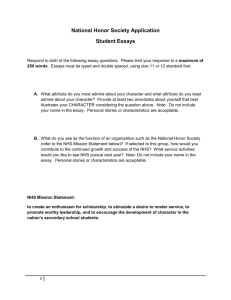
NHS England Summer communication pack
advertisement

North SUMMER HEALTH, SELF CARE AND NHS SERVICES Communications pack 1. 2. 3. 4. 5. 6. 7. Context Target audiences Key overall messages Key messages for parents News releases Other communications channels Appendices 1. Context Peaks in NHS activity during the summer months are seen to be linked with people experiencing a variety of seasonal ailments, such as sunstroke, allergies, minor injuries and food poisoning and an increased number of children attending A&E. This summer communications information pack has been developed as a resource to provide themes, facts and statistics, key messages and information to use with stakeholders, partners and local media. The aim is to provide coordination and consistency in messages about key summer health issues and NHS services. 2. Target audiences While it would be of benefit for all age groups and demographics to be aware of the summer health messages, we would particularly like to target: Parents of school age children People going on holiday Young adults. 3. Key overall messages North It’s much quicker and pretty straightforward to look after yourself if you have a common complaint, such as upset stomach, sunburn, bite or sting or a minor injury such as a cut or sprain. Visit a local pharmacist for confidential advice and treatment to put you on the fast track to feeling better, there’s no need for a prescription or unnecessary A&E wait. Accident and emergency is for life threatening injuries and serious, immediate health problems. These include major loss of blood, chest pain, stroke, severe abdominal pain, broken bones, breathing problems, serious eye injuries. For most people, common complaints such as an upset stomach, sprains, strains and aches, sore throats and colds will start to clear up within a few days to a couple of weeks. There are a number of NHS services you can use to treat less serious injuries and illnesses. To find your nearest service and get further advice call NHS 111 or visit www.nhs.uk 4. Key messages for parents Having an ill child can be a scary experience, but often the best person to help your child quickly is you. Understanding more about common childhood illnesses and injuries can help you feel more confident in knowing what to do. Further information is available at www.nhs.uk Parents often get worried about temperatures, coughs and minor injuries, such as sprains and cuts. But with some advice from your pharmacist and the use of some stock medicines and first aid kit, you can often manage to make your child feel better at home. 5. News releases It is assumed that other NHS organisations, local authorities and other partners would prefer to produce their own news releases in line with lead responsibilities and local knowledge/need. To assist with this, facts, stats and articles about common summer ailments are provided in appendix C. North 6. Other communications channels Content for websites/intranets/newsletters Themed content / articles in appendix A include: Sunburn and heat exhaustion Confident care from mum and dad Don’t let allergies take the spring out of your step Passports and paracetamol Summer health Parenting websites A number of sites offer localised content depending on user preference and location. All feature discussion forums/threads, local advertising and sponsorship opportunities and would be useful for sharing information about self care, sun care, use of services and allergies. The most widely used sites include: www.parentdish.co.uk www.netmums.com www.mumsnet.com Social media Themed messages for social media, including Twitter, are included in appendix B The messages can be localised where appropriate or necessary and partner organisations can be encouraged to retweet and use the same hashtag. North APPENDIX A – COPY FOR WEB/INTRANET OR NEWSLETTERS 1. CONFIDENT CARE FROM MUM AND DAD Having an ill child or dealing with a minor injury can be daunting, but parents are often in the best position to help their child get better quickly. Understanding more about common childhood injuries or illnesses can help you decide what to do. High temperature High temperature is a normal response to fight a virus or infection or to cool the body down and does not harm your child. Children with a persistent high temperature (40c or above) who have other symptoms – see below – could have a more serious infection but most will not. You can usually lower your child’s temperature using paracetamol and / or ibuprofen and removing some of their clothing. Sponging with cool water can make children shiver, which can actually raise their temperature. However, sponging with lukewarm water may help. Cuts and gashes Children are always playing and exploring, and getting cuts and scrapes. If there’s a lot of bleeding, press firmly on the wound with a clean cloth, such as a tea towel or flannel. If you don’t have one, use your fingers. Press until the bleeding stops – may be 10 minutes or more. If possible, raise the injured limb to help stop the bleeding. (Not if you think the limb might be broken, in which case seek medical help). Cover the wound with a clean dressing. If blood soaks through, leave the dressing there and put another over the top. It’s very unusual for a wound to cause serious blood loss. But if the cut keeps bleeding, or there’s a gap between the edges of the wound, take your child to accident and emergency or a minor injury unit. If there is a possibility of a foreign body (e.g. a piece of glass) in the cut, go straight to A&E. Sprains and strains These are very common injuries, especially during physical games and sports. A sprain is when ligaments have been stretched, twisted or torn and often happens in the knees, ankles, wrists and thumbs. Symptoms can include tenderness/pain, being unable to use the joint normally or put weight on it, swelling and bruising. North Strains are when muscles stretch or tear and are common in the legs and back. Symptoms can include pain, swelling, bruising, spasms and temporary loss of function in the affected muscle. Generally, a sprained joint should be moved as soon as it is not too painful, whereas a strained muscle should ideally be kept still for a few days. Most sprains and strains can be cared for at home using PRICE therapy (protection, rest, ice, compression and elevation). Painkillers, such as paracetamol, can help and the affected body part will usually be back to normal within a few weeks. You should take your child for medical advice if the pain is very severe, they cannot put any weight on the injured area, it gives way when they try to use it, the injury looks crooked/has unusual lumps or bumps (other than swelling) or there is numbness or coldness in any part of the area. Sickness and diarrhoea Sickness and diarrhoea are common in school age children. Diarrhoea usually lasts for five to