Lec 09: Urticaria
advertisement
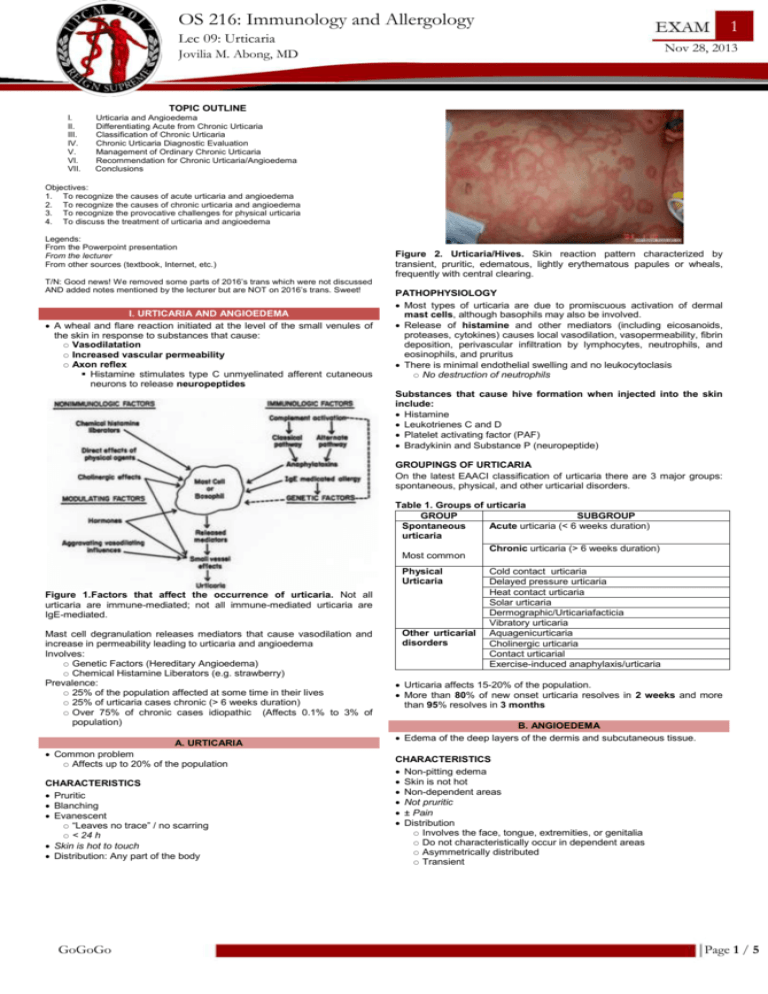
OS 216: Immunology and Allergology 12 Lec 10: 09: Urticaria and Angioedema November 2013 Nov 28, 28, 2013 Jovilia M. Abong Abong, MD TOPIC OUTLINE I. II. III. IV. V. VI. VII. Urticaria and Angioedema Differentiating Acute from Chronic Urticaria Classification of Chronic Urticaria Chronic Urticaria Diagnostic Evaluation Management of Ordinary Chronic Urticaria Recommendation for Chronic Urticaria/Angioedema Conclusions Objectives: 1. To recognize the causes of acute urticaria and angioedema 2. To recognize the causes of chronic urticaria and angioedema 3. To recognize the provocative challenges for physical urticaria 4. To discuss the treatment of urticaria and angioedema Legends: From the Powerpoint presentation From the lecturer From other sources (textbook, Internet, etc.) T/N: Good news! We removed some parts of 2016’s trans which were not discussed AND added notes mentioned by the lecturer but are NOT on 2016’s trans. Sweet! I. URTICARIA AND ANGIOEDEMA A wheal and flare reaction initiated at the level of the small venules of the skin in response to substances that cause: Vasodilatation Increased vascular permeability Axon reflex Histamine stimulates type C unmyelinated afferent cutaneous neurons to release neuropeptides Figure 2. Urticaria/Hives. Skin reaction pattern characterized by transient, pruritic, edematous, lightly erythematous papules or wheals, frequently with central clearing. PATHOPHYSIOLOGY Most types of urticaria are due to promiscuous activation of dermal mast cells, although basophils may also be involved. Release of histamine and other mediators (including eicosanoids, proteases, cytokines) causes local vasodilation, vasopermeability, fibrin deposition, perivascular infiltration by lymphocytes, neutrophils, and eosinophils, and pruritus There is minimal endothelial swelling and no leukocytoclasis No destruction of neutrophils Substances that cause hive formation when injected into the skin include: Histamine Leukotrienes C and D Platelet activating factor (PAF) Bradykinin and Substance P (neuropeptide) GROUPINGS OF URTICARIA On the latest EAACI classification of urticaria there are 3 major groups: spontaneous, physical, and other urticarial disorders. Table 1. Groups of urticaria GROUP SUBGROUP Spontaneous Acute urticaria (< 6 weeks duration) urticaria Most common Physical Urticaria Figure 1.Factors that affect the occurrence of urticaria. Not all urticaria are immune-mediated; not all immune-mediated urticaria are IgE-mediated. Mast cell degranulation releases mediators that cause vasodilation and increase in permeability leading to urticaria and angioedema Involves: Genetic Factors (Hereditary Angioedema) Chemical Histamine Liberators (e.g. strawberry) Prevalence: 25% of the population affected at some time in their lives 25% of urticaria cases chronic (> 6 weeks duration) Over 75% of chronic cases idiopathic (Affects 0.1% to 3% of population) A. URTICARIA Common problem Affects up to 20% of the population CHARACTERISTICS Pruritic Blanching Evanescent “Leaves no trace” / no scarring < 24 h Skin is hot to touch Distribution: Any part of the body GoGoGo Other urticarial disorders Chronic urticaria (> 6 weeks duration) Cold contact urticaria Delayed pressure urticaria Heat contact urticaria Solar urticaria Dermographic/Urticariafacticia Vibratory urticaria Aquagenicurticaria Cholinergic urticaria Contact urticarial Exercise-induced anaphylaxis/urticaria Urticaria affects 15-20% of the population. More than 80% of new onset urticaria resolves in 2 weeks and more than 95% resolves in 3 months B. ANGIOEDEMA Edema of the deep layers of the dermis and subcutaneous tissue. CHARACTERISTICS Non-pitting edema Skin is not hot Non-dependent areas Not pruritic ± Pain Distribution Involves the face, tongue, extremities, or genitalia Do not characteristically occur in dependent areas Asymmetrically distributed Transient Page 1 / 5 Lecture 09: Urticaria and Angioedema OS 216 B. PHYSICAL URTICARIA Reproducible by environmental factors Physical stimuli Most frequently in young adults Episodic and often limited to areas of inciting stimulus Overall, treatment with non-sedating antihistamines Usually unresponsive to corticosteroids except for delayed pressure urticaria Example: See Table 1 for more subgroups. Dermatographism – a physical urticaria Figure 3: Angioedema of the face II. DIFFERNTIATING ACUTE AND CHRONIC URTICARIA A. ACUTE URTICARIA Duration of few days to few weeks (< 6 weeks) Incidence of 15-20% of population Etiology usually detected Most cases are mild and never seen by physician (because it quickly disappears; seek consult when prolonged) CAUSES Viral infections particularly in children In adults: prodrome of HBV, infectious mononucleosis (EBV) Drugs NSAIDS, penicillins and derivatives, radiocontrast media Foods Non–allergic (e.g., scombroid fish poisoning) Allergic/IgE–mediated (e.g., nuts, shellfish) Immunization vaccines (e.g., MMR, tetanus toxoid) INVESTIGATION OF ACUTE URTICARIA Many cases require no investigation The cause is evident to patient and doctor alike Skin prick tests may support the diagnosis Avoid SPT in severely affected patients and in patients with current angioedema or a history of angioedema Serum IgE testing may also help confirm the culprit B. CHRONIC URTICARIA AND ANGIOEDEMA > 6 weeks Probability of having urticarial and/or angioedema: Hives and angioedema (40%) Hives alone (40%) Angioedema alone (20%) ETIOLOGY Difficult to determine; cause is rarely found Common in 3rd and 4th decade of life Usually not foods, drugs, pollens, infections, “dyes” Bad News: May last for years MOST COMMON CAUSES OF CHRONIC URTICARIA 66-93% chronic spontaneous 4-33% physical 1-7% cholinergic DURATION OF SYMPTOM RESOLUTION 50% of patients become symptom-free after 3 months and 80% after 12 months 11% suffer for 5 years Peak between 20-40 years of age (during working age) Women twice more affected than men III. CLASSIFICATION OF CHRONIC URTICARIA A. CHRONIC SPONTANEOUS URTICARIA (IN CHILDREN) Success rate of locating etiology: 21-55% Infections appear to have a more significant role (recurrent URTI, pharyngitis, tonsillitis, sinusitis, otitis, UTI) Streptococci, H. pylori, Staphylococci, Chlamydia Chronic infection is a more common trigger in children Food allergy (egg, milk, soy, peanut, seafood, wheat) More common cause of acute