (dorsiflexion, inversion, plantar flexion, eversion) [ ] Toes: (flexion, extension) 127. Did the learner assess strength against resistance bilaterally. [ ] Shoulder abductors & adductors [ ] Shoulder horizontal abductors & adductors [ ] Shoulder internal & external rotation [ ] Elbow biceps & triceps [ ] Wrist flexors & extensors [ ] Fingers abduction & adduction [ ] Fingers grip [ ] Hip flexors & extensors [ ] Hip abductors & adductors [ ] Knee flexors & extensors [ ] Ankle dorsiflexion (stand on heels) [ ] Ankle plantar flexors (stand on toes) [ ] Ankle inverters & everters Student of Concern & Performance Deficits (SOC) 128. Do you have concerns about this student? () Yes () No Notes: Concerns may include: below average overall, below average in a single section, concern about an area not included in the checklists. 129. Comments re skill deficits observed: