TST Resource Guide - Washington State Pharmacy Association
advertisement

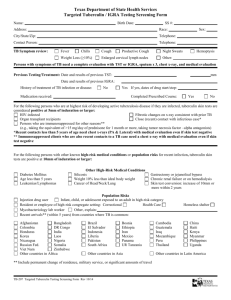
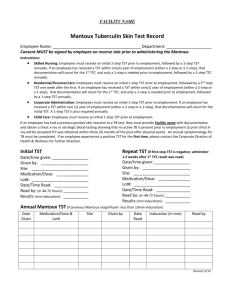
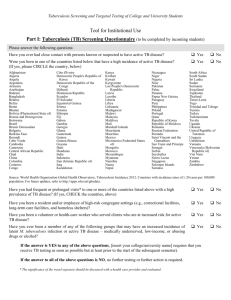
Tuberculin Skin Test Certificate Program Steps to complete Certificate: Complete classroom instruction with Tuberculin Skin Test placement with wheel, reading practice arms, and determining positive or negative result of cases. Watch voice-over-PowerPoint CE on WSPA website and complete test for the didactic portion. Send in both the form from the practicum with cases and verification of practice placement, didactic CE test* and WSPA evaluation and certificate form to the WSPA office, 411 Williams Ave S, Renton, WA 98057, fax to 425-277-3897, or email to wspa@wsparx.org. Learners must have a score of 70% to pass didactic study portion to complete the certificate. WSPA will send the certificate within 3-5 weeks. XYZ Pharmacy 12345 Main St. Seattle WA, 98115 p. 205.555.5555 f. 206.555.5554 TUBERCULIN SKIN TEST Name: ___________________________________________________________________ Date: ______________________ Address: _________________________________________________________________ Zip Code: ________________ Phone: ___________________________________ DOB: _________________________ Sex: (Circle one) M or F Doctor: _________________________________________________________ Dr’s Phone: ______________________ 1. Have you ever had a Tuberculin Skin Test (TST, also called a PPD)? If yes, when was the most recent: ______________ Was the result positive? _______ 2. Have you ever been diagnosed with tuberculosis? 3. Are you HIV positive? 4. Are you currently taking any drugs that affect your immune system (including steroids)? 5. Were you born outside the United States? If yes, how long have you lived here? _________ years 6. Have you received any live vaccines in the last four weeks? (MMR, yellow fever, polio, varicella, oral typhoid, nasal influenza, or herpes zoster) 7. Have you recently had contact with a person infected with TB? 8. Do you use intravenous (IV) drugs? 9. Do you have any chronic medical conditions? If yes, what: _____________________________________________________________________ 10. Have received the Bacille Calmette-Guérin (BCG) vaccine? This is the vaccine to prevent tuberculosis. 11. Are you a healthcare worker? 12. Women only: Are you currently pregnant? Yes No Yes Yes Yes No No No Yes No Yes No Yes Yes Yes No No No Yes No Yes Yes No No I have received and read the Patient Information supplied about the TST. I understand the risks. I authorize the pharmacist (or pharmacy intern under a pharmacist supervision) to administer the TST and interpret its results. I understand that a copy of this form, containing the test results, will be sent to my primary care or referring physician. I understand that the pharmacist will report any positive test results to the local health department in which I reside within 24 hours in accordance with Washington State Law, under WAC 246101-101. I understand that for my test to be valid I must return to have my test read in 48 to 72 hours by a pharmacist or pharmacy intern at this pharmacy. Signature______________________________________________________________ Date _________________________ For Internal Use Only: Name of Product Lot number Expiration Date Arm (circle) LEFT or RIGHT Pharmacist ___________________________________________________________________________________________ Date _______________ Printed Name Signature Date and Time: Placement________________________________ Reading________________________________ Induration: _____________mm. This result is POSITIVE or NEGATIVE (circle). Results faxed to physician and positive results reported by:______________________________ Date: ___________________ Pharmacy Tuberculin Skin Test (TST) Screening Answer Implications If the patient answered, “Yes” to any questions, further information is needed before performing a TST. See below for details. 1. Previous TST. Screen for hypersensitivity or other severe reactions (e.g. vesiculation, ulceration, necrosis) to previous test. If either occurred previously TST is not recommended. If pt had a previous positive result they are at higher risk of experiencing a severe reaction; counsel such pts about when to seek additional care for severe reactions. 2. Previous TB Diagnosis. Documented active TB or a history of treatment for TB infection or disease are both contraindications for TST. 3. HIV Positive. As CD4+ T-cell count decline the TST is less sensitive in these individuals. Test as soon as HIV positive status is known for best results. Accurate tuberculosis screening is very important in this patient population. Induration ≥5 mm is a positive result. 4. Pharmacotherapy impacting immune system. Decreased immune system activity can lead to a falsenegative result. Daily prednisone doses of 15 mg or less (or equivalent corticosteroid) are not considered high risk. Pts taking ≥ 15 mg prednisone daily for ≥ 1 month, or patients on other immunosuppressive therapy are at high risk of infection; ≥ 5 mm induration considered positive result. 5. Residence outside of the United States. Foreign-born persons arriving within the last 5 years from areas with high prevalence/incidence of TB (e.g., Asia, Africa, the Caribbean, Latin America) should be screen more sensitively (induration ≥10 mm is a positive result.) 6. Recent Live Vaccines. Decreased immune response can result in false-negative result. Defer TST for four to six weeks after administration of live vaccine. If TST must given concomitantly or recently after live vaccine administration, administer TST at separate site from vaccine. 7. Recent Contact with TB infected person. Patients are at high risk of infection, ≥5 mm of induration considered positive. 8. IV Drug Use. IV drug users are at an increased risk of TB infection; ≥ 10 mm induration is positive result. 9. Chronic Medical Conditions. Some medical conditions increased risk of TB infection. In patients with such conditions induration of ≥ 10 mm induration is considered positive. Such conditions include: diabetes mellitus, chronic renal failure, malignancies, weight loss of ≥10% of ideal body weight, silicosis, gastrectomy, and jejunoileal bypass. 10. BCG vaccine. Previous BCG vaccine can yield false-positive result. In the US we do not take this into consideration, and report the positive result based on measurement and risks without regart to BCG status. 11. Healthcare Workers. Health-care professionals, residents and workers in hospitals, nursing homes, mental institutions, prisons and other persons requiring periodic TB screening should initially receive a twostep test. This two-step process involves a second TST one to four weeks following an initial negative TST. If reaction to second test is positive, the individual is considered infected. If the reaction to the second test negative the individual is considered uninfected. TUBERCULIN SKIN TEST PROCEDURES AND PROTOCOLS How to Place a TST: Supplies: o Vial of tuberculin (Tubersolor Aplisol) o Single-dose disposable tuberculin syringe o ¼” to ½” 27-gauge needle o small gauze pads or cotton balls o 70% alcohol swabs o puncture resistant sharps container o ruler with millimeter markings Prepare dose o Wipe vial stopper with 70% alcohol swab and allow to dry o Draw 0.1 ml into syringe using aseptic technique, use care to exclude air bubbles o Check that the vial has not expired. When opening a new vial of tuberculin, mark an expiration date of 30 days from the day you open the vial. Discard the vial after this date. Refrigerate the vial after each use. Prepare the administration site o Preferred site is volar surface of forearm, approximately 4 inches below elbow. Dorsal side can be used. o Choose a clean, healthy site Avoid: hairy areas, areas with lesions, areas near veins, swollen or red areas or areas without adequate subcutaneous tissues, sores, tattoos or scars o Clean site with a 70% alcohol swab and allow to dry completely Administer TST—Intradermal Injection o Stretch the selected area of skin taut between thumb and forefinger, or using forefingers o Insert the needle into the most superficial layers of skin at a 5 to 15 degree angle. Release stretch on skin. Bevel should be facing upward or downward, perpendicular to the arm Bevel should be advanced approximately 3 mm through the epidermis Bevel should be completely covered by skin. o Inject slowly. A pale bleb 6 to 10 mm should form. o Remove needle without applying pressure to bleb. o Dispose of needle in sharps container. Do not re-cap before disposal. o It is common for a drop of blood to appear. Blot blood away with gauze or cotton ball. Do not cover bled with adhesive bandage. Properly dispose of blood contaminated gauze or cotton. o Verify proper administration by using ruler to ensure bleb is at least 6mm in diameter. If bleb is < 6mm in diameter, or not visible, then the test should be re-administered in a different location. How To Read a TST: Locate TST on inner aspect of lower arm. Place arm palm up, bent at elbow and resting on a smooth surface. Only the induration is to be measured, this is the firm palpable raised area surrounding the injection site. Erythema or mild swelling should not be measured. Rely primarily on palpation (with light sweeping motions of fingers) rather than visual inspection to identify the margins of induration. Measure induration across the forearm, from the thumb side to the little finger side or vice versa. Direction of measurement should parallel direction a watchband would lay across the wrist. Palpate widest margins on each side and mark with a small dot. Using a transparent ruler, place the zero millimeter mark at one margin and record the width of the induration. If result falls between two divisions of millimeter scale, record the lower mark. Do not record fractions of a millimeter. Record the exact measurement, not > or < a measurement breakpoint (ie. <10 mm, negative). Immediately record result in millimeters. Using pt demographics and answers to screening questions, interpret the result via the above guidelines as positive or negative. Fax a copy of all results to patient’s primary care provider or referring physician. If the result is positive, refer the patient to another provider for further testing. A warm referral, where you fax information to the provider is best. Provide patient with patient education materials and counsel them about the next steps to take for diagnosis. A positive TST is not a diagnosis. Guidelines for Interpreting Tuberculin Skin Test Reaction Induration Interpretation ≥5 mm Positive in the following groups: o Individuals with fibrotic changes on chest radiographs consistent with prior TB o Recent contacts of individuals with active TB o Individuals with known or suspected HIV-infection o Other immunosuppressed patients (patients receiving ≥15 mg of prednisone, or its equivalent, daily for ≥1 month; organ or bone marrow transplant patients; patients taking tumor necrosis factor-alpha antagonists) ≥10 mm Positive in the following groups who do not meet above criteria: o IV drug users who are HIV-negative o Individuals with medical conditions that increase risk of progressing from latent TB infection to active TB (e.g., diabetes mellitus, chronic renal failure, malignancies [e.g., leukemias, lymphomas, head/neck/lung cancer], weight loss of ≥10% of ideal body weight, silicosis, gastrectomy, jejunoileal bypass) o Residents/employees of high-risk congregate settings (e.g., prisons, nursing homes, long-term care/health-care facilities, homeless shelters, residential facilities for AIDS patients) o Foreign-born persons arriving within the last 5 years from areas with high prevalence/incidence of TB (e.g., Asia, Africa, the Caribbean, Latin America) o Some medically underserved, low-income populations (e.g., migrant farm workers, homeless persons) o High-risk racial or ethnic minority populations, as defined locally o Personnel in mycobacteriology laboratories o Children <4 years of age o Children (including infants) and adolescents exposed to adults in high-risk categories o Children who travel to areas with high prevalence of TB ≥15 mm Positive in individuals (including children ≥4 years of age) with no risk factors for TB Negative in normal, healthy individuals with no risk factors for TB (lack of hypersensitivity <15 mm to tuberculin); TB highly unlikely Test should be read 48-72 hours after placement of test. Record result in millimeters even if result is negative or zero mm induration. Induration is a firm and raised, erythema does not indicate a positive result. Your Pharmacy Letterhead here Tuberculin Skin Tests Results Patient name:_______________________________ Date of Birth: __________ Mantoux 5U test (Intermediate PPD) use only Date Administered: ____________ Date Read: _____________ Result (48-72 hours) ______mm of induration Tuberculin skin test was _____ Positive or ____ Negative If the tuberculin skin test is positive the patient was referred for chest X-ray and clinical evaluation by a physician or ARNP. Results faxed to physician: Yes____________ No_______________ Thank you, Pharmacist Name and contact information here