urticaria Food intolerances (additives) and drug allergy may be present Comorbid diseases: thyroid autoimmunity, coeliac disease GoGoGo Figure 4. Dermatographism. Scratching skin results in hives lasting 30 mins to 2 hours. CASE If shoulder swells (angioedema) 4-6 hours after carrying a heavy shoulder bag? Answer: Delayed pressure-induced urticaria and angioedema Note: may require corticosteroids If patient develops hives only while mowing the lawn? Answer: Vibratory-induced urticaria DIAGNOSTIC PROCEDURES Table 2. Diagnostic procedures to elicit physical urticaria Types Procedure Aquagenic urticaria Apply water compresses Cholinergic Have the patient run up and down stairs to urticaria induce sweating (appears when core body tempearature is increased by 1ºC) Cold urticaria (ice cube test) Delayed pressure urticarial Dermatographism Solar urticaria Vibratory angioedema Can be induced by stress, warm bath and exercise Holding an ice cube to the forearm removing, then re-warming will quickly elicit a hive Weight the skin with a sandbag for a short period, then observe skin after three hours [observe for angioedema] Stroking the back will produce a hive in a few minutes Phototest patient (special lamp needed) Apply a vibratory lab mixer to the forearm [observe for urtication] Interestingly, a negative ice cube test does not negate the possibility of cold urticaria. If you suspect cold urticaria, and have a negative ice cube test, then place the whole arm in cold water, or if the outside temperature is cold enough, ask the patient to stand outside for a few minutes. Cholinergic – small hives with widespread erythema Dermographism can be induced with a calibrated, spring loaded dermographometer C. ASSOCIATION OF CHRONIC URTICARIA AND ANGIOEDEMA TO AUTOIMMUNE DISEASE Table 3. Diseases associated with chronic urticaria Associated Diseases Autoimmune Person develops autoantibodies to the high affinity IgE receptor (FcεR) (40%) Hives: 4-36 h Thyroid Disease Thyroid function tests Association Thyroid autoantibodies (i.e. Hashimoto’s) Hives: 4-36 h? Idiopathic Hives: 4-36 h Urticarial Rare Vasculitis Systemic or isolated Hives: > 24 hours Leaves a faint hyperpigmentation after they disappear AUTOIMMUNE ASSOCIATION 35% to 40% of patients have IgG antibody to ɑ subunit of IgE Page 2 / 5 Lecture 09: Urticaria and Angioedema OS 216 Hashimoto’s disease is the only systemic disorder with common association (possibly reflects underlying autoimmune process for both) Occasionally manifestation of a connective tissue disease such as SLE (cutaneous vasculitis accounts for < 1%) URTICARIAL VASCULITIS Inflammatory injury of capillaries and postcapillary venules in the skin (as well as increased vascular permeability) Etiology: Manifestation of systemic disease (usually); some are isolated in the skin Clinically: Hives persisting > 24 h Pruritic Painful, stinging, burning sensation “Leaves a trace” Faint residual hyperpigmentation, indicating RBC extravasation (usually colored light brown) Figure 6. Autoantibodies involved in chronic immune urticaria. IgG anti-FcεRI is more common than IgG anti-IgE. B. DIAGNOSTIC ALGORITHM See Appendix 1. Figure 5. Urticarial vasculitis CAUSES OF URTICARIAL VASCULITIS Autoimmune connective tissue disease: (Sjogren’s syndrome, SLE, RA) Viral hepatitis B and C Paraproteinaemia: (Schnitzler’s syndrome occasionally has a vasculitic histology) Inflammatory bowel disease IV. CHRONIC URTICARIA: DIAGNOSTIC EVALUATION There is no single test for urticaria! 1. History & Physical Exam Diary (food intake, medications, environment, activities) Relationship of hives with menstrual cycle? C. ASST Detects autoantibodies to the IgE receptor Positive test (auto-reactivity) seen in 1/3 of patients with CSU ASST – positive patients have more severe symptoms, longer duration of disease, require higher doses to control symptoms Significance of a negative ASST: essentially rules out autoimmune urticaria Significance of a positive ASST: indicates the presence of autoreactivity in the serum, but in- vitro confirmation is required before this can be identified as due to functional autoantibodies V. MANAGEMENT OF CHRONIC ORDINARY URTICARIA A. MANAGEMENT GOAL 1: GENERAL TREATMENT Avoidance of: NSAIDS, alcohol, spicy food Overtiredness and stress Wearing of tightly fitting garments, footwear Strenuous physical exercise Overheated ambient temperature B. MANAGEMENT GOAL 2: SYMPTOMATIC THERAPY 2. Provocative tests for physical causes (if physical urticaria is suspected) 3. Laboratory tests: CBC with differential, ESR, CRP, UA, LFTs Thyroid function, anti-thyroid antibodies Skin tests Autologus serum skin test (ASST) – autoantibody against IgE receptor for chronic autoimmune urticaria Complements 4. Skin biopsy Generally, not helpful except in urticarial vasculitis Indications: Lesions lasting > 24-48 h Atypical? Scarring RBC extravasation Cutaneous vasculitis Urticaria pigmentosa − lesions where there are many mast cells in the area 5. Refractoriness to therapy Figure 7. Anti-histamines. 1st generation anti-histamines are nonselective (i.e., they have anti-cholinergic and anti-muscarinic effects) and sedating. A. DIAGNOSIS OF CHRONIC IMMUNE URTICARIA Autoantibodies (Fig. 6) Functional IgG anti-FcεRI (30%) – more common Functional IgG anti-IgE (5-10%) Antihistamines must be considered as first-line symptomatic treatment for urticaria because all symptoms of urticaria are mediated by H1 receptors on nerves and endothelial cells. Immunoblotting has been unsuccessful ASST Intradermal injection of subject’s serum Wheal and flare reaction after 30 min Basophil CD203c Expression To confirm previous procedure, but not available in the Philippines GoGoGo THERAPEUTIC OPTIONS Main therapy: H1 ANTI-HISTAMINES Why? Non-sedating, long-acting 2nd and 3rd generation antihistamines are more specific for H1 receptor, are less likely to cross the blood-brain barrier (hence non-sedating), and can be effective from 12-24 h. Improve pruritus and decrease formation of hives in mild chronic urticaria Page 3 / 5 Lecture 09: Urticaria and Angioedema Moderate/severe forms may benefit from higher doses (up to 4x the normal dose) Desloratidine, Loratidine, Fexofenadine Ebastine, Levocetirizine, Cetirizine SEDATION WITH ANTIHISTAMINES Clearly more evident with first generation antihistamines and more likely to adversely affect performance st If the patient sleeps poorly