seven days, and for most children it will stop within two weeks. Vomiting often lasts for one to two days, and in most children it will stop within three days. Ask your pharmacist or GP for advice if your child is taking longer to get better. To stop dehydration, give your child plenty of clear drinks (such as water or clear broth). Avoid fruit juice or squash, which can make things worse. Only give your child food if they want it. Don't give anti-diarrhoeal drugs, as they can be dangerous. Oral rehydration treatment from your pharmacist can help. Help to prevent germs spreading by using separate towels for your child and reminding everyone in the family to wash their hands after using the toilet and before eating. Don't return your child to their school or childcare until at least 48 hours after the last episode of diarrhoea or vomiting. Insect bites and stings Bites and stings are normally harmless and usually only cause minor irritation by becoming red, swollen and itchy for a few days. North You can easily treat them by washing the area with soap and water and placing a cold compress (a flannel or cloth soaked in cold water) over to reduce swelling. Tell your child to avoid scratching to reduce the chance of infection. If they are in pain, or the area is swollen, use paracetamol or ibuprofen. See a GP if there's a lot of swelling and blistering of the area or if there's pus, which indicates an infection. In rare cases, some people can have a serious allergic reaction (anaphylaxis) to a bite or sting. Dial 999 for an ambulance if your child experiences : difficulty breathing or swallowing nausea, vomiting or diarrhoea dizziness or feeling faint confusion, anxiety or agitation. Coughs and colds Colds are very common - normal, healthy children can have eight or more colds a year. Young children often develop a chesty cough because they have smaller airways. This can be worrying but is often not a chest infection - a child with an infection will generally be more unwell. Colds normally last 7-14 days and are not helped by antibiotics - green discharge from the nose (snot/phlegm) does not indicate an infection. While coughing can be irritating and take a while to go, cough syrups probably do not help and antibiotics aren’t needed. Keep your child’s throat lubricated and their body hydrated with regular drinks of water and encourage them to rest. Burns and scalds Immediately place the area under cold running water to take the heat out of the skin. Don't do this for longer than 10 minutes, as babies and toddlers can get too cold. If there’s no running water, immerse the burn or scald in cold water or any other cool fluid, such as milk or a cold drink. Use something clean and non-fluffy, like a cotton pillowcase or clingfilm, to cover the burn or scald and reduce the danger of infection. If your child’s clothes are stuck to the skin, don’t try to take them off. If the burn is not calmed by the above actions, don’t put any ointments or creams on, as it will have to be cleaned off before the area can be treated. Depending on how severe it is, see your GP or go to a minor injuries unit or accident and emergency department. North Blisters will burst naturally. The raw area underneath needs a protective dressing. Ask your pharmacist or practice nurse for advice. In all cases, if you are still worried about your child after caring for them at home, get further advice from your GP surgery or by calling NHS 111. In an emergency situation, dial 999 for an ambulance. Signs of possible serious illness: Your child is very drowsy or irritable and doesn’t improve after taking paracetamol or ibuprofen. Your child has problems breathing – e.g. rapid breaths, short of breath or ’working hard’ to breathe (which sometimes looks as though the skin below the ribs gets sucked in when they inhale). Cold or discoloured hands or feet with a warm body. Unusual skin colour (pale or blue around lips) Persistent high temperature (40c or above) which does not come down with treatment. An infant who is not feeding or any child showing signs of dehydration. 2. SUNBURN AND HEAT EXHAUSTION Most of us enjoy spending time in the sun and but, despite the advice, it still seems Brits can still be prone to overdoing exposure to the sun’s rays. It’s easy to underestimate your time to the sun and not realise you’re getting burnt. While sunburn is usually short-lived and mild, it's important to avoid because it can increase the chances of developing skin cancer in later life. The first thing to do if you or your child has sunburn, is to get out of direct sunlight as soon as possible. Cool skin by sponging it with cool water or by having a cool bath or shower – applying a cold compress to the affected area may also help. Drink plenty of fluids to bring temperature down and prevent dehydration. Apply a water-based cream, emollient or petroleum jelly (such as Vaseline) to keep skin cool and moist. If necessary, take painkillers such as ibuprofen or paracetamol. Try to avoid all sunlight, including through windows, by covering up the affected areas of skin until your skin has fully healed. North You should contact your GP or call NHS 111 for advice if: the sunburn is over a large area there is blistering or swelling of the skin you have chills or a high temperature of 38C or above, or 37.5C or above in children under five. there are symptoms of dizziness, headaches and feeling sick (possible heat exhaustion). Heat exhaustion and heatstroke Heat exhaustion causes extreme tiredness as a result of a decrease in blood pressure and blood volume. It's caused by a loss of body fluids after being exposed to heat for a prolonged period of time. Someone with heat exhaustion will feel sick, faint and sweat heavily. They should go immediately to a cool place and drink plenty of water. Remove excess clothing and you should start to feel better within half an hour with no long-term complications. Heatstroke Heatstroke is a more serious condition than heat exhaustion and occurs when the body's temperature becomes dangerously high. The body is no longer able to cool itself and starts to overheat. Groups more at risk of developing heatstroke are: children under two very elderly people people with kidney, heart or circulation problems people with diabetes. Signs of heatstroke include dry skin, vertigo, confusion, headache, thirst, nausea, rapid shallow breathing (hyperventilation) and muscle cramps. Suspected heatstroke should always be regarded as an emergency, and you should dial 999 to request an ambulance. While waiting for the ambulance you should: immediately move the person to a cool area increase ventilation by opening windows or using a fan give water to drink (if the person is conscious), but don't give them medication such as aspirin or paracetamol North shower skin with cool, but not cold, water (15-18°C); alternatively, cover their body with cool, damp towels or sheets. