Embryo Large concepts 2012
advertisement

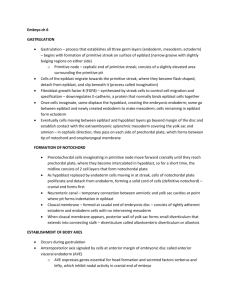
Embryology Gametogenesis (in general) G1 – synthesis of proteins and enzymes G2 – synthesis of microtubules, errors in replication checked o Fragile X – too many CGG repeats in gene that codes for protein necessary for brain development Gametes – originate from primary ectoderm, migrate to yolk sac (week 2) and along posterior abdominal wall to lower thoracic region (week 4-6), where they divide and induce surrounding tissue to differentiate into primitive sex cords o Genital ridges – give rise to Leydig cells or follicular cells o Maternal non-disjunction during gametogenesis is primary cause of Down Syndrome o Paternal non-disjunction is primary cause of Turner’s Syndrome Spermatogenesis Testes descend to scrotum during 7th month in utero o Enclosed in dense CT (tunica albuginea) which is thickened posteriorly to form mediastinum o CT septa extend from mediastinum to form 250 lobules o Each lobule consist of 1-4 seminiferous tubules (closed loops) surrounded by loose CT (interstitium). o Interstitium houses blood vessels, nerves, lymphatics and Leydig cells. Spermatogenesis – Type A dark spermatogonia Type A pale spermatogonia (may divide a few times) Type B spermatogonia primary spermatocytes secondary spermatocytes spermatids (these will be modified prior to ejaculation) –(spermiogenesis) spermatozoa Seminiferous tubules encased by tunica propria, which is covered by interstitium o Spermatogenesis in seminiferous tubules is patchy, so can find any stage anywhere o Movement of spermatogonia from basal to adluminal compartment involves disassembly and reassembly of occluding junctions (squeezes it like toothpaste) Key events of spermiogenesis o Formation of acrosome (membrane bound structure that contains hydrolytic enzymes that disperse the corona radiata and digest the zona pellucida) o Condensation of DNA o Shedding of cytoplasm o Formation of middle piece and tail (middle piece has lots of mitochondria, tail has 9+2 arrangement of microfibers) Hormonal influences of spermiogenesis o LH – stimulates Leydig cells to produce testosterone o FSH and testosterone both stimulate production of spermatozoa o Too much FSH produces inhibin, which tells hypothalamus to tell anterior pituitary to stop producing LH and FSH o Too much testosterone also tells hypothalamus to tell anterior pituitary to stop Spermatogenesis doesn’t begin until puberty (hence why you need testes-blood barrier) Spermatozoa can live for 5 days in female reproductive tract and are initially lethargic and incapable of fertilization o Interaction between sperm and mucosa of uterine tube removes glycoproteins from overlying acrosome, making it capable of fertilization (capacitation – takes about 7 hours) Oogenesis Oogenesis occurs in cortex of ovary, begins in utero o 1st meiotic division begins in 12th fetal week (arrested at prophase I at week 20) o Follicular maturation begins at puberty (each maturing follicle has an oocyte arrested at metaphase II) o Meiosis II is not finished unless a sperm unites with it, in which case the oocyte undergoes 2nd division right before pronuclei unite Ovulation – random whether from right or left side o 15-20 follicles begin to mature each month, but first one to mature causes the rest to degenerate by involution Primary follicle secondary follicle Graafian follicle (tertiary follicle) Graafian follicle bulges out of surface of ovary Follicle includes corona radiata (outside) and zona pellucida (inside) Corona radiata formed by cumulus oophorus cells of granulosa cells surrounding developing follicle Corona radiata easily penetrated by sperm that have undergone capacitation Acrosome reaction digests zona pellucida Hormones in ovarian cycle – LH and FSH spike at ovulation (LH spike stimulates completion of meiosis I), estrogen dominates until ovulation, and then progesterone dominates Fertilization Fertilization typically occurs in ampulla of uterine tube Involves fusion of oocyte and sperm plasma membranes (entire sperm contents, including tail, enter oocyte) When sperm head contacts oocyte plasma membrane, oocyte releases lysosomes that block penetration of plasma membrane by any other sperm (cortical reaction) and prevents binding of sperm to zona pellucida (zona reaction) Penetration of sperm into oocyte plasma membrane initiates o Cortical reaction and zona reaction o Resumption of meiosis II o Upregulates metabolism in oocyte and initiates early development Sperm loses tail and nucleus swells to become male pronucleus Nuclear membranes of sperm and oocyte dissolve and homologous chromosomes align (completion of fertilization) DNA is duplicated and zygote begins to undergo mitosis If fertilization does not occur, corpus luteum degenerates and the functional (compact and spongy) layer of the endometrium of the uterus is sloughed (menstrual flow) Uterus lining will regenerate over the next 28 days under influence of estrogen from ovaries Conception to Implantation Morula – day 3 (means “mulberry”) Blastocyst – day 5 (hollow ball of cells with an inner mass forming at one side o Outside of blastocyst forms trophoblast o Inner mass is embryonic stem cells that will form fetus o Blastocyst attaches to anterior or posterior wall of uterus on day 6 L-selectin – a carbohydrate binding protein located on trophoblast cells binds to a receptor on epithelium of uterus to initiate attachment Trophoblast sends out projections that invade uterine epithelium and underlying CT between uterine glands and arteries