due to nocturnal sx, 1 generation may be helpful. CORTICOSTEROIDS Indicated when unresponsive to H1/H2 receptor blockers and LTRA Effective but with substantial side effects So alternate day therapy if must be used One approach – start 15-20 mg qod and taper to 2.5-5mg q three weeks, d/c after 4-5 months OS 216 NIKA: Fight! ADA: Roads go ever, ever on, Under cloud and under star. Yet feet that wandering have gone Turn at last to home afar. Eyes that fire and sword have seen, And horror in the halls of stone Look at last on meadows green, And trees and hills they long have known. - JRR Tolkien FRANCIS: COMBINED H1-H2 RECEPTOR ANTAGONISTS 85/15 ratio of skin H1/H2 receptors More H1 than H2 receptors; that’s why you have to give them as a combination Combination of anti H1 and H2 blockers provides additional treatment benefit Doxepin blocks (tricyclic anti-H1 blocker) both receptors and is a more potent anti-H1 blocker than diphenhydramine or hydroxizine Sedation may limit usefulness of doxepin SYMPATHOMIMETIC AGENTS Oral sympathomimetics (e.g. terbutaline) studied to reduce erythema/swelling Substantial side effects (insomnia, tachycardia) Low efficacy LTRA (leukotriene receptor antagonists) Zafirlukast and montelukast superior to placebo in treatment of chronic urticaria Have not been compared to therapy with antihistamines No additional effect once maximal antihistamine effect is achieved EXPERIMENTAL THERAPIES Cyclosporine at low doses (2.5-3 mg/kg) is effective and steroid sparing High dose (6 mg/kg) is very effective but with severe side effects Other less studied agents include sulfasalazine, hydroxychloroquine and dapsone, IV IgG Plasmapheresis is effective for patients with autoimmune urticaria (anti-IgE Ab) but it is impractical for long-term treatment RECOMMENDATIONS FOR CHRONIC URTICARIA AND ANGIOEDEMA Combination of therapies Triple drug therapy: H1 & H2 antagonists + LTRA Tricyclic antidepressants (doxepin) Immunomodulators (e.g. steroids, cyclosporine) Hydroxychloroquine, dapsone, CCBs, methotrexate, colchicine, pentoxyfilline, cyclophosphamide Antihistamines: mainstay of therapy (H1 and H2) Nonsedating at low/high doses effective for mild/moderate disease Older, sedating antihistamines more effective for severe urticaria and/or angioedema LTRAs are worth trying Minimize systemic corticosteroids (alternate day) VI. SUMMARY Hives are very common Acute urticaria < 6 weeks History is key to diagnosis Non-sedating anti-histamines as drug of choice Physical urticaria History is key to diagnosis Provocative tests as diagnostic tool Non-sedating anti-histamines Chronic urticaria > 6 weeks Etiology is rarely determined Therapy is difficult IT’S PAST YOUR BEDTIME. GO TO SLEEP. GoGoGo Page 4 / 5 Lecture 09: Urticaria and Angioedema OS 216 APPENDIX 1: DIAGNOSTIC ALGORITHM If chronic urticaria, do the following tests: Autoimmunity screening; Infectious disease screening; and Malignancy screening. HAE (hereditary angioedema): Recurrent angioedema alone C1 inhibitor (C1-inh) deficient Request for C1-inh screening If all (-): idiopathic urticaria Because we’re too idiot to know and the patient’s pathetic APPENDIX 2: CLASSIFICATION OF CHRONIC URTICARIA GoGoGo Page 5 / 5