o Uterus is in secretory phase, maintained by progesterone and estrogen from corpus luteum o About 50% of blastocysts fail to implant properly and mother will never know she was pregnant because this will be shed around time of normal menstrual flow o Zygote and abnormal chromosomes usually cause spontaneous abortion Early Development (fertilization to day 16) Cytotrophoblast (inner trophoblast) and syncytiotrophoblast (outer trophoblast) – day 8 o Inner cell mass differentiates into flat bilaminar disc composed of epiblast and hypoblast o Amniotic cavity appears in epiblast Syncytiotrophoblast sends out lacunae o Maternal blood vessels enlarge into sinusoids o Blastocyst cavity enlarges and is lined by hypoblast cells to form primitive yolk sac Day 11-12 – sinusoids and lacunae fuse, forming uteroplacental circulation o Extraembryonic mesoderm forms between the inner surface of the cytotrophoblast and the outer surface of the primitive yolk sac o Chorionic cavity forms within the splanchnic (inner) and somatic (outer) layers of extraembryonic mesoderm, while the primitive yolk sac diminishes in size o Cytotrophoblast cells proliferate to form villi, and hypoblast cells migrate along exocoelomic cavity to form secondary (definitive) yolk sac 2nd week is week of 2’s o Trophoblast differentiates into 2 layers (syncytiotrophoblast and cytotrophoblast) o Inner cell mass forms 2 layers (epiblast and hypoblast) o Extraembryonic mesoderm splits into 2 layers (somatic and splanchnic mesoderm) o 2 cavities form (amniotic cavity and yolk sac) HCG – used for home pregnancy tests, starts showing up in mother around day 6, and level doubles every 48-72 hours Around day 14 – endometrium of the uterus closes over the site where implantation occurred, but this site may occasionally bleed due to the profuse blood supply of the sinusoids and lacunae – can be seen as menstrual flow, since this should be around day 28 of LNMP Embryonic Period (weeks 3-8) HOX genes – regulate anterior-posterior development Gastrulation – formation of 3 germ layers o Epiblast cells migrate through primitive streak (at caudal end of embryo) Cells that do not migrate through this streak are ectoderm Cells migrating through streak to populate hypoblast are endoderm Cells that migrate later than endoderm form mesoderm Mesoderm cells form notochordal plate – detaches from endoderm to form notochord (notochord forms in cranial to caudal direction) Vasculogenesis – blood vessels forming from blood islands – controlled by FGF2 (mesoderm forms hemangioblasts) and VEGF (induces cells to form blood cells in center of island and cells on periphery to form vessels) Angiogenesis – blood vessels sprouting off other blood vessels – regulated by VEGF Primary villus – projection of trophoblast Secondary villus – has core of mesoderm Tertiary villus – has blood vessels Before week 4, embryo gets nutrients by diffusion – after week 4 capillaries extend from embryo, through connecting stalk (future umbilical cord) into villi Neural crest cells – cells from the lateral side of the neural plate, migrate away from the neural tube and form bars of tissue in mesenchyme BMP-4 ventralizes mesoderm to form intermediate and lateral plate mesoderm o Several genes expressed at primitive node block BMP-4 and dorsalize the mesoderm (area with notochord and future somites) o Type of mesoderm that forms depends on how caudal or cranial the cells pass near the primitive node Day 18 – paraxial mesoderm segments to form somitomeres, many of which compact to form somites o Somites begin to form on day 20 and form 3 per day o First occipital and 6 caudal pairs disappear, so 37 pairs total form o Most somitomeres of head do not form somites and contribute to mesenchyme of head Ventral and medial wall form sclerotome (will be axial bone and cartilage) – sclerotome gives rise to cells that invade parietal mesoderm and will become CT of limbs Dorsomedial and ventrolateral cells form myotome – will split to form epaxial (back) and hypaxial (lateral and ventral body wall) muscles o Hypaxial portion of myotome gives rise to cells that will invade parietal mesoderm to form muscles of limbs Dermatome gives rise to dermis of neck, back, lateral trunk, and ventral trunk Intermediate mesoderm forms excretory portions of kidneys and gonads Lateral plate mesoderm splits into parietal (somatic) mesoderm and visceral (splanchnic) mesoderm o Parietal mesoderm gives rise to dermis of body wall and limbs, bones, and CT of limbs and sternum o Visceral mesoderm gives rise to wall around gut tube Cephalocaudal folding of embryo forms 3 divisions of gut tube (foregut, midgut, and hindgut) Lateral folding that closes abdomen obliterates connection between gut tube and yolk sac (except for vitelline duct) o Ectopia cordis – heart outside thoracic cavity o Gastroschisis – part of gut outside abdominal cavity – may have compromised blood flow due to volvulus or may have compromised bowel in general because amniotic fluid doesn’t play well with internal organs Development of Axial Skeleton and Muscle Germ layers that give rise to certain types of muscles o Paraxial mesoderm – skeletal muscle o Visceral layer and lateral plate mesoderm – cardiac muscle, smooth muscle of gut tube o Somatic layer of lateral plate mesoderm and neural crest cells – smooth muscle of blood and lymph vessels o Ectoderm – smooth muscle of mammary glands, sweat glands, dilator pupillae, and sphincter pupillae Development of smooth muscle – uninucleated splanchnic/somatic mesoderm cells elongate to form spindleshaped myoblasts that proliferate but don’t fuse o As proliferation of myoblasts continue, smooth muscle forms sheets or bundles that acquire autonomic innervation Development of Heart o Day 16-18 – splanchnic layer of lateral plate mesoderm forms a horseshoe-shaped cluster of cells rostral to the neural folds (primary heart field) – will become atria, left ventricle, and most of right ventricle o Day 20-21 – splanchnic mesodermal cells ventral to pharynx form secondary heart field that gives rise to rest of right ventricle o Underlying endoderm induces primary and secondary heart fields to become myoblasts o PBX and Hand2 signal myoblasts to become cardiac muscle cells o As they grow, they retain junctions between cell membranes that will eventually form intercalated discs o Purkinje fibers are last myocytes to form Primaxial and abaxial domains separated by lateral somitic frontier (border between dermis derived from dermatomes in back and dermis from lateral plate mesoderm in body wall) o Primaxial – cells around neural tube that receive developmental signals from notochord and neural tube (i.e., bony parts of ribs) o Abaxial – cells of somatic layer of lateral plate mesoderm and cells from somites that have crossed lateral somitic frontier (i.e., costal cartilage) Epaxial and hypaxial – refer to sets of muscles that originate from the dorsomedial portion of the myotome (epaxial) or the ventrolateral portion of the myotome (hypaxial) o Epaxial – dorsal intrinsic muscles innervated by dorsal rami of spinal nerves o Hypaxial – muscles of the lateral and ventral body wall innervated by ventral rami Myf5 and MyoD are MRF proteins important for skeletal muscle differentiation from mesodermal cells o Myf5 makes epaxial muscles (partially activated by SHH) o MyoD makes hypaxial muscles - controlled by Wnt (+) and BMP4 (-) o Wnt – upregulates expression of Myf5 During somite differentiation, developing dermomyotome was divided into dorsomedial and ventrolateral segments o Dorsomedial segment forms the smaller epimere that will develop into the epaxial muscles o Ventrolateral segment forms the larger hypomere that will develop into hypaxial muscles During somite development, myoblasts in myotome fuse to form multinucleate muscle cells Patterns of muscle formation (splitting of dorsal and ventral masses into individual muscles) are directed by connective tissues into which myoblasts migrate Tendons that connect muscle to bone formed from sclerotome Poland sequence – absence of pectoralis minor and part of pectoralis major – hand on opposite side as missing pectoralis minor is usually webbed – nipple and areola misplaced laterally or missing Skeleton development o Neural crest cells – form most of skull o Lateral plate mesoderm – forms appendicular skeleton o Somites – form vertebrae, ribs, and base of skull near occipital Bones that form by endochondral ossification are derived from neural crest and paraxial mesoderm Membranous part of neurocranium formed by intramembranous ossification Posterior fontanelle closes first (1-2 months of age),followed by sphenoid (6 mo), mastoid (6-18 mo) and anterior fontanelle (18 -36 mo) Cranial synostosis – premature closure of sutures; can be attributed to mutations in genes that code for FGF receptors o Scaphocephaly – sagittal suture closes prematurely (long thin head) o Bradycephaly – when coronal suture closes too soon (short wide head) In week 4, sclerotome cells from left and right sides migrate around spinal cord and notochord and unite to form vertebrae o Notochord persists as nucleus pulposus of intervertebral discs Ribs develop from sclerotome cells that grow out of costal processes of thoracic vertebrae Sternum develops from somatic layer of lateral plate mesoderm in ventral body walls o Problem with above leads to pectus excavatum or pectus carinatum Sclerotomes resegment to form vertebrae – intervertebral discs form from mesenchyme between cephalic and caudal parts of original sclerotome Limb Development First evidence of limb buds on day 26, and major features of limbs present by end of 8th week o Forelimbs precede hindlimbs by 1-2 days Initially limb bud formed by core of somatic lateral plate mesoderm covered with ectoderm o Limb bud elongates by proliferation of mesenchyme in proximal-distal direction Lateral plate mesoderm – contributes to bones, blood vessels, and connective tissue Somites – contribute myoblasts that will form muscles Neural tube spinal cord – contributes motor nerve axons for limb innervation Neural crest cells – give rise to sensory nerves, Schwann cells, and pigment cells In 6th week, hand plates form, and in 7th week, foot plates form – also proximal constriction denotes future joint o Mesenchyme in plates condenses and forms digital rays o Proliferation of rays and apoptosis between form digits by end of 8th week Limbs develop from somite numbers that will contain their future dermatomes (C4-T1 for upper limb and L1-S2 for lower limb) Limb muscles appear in 7th week – form from hypomeres of myotomes Chondrification begins in 5th week, and osteogenesis in 7th week – endochondral ossification begins in 12th week In 6th week, limb buds bend at elbow and knee, and in 7th week, elbows rotate 90o to face posteriorly and knees rotate 90o opposite direction to face anteriorly HOX genes crucial to determining limb location on body wall, needed for anterior-posterior positioning o Expressed cranial to caudal and expressed differently depending on limb position o Hand-Foot-Genital Syndrome – mutation in HoxA13 – thumb and big toe are underdeveloped (problem with anterior segments of limb forming) – peraxial problems, not postaxial FGF10 – provides signal for limb bud formation TBX4 makes hindlimb, and TBX5 makes forelimb initiated by HOX9, and they will initiate FGF10 expression o Holt-Oram Syndrome – mutation in TBX 5 gene that causes lack of forelimbs – can be asymmetric and usually is coincident with heart problems FGF10 stimulates ectoderm to produce FGF8, which creates a feedback loop beginning limb development AER needed on tip of limb bud to form distal limb features (has both FGF4 and FGF8) – FGF gradient tells cells how “distal” they are ZPA is on pinky side of limbs and secretes SHH to establish anterior/posterior features according to gradient o TPTPS – overexpression of SHH and duplications of ZPA – have 2 thumbs and webbing in last fingers Wnt-7a secreted by dorsal ectoderm of limb – induces activity of Lmx-1 (HOX gene) that establishes the “dorsal” features o AARRS – rare autosomal recessive linked to mutations in Wnt-7a – phocomelia, absence of ulna and fibula, limb/pelvis aplasia, and other limb malformations o Nail-patella syndrome – mutation in Lmx-1 gene – hypoplastic nails and lack patella in their knees (ventralization of limbs) En-1 (HOX gene) is expressed in ventral ectoderm and establishes ventral features (Courtesy Ron BMP4 and BMP2 responsible for apoptosis that forms individual digits Meromelia – absence of part of a limb o Phocomelia – absence/shortening of proximal limb segments o Hemimelia – absence of anterior or posterior parts of limbs o Acheiria – absence of hands Syndactyly – presence of interdigital webbing Disruption of limb during 4th week produces amelia, and arrest or disturbance in 5th week produces meromelia Development of Spinal Cord Starts to develop around day 19 as neural plate; neurulation – cranial end closes at day 25 and caudal end at day 28 – first fuses around C5 and goes cranial and caudal Following closure, cells rapidly divide forming the neuroepithelial layer Closure of the neural tube results in the neuroepithelial cells giving rise to primitive neurons (neuroblasts) that form a layer “zone” around epithelial layer known as the mantle layer (gray matter) Outermost layers contain nerve fibers (white matter) Thickening of dorsal and ventral area of mantle form alar plate (sensory horn) and basal plate (motor horn) Sulcus limitans divides the neural tube into 2 halves, connected by the roof and floor plates (one alar plate and one basal plate on each side) Axons of basal plates break through marginal zone to become ventral motor root Development of sensory nerves – neural crest cells ride the wave of the closing neural tube; as soon as it closes, they run around and make ganglia, which will send out processes (axons), one to the vertebra (dorsal sensory root) and the other to a body part to innervate During 3rd month, spinal cord extends length of embryo, but vertebral column grows, so dura mater runs all the way down to cover cauda equina and filum terminale SHH and TGF-β form gradients, such that SHH signals ventralization of spinal cord and TGF-β signals dorsalization Rachischisis – when neural tube remains flat sheet (never seals off as a tube) Tethered spinal cord can cause Arnold-Chiari malformation because it can pull the cerebellum down to block off the foramen magnum Development of Brain Prosencephalon – forebrain o Telencephalon – primitive cerebral hemispheres (appear at beginning of 5th week) – develops from pallium - neuroblasts migrate outwards to a sub pial position, then each successive wave of neuroblast migration proceeds subpial, so youngest neurons are on the outside and oldest the inside of the brain Forms CN I 10 weeks – corpus callosum forms Gyri and sulci form because of rapid growth during final stages of fetal period o Diencephalon – characterized by the outgrowth of the optic vesicles – also will form thalamus, hypothalamus, and posterior pituitary (anterior pituitary comes from Rathke’s pouch) Forms CN II Has roof plate (single layer of ependymal cells covered by vascular mesenchyme and gives rise to choroid plexus) and 2 alar plates (separated by hypothalamic sulcus, which divides thalamus from hypothalamus), but no floor or basal plates Mesencephalon – midbrain – consists of colliculi o Basal and alar plates form – basal plates form CN III and CN IV, as well as Edinger-Westphal nuclei that innervate sphincter pupillae – marginal layers of basal plates form crus cerebri – alar plates form superior (coordinates eye movements & reflexes) and inferior (synaptic relay for auditory information) colliculi Rhombencephalon – hindbrain – Pontine flexure deepens, compressing the rhombic lips cephalocaudally forming the cerebellar plate, developing a midline portion (vermis – forms at 12 weeks, separating the cerebellar hemispheres) and 2 lateral portions (cerebellar hemispheres) o Metenecephalon – Goes on to form the pons and cerebellum Basal and alar plates form – basal plates give rise to CN V, CN VI, and CN VII; alar plates give rise to sensory nuclei o Myelencephalon – Goes on to form the medulla oblongata Forms basal and alar plates, similar to spinal cord – basal plates will form CN IX, CN X, and CN XII; alar plates will form CN V and CN VII Choroid plexus (makes CSF) forms on roof plate here HOX genes establish 3 regions of brain SHH establishes midline features – loss or mutation results in holoprosencephaly (cyclopia) Craniorachischisis – failure of neural tube to fuse in cervical region and cranial neuropore – no head whatsoever, just neural tissue sitting on shoulders Most common cause of hydrocephaly is blockage of cerebral aqueduct (aqueduct of Sylvius) Development of Heart Begins in early week 3 – lateral plate mesoderm cells near the rostral end of embryo splits and the intervening space forms the precursor of pericardial cavity – mesoderm near the midline forms a sheet on each side of embryo – blood islands in the center of the sheet form a heart tube on each side of the embryo by vasculogenesis (induced by VEGF) – two heart tubes fuse to form single heart tube Heart is initially cranial to oropharyngeal membrane, but cephalocaudal folding and large growth of brain bring it closer to final position Mesoderm surrounding endocardium differentiates into myocardium, which secretes matrix rich in GAG (hyaluronic acid) called cardiac jelly, which separates endocardium from myocardium and plays important role in valve formation and septation of heart Mesoderm near the sinus venosus (collects venous inflow to that tube – most caudal part of heart tube) migrates to form the outer layer of the heart (epicardium – becomes visceral pericardium) Bulges present in heart tube at end of 3rd week (caudal to cranial – also direction of blood flow) o Sinus venosus collects blood from umbilical veins (from chorion), yolk sac (through pair of vitelline veins), and from embryo via cardinal veins o Primitive atrium o Primitive ventricle o Bulbis cordis – trabeculated portion of right ventricle, conus cordis (outflow tracts of ventricles), and truncus arteriosus (proximal parts of aorta and pulmonary trunk) Fetal circulation consists of embryonic circuit (returned via cardinal veins), vitelline circuit (supplies yolk sac), and placental circuit (umbilical circulation) Fetal heart forms 2 flexures – bulboventricular loop (between bulbis cordis and primitive ventricle) and atrioventricular loop (between ventricle and primitive atria) o Primitive ventricle is moving ventral, caudal and to the right o Primitive atrial region is moving dorsal, cranial and to the left Dextrocardia – heart pushes liver toward midline and no spleen if caused by folding the wrong direction (all organs are inverted so it doesn’t matter if it was caused by situs inversus) Fate of sinus venosus – everything degenerates except right vitelline vein and right cardinal vein o Left horn reduces in size and becomes coronary sinus o Right horn enlarges in size and becomes posterior part of right atrium (sinus venarum) Pulmonary veins begin as single vein coming out of left atrium that bifurcates twice – growth of left atrium encases the original stem and bifurcation Atrioventricular partitioning – mesenchymal cells (endocardial cushions) located between primitive atria and primitive ventricles – superior and inferior cushions merge to form atrioventricular septum (valves) o Mesenchyme surrounding atrioventricular orifices thickens and muscle on ventricular side undergoes apoptosis until only papillary muscle and chordae tendinae connect wall and atrioventricular septum o Complete atrioventricular canal defect – mitral and tricuspid valve form as one large valve that covers both ventricles, thus blood gets shunted left-to-right Septation of atria – septum primum forms with foramen primum (which eventually seals off) – foramen secundum forms by apoptosis in septum primum wall as septum secundum forms – foramen secundum and hole in septum secundum form foramen ovale o After birth, flow through the foramen ovale is stopped by decrease in right atrial pressure (due to occlusion of maternal circulation) and increase in left atrial pressure (due to increase in pulmonary return) – eventually septum primum and septum secundum fuse to form atrial septum o Fix atrial septal defects with Dacron patch or use a piece of the pericardial sac as the septum Septation of ventricle – muscular septum grows up from bottom of ventricles to AV cushions – membranous interventricular septum formed by neural crest tissue (also will separate outflow of aorta and pulmonary arteries) o Neural crest cells make truncal and bulbar ridges, which fuse to form a sheet between aorta and pulmonary trunk, which spirals to place them in final position o Persistent truncus arteriosus (PTA) – one large vessel that splits into aorta and pulmonary trunks and receives blood from both ventricles – most of blood goes out aorta in this case (left ventricle’s blood goes through aorta, and right ventricle’s blood partially goes to aorta due to pressure differences with lack of septum) o Membranous ventricular septal defect – initially left-to-right shunting, but pulmonary hypertension results in proliferation of tunica intima and media in pulmonary arterioles increasing resistance to blood flow; pressure rises in the right ventricle to a point where the blood flow is reversed (“blue kid”) o Tetralogy of Fallot – abnormal neural crest cell migration where aorta is much larger than pulmonary trunk, which has very small diameter Four traits – overriding aorta, pulmonary stenosis, VSD, and right ventricular hypertrophy Cyanotic at birth due to right-to-left shunting SA node is initially located in wall of sinus venosus – incorporated into right atrium when sinus venosus becomes sinus venarum AV node forms from AV canal Heart begins to beat on day 22, and conduction system forms in next few days (autonomic innervation complete at day 30) Development of Arterial Systems Cardiovascular system forms when diffusion no longer is able to meet the metabolic demands of a developing embryo (begins during the third week and heart begins to beat at day 22) Blood cell production shifts from yolk sac (mesoblastic) to liver/spleen (hepatosplenic) to bone marrow (myeloid) throughout development Fetal circulation proceeds placenta umbilical vein ductus venosus (20% actually flows through liver) inferior vena cava (also receives blood from lower limb) right atrium (also receives blood from head and arms from superior vena cava) foramen ovale left atrium (receives small amount of blood from pulmonary system) left ventricle aorta (receives some blood from ductus arteriosus) common iliacs umbilical arteries placenta Degeneration of the distal portion of the 6th arch on right side and the caudal shift of the heart results in asymmetry in the courses of the right and left recurrent laryngeal nerves Double aortic arch – right dorsal aorta never degenerates, so 2 aortic arches – problem because it can squeeze off trachea and esophagus Coarctation of aorta – constriction in aorta – symptoms are hypertension in right arm and hypotension in legs o Classified with regards to ductus arteriosus (preductal or postductal) Vitelline arteries turn into celiac, superior mesenteric, and inferior mesenteric arteries Vitelline vein turns into ligamentum teres hepatis (left) and hepatic portal system (right) Umbilical arteries degenerate into medial umbilical ligaments Development of Lymphatic System Develops 2 weeks later than cardiovascular system as outgrowths of veins At end of embryonic period, 6 lymph sacs are present. (2 jugular, 2 iliac, retroperitoneal, cisterna chyli) Two main channels, right and left thoracic ducts connect jugular sacs with cisterna chili Right and left thoracic ducts form anastomoses – superior part of right duct loses contact with thoracic duct; left thoracic duct degenerates leaving right lymphatic duct and thoracic ducts as the two main lymph ducts Development of Urinary System Urogenital systems form from intermediate mesoderm ridge along posterior wall – both excrete into cloaca 3 different systems form o Pronephros – goes away, doesn’t work – forms in cervical region at beginning of 4th week and goes away by end of 4th week o Mesonephros – might work in early life, but goes away – starts in middle of 4th week – 1st excretory tubules – rapid development causes it to form S shape – tufts form where bends form (on the inside of the bends) that will become glomerulus Bowman’s capsules form around glomeruli Longitudinal collecting duct (Wolffian duct) forms While caudal tube are still differentiating, at cranial end, tube and glomerulus show signs of degeneration, and by end of 2nd month, majority of tube disappears entirely Few caudal aspects of tube remains in male (participate in genital system formation), but completely disappear in female o Metanephros – this is final form that will work later – appears in 5th week from metanephric mesoderm Bud penetrates metanephric tissue and dilates to form primitive renal pelvis – gives rise to calyces, ureter, and all collecting tubes Nephrons begin forming and will continue to until birth – once born, no new nephrons Urine production begins in 10th week Gene regulation factors o WT-1 regulates production of GDNF and HGF, stimulating branching of uteric bud Ret is receptor for GDNF and MET is receptor for HGF o FGF2 and BMP7 – synthesis is induced via the buds and are strong survival genes (no apoptosis) o Without Wnt9b upregulating PAX2, there is no tubule formation – PAX2 promotes condensation of mesenchyme o Without Wnt6, there is no epithelium – Wnt6 causes upregulation of Wnt4, which causes mesenchyme to epithelialize and form tubules o ECM modified to replace collagen I and III with collagen IV and laminin Kidney originally forms in pelvis and begins ascent due to diminishing body curvature – becomes completely functional at 12 weeks During weeks 4-7 cloaca divides into anal canal and urogenital sinus o During differentiation of the cloaca, caudal portion of mesonephric ducts absorbed into walls of bladder Bladder continuous with the allantois, however when lumen of allantois is obliterated, thick fibrous cord urachus connects the bladder apex to the umbilical cord (adult median umbilical ligament) In males the mesonephric ducts move closer (during ascent) and enter the prostatic urethra becoming the ejaculatory ducts Wilms’ Tumor – Mutation in WT1 gene, resulting in kidney cancer by age 5 WAGR Syndrome – Microdeletion on chromosome 11 involving WT1 and Pax6 genes. Results in a Wilms’ tumor, Aniridia (Lack of an Iris), Gonadoblastoma, Retardation Multicystic dysplastic kidney – Failure of nephron to develop, failure of ureteric bud to branch, can cause renal agenesis. GDNF mutation Autosomal recessive polycystic kidney disease (ARPKD) – 1/5,000 births, progressive cyst forming disease kidneys become large renal failure occurs in childhood/infancy Genital System Formation Pair of longitudinal gonadal ridges form from epithelium and mesenchyme in posterior abdominal cavity in week 5 – epithelium proliferates to form primitive sex cords Germ cells arise from epiblast in Wk. 2, migrate to the yolk sac (Wk 3), migrate through dorsal mesentery of the hindgut (Wk 5) arriving at genital ridges in week 6 – if germ cells never reach the ridges, gonads will not form SRY gene on Y chromosome produces SOX9, which blocks WNT4, which would produce female hormones – at the same time WNT4 produces DAX1, which blocks SOX9 in females Male gonad formation and differentiation o Under the influence of SRY, primitive sex cord proliferate and penetrate medulla to form medullary cords (no cortex), which form a network (rete testes) at the hilum o Tunica albuginea separates cords from surface epithelium (solid until puberty) o Leydig cells form from mesenchyme shortly after differentiation of the cords and begin to secrete testosterone essential for differentiation of genital ducts and external genitalia at week 8 o Sertoli cells derived from surface epithelium and populate cords at 16 weeks o By week 26, the testes have descended from the lumbar region to the deep inguinal ring o Testes follow the processus vaginalis (inguinal canal), an evagination of peritoneum, out of the abdomen o Cryptorchidism – undescended testis – must be corrected surgically if it does not descend by 1 year of age or it could become cancerous Initially males and females have 2 pairs of ducts: mesonephric (wolffian) and paramesonephric (müllerian) ducts o In men, wolffian ducts persist and müllerian ducts degenerate (remnant forms prostatic utricle) o In women, müllerian ducts persist and wolffian ducts degenerate Female gonad formation and differentiation o Primitive sex cords degenerate and are replaced by CT that forms medulla of ovary o Surface epithelium continues to proliferate to form cortical cords o In 3rd month, cortical cords split into clusters of cells (future follicular cells) that surround germ cells that migrated into ovary o Müllerian ducts proliferate under the influence of estrogen to form uterine (fallopian) tubes, uterus and upper portion of vagina o Ovaries descend to just superior to rim of pelvis o Gubernaculum is attached to uterus, where it becomes ovarian ligament and round ligament of uterus o Vagina forms from evagination of urogenital sinus, which forms a urogenital plate, and lumen is made by vacuolization of this (hymen is remnant of urogenital plate) o Uterus didelphys – 2 uterus halves with 2 vaginas o Uterus arcuatus – indentation of fundus of uterus (barely a difference from normal) o Uterus bicornis – 2 uterus halves with 1 vagina o Uterus bicornis unicollis – 2 uterus halves with 1 vagina, but one half is blind-ended pouch Cloaca folds – fuse cranially to form genital tubercle which will become phallus o Becomes glans clitoris, corpora cavernosus of the clitoris, and vestibular bulbs in females o Becomes glans penis, corpora cavernosa, and corpus spongiosum in males Cloacal folds partitioned into urethral and anal folds o Urethral folds become labia minora in females o Urethral folds become ventral aspect of penis in males Labioscrotal (genital) swellings form lateral to urethral fold o Becomes labia majora and mons pubis in females o Becomes scrotum in males Development of Respiratory System Septum transversum – thick plate of mesoderm occupies space between thoracic cavity and yolk sac (still allows communication between thorax and abdomen via pericardioperitoneal canals – forms around C3-C5 somites o Lung growth occurs so rapidly, they grow into the mesenchyme of the body wall – this growth splits the mesoderm of the body wall into two components. Mesoderm of body wall splits into definitive wall of thorax and pleuropericardial membranes which form both common cardinal veins and the phrenic nerves Positional changes in heart and sinus venosus shift cardinal veins towards midline, drawing pleuropericardial membranes out in mesentery-like fashion – they then fuse with each other and with root of lungs, dividing thoracic cavity into definitive pericardial and 2 pleural cavities o Pleuropericardial membranes form with fibrous pericardium o While formation of the pleural cavities isolates the pericardial cavity, the two pleural cavities are still in communication with the abdominal cavity via the pericardio-peritoneal canals – closed by crescent fold of tissue (pleuroperitoneal folds) that grow medially and ventrally, so that by 7th week, they fuse with mesentery of esophagus and septum transversum o Once rim is established, myoblasts originating from cervical somites (C3-C5) penetrate membranes and grow to form muscular portion of diaphragm (formation of the muscular ridge signals somites to send down nerves) o Septum transversum stays as central ligament, and mesentery of esophagus forms crura Diaphragmatic hernias – formed by failure of pleuroperitoneal folds to completely close pericardioperitoneal canals – usually on left side, compressing heart and lungs About 4 weeks, lung bud develops o Retinoic acid produced by adjacent mesoderm upregulates expression of TBX4, which induces formation of lung bud o Cartilagenous, muscular, and CT components of trachea are derived from splanchnic mesoderm o Trachesophageal ridges fuse to form septum separating trachea and esophagus Laryngeal epithelium proliferates so much, lumen occluded; subsequent vacuolization and recanalization forms laryngeal ventricles, which then split into true and false vocal cords During 5th week, lung buds form bronchiole buds (3 on right and 2 on left) o Continued growth expands lung buds into body cavity into pericardioperitoneal canals o Bronchi continue branching until the 7th month (regulated by epithelial-mesenchyme interactions between the endoderm of the lung buds and splanchnic mesoderm surrounding them ) – branching signals include FGF family Mesoderm on the outer surface of lungs will become visceral pleura, and somatic mesoderm covering inside of body wall will become parietal pleura Prior to birth, lungs filled with Cl- rich fluid, little protein, and some mucus produced by bronchial glands, and some surfactant. During final 2 weeks of prenatal life, concentration of surfactant protein increases. As surfactant levels rise (usually during the 34th week), it enters amniotic fluid and acts on macrophages in amniotic cavity; once these “activated” macrophages move across chorion into uterus and produce interluken-1 (IL-1), prostaglandins upregulated, which in turn leads to uterine contractions (mechanism to tell when bun is done?) Most fluid in lungs absorbed via vascular and lymph systems, leaving layer of surfactant deposited on alveoli VACTERL – association of these defects (Vertebral anomalies, Anal atresia, Cardiac defects, TracheoEsophageal atresia/fistula, Renal anomalies, Limb defects) Development of Digestive System Gut tube is 4-layered in cross-section: innermost lining (epithelium) derived from endoderm, remainder of wall (lamina propria to adventitia/serosa) forms from visceral lateral plate mesoderm, and its innervation is derived from ectoderm (neural tube and neural crest) Primitive gut forms from yolk sac to form tube lined by endoderm; remainder of endoderm-lined cavity (yolk sac and allantois) remain extraembryonic o Controlled by gradient of retinoic acid (high in cloaca, very low in pharynx) o Endoderm of gut tube expresses SHH, which causes expression of Hox genes in mesoderm of different regions of gut to specify region (stomach, duodenum, etc.) o Mesoderm directs the development of the endodermal lining for the region (stratified squamous, simple columnar, etc.) Lateral folding closes off ventral aspect of body – cranial to umbilicus there is both dorsal and ventral mesentery; caudal to umbilicus, there is only dorsal mesentery Foregut dilates to form stomach during week 4 o Stomach rotates 90o clockwise around vertical axis such that dorsal part (greater curvature) winds up on left side and ventral surface (lesser curvature) winds up on right side – left vagus n. is dragged along with left side of stomach so that it now innervates the anterior surface, and right vagus nerve is dragged to innervate posterior surface. o Stomach also rotates approx. 45o in coronal plane moving pylorus anterior and right o Stomach is attached to the dorsal and ventral body walls by mesenteries, so when stomach rotates, it forms omental bursa Week 5, mesodermal cells between 2 layers of dorsal mesogastrium differentiate to form spleen Note that liver, stomach and spleen are intraperitoneal (suspended by mesenteries), kidneys and aorta are retroperitoneal, and pancreas is secondarily retroperitoneal As stomach rotates around anterior-posterior axis, dorsal mesogastrium (dorsal mesentery) grows down and forms double layer sac (greater omentum) o Ventral mesogastrium becomes lesser omentum and falciform ligament Duodenum, liver, and pancreas rotate as a unit following stomach (90o around a longitudinal axis) o Biliary emesis (green vomit) by a newborn is a sign of either duodenal atresia after major papilla or strangulation of small intestine – serious problem (deal with it NAO!!) – happens because bile can’t continue down, so it builds up until it reaches stomach – once it reaches stomach, it induces vomiting Liver bud forms during week 3 as outgrowth of foregut called hepatic diverticulum o Gall bladder, its duct, and ventral bud of pancreas form as outpocketing of hepatic diverticulum o o Vitelline and umbilical veins give rise to the hepatic sinusoids, and mesoderm gives rise to CT All foregut cells have the potential to become liver cells, but ectoderm, mesoderm and notochord suppress expression of liver-specific genes – FGF2 suppresses the suppression, and BMP enhances ability of foregut to react to FGF2 Pancreas forms from ventral (off of gallbladder/hepatic bud) and dorsal bud (off of duodenum) – ventral bud will swing around dorsally to fuse with dorsal bud and become uncinate process of pancreas o Main pancreatic duct derived from distal portion of dorsal bud duct fusing with duct of ventral bud, whereas accessory duct may form in 10% of people from proximal portion of duct of dorsal bud o Pancreas forms because of HOX gene (PDX) being upregulated o Islets of Langerhans are specified by PAX4 and PAX6 (HOX genes) Wk. 6, midgut exists as single loop that projects out into umbilical cord (physiological umbilical herniation) and rotates 90o counterclockwise around axis of superior mesenteric a. – midgut continues to lengthen, and ileum and jejunum coil o During 10th week, intestinal loops return to abdominal cavity and rotate an additional 180o (to fan out or spread SMA to avoid strangulation of artery) Omphalocele – herniation of intestines never returns to abdominal cavity and remains in umbilical cord – may have compromised blood supply due to volvulus o Cecum begins to form during 6th week, and appendix forms after intestines return to abdominal cavity – this is initially in upper right quadrant of abdomen o Ligament of Treitz – suspensory ligament (skeletal and smooth muscle component) that connects duodenum to diaphragm – if midgut malrotates, this can become wrapped around intestine and strangulate that section Hindgut – blind sac that terminates at cloacal membrane – allantois enters anterior portion of hindgut as urogenital sinus; layer of mesoderm (urorectal septum) forms separating urogenital sinus (future bladder) from hindgut; invagination of ectoderm merges with endoderm of hindgut to form anal canal (merging forms pectinate line) o Imperforate anus – cloacal membrane does not breakdown resulting in failure of fusion of superior (hindgut) and inferior (ectodermal invagination) parts of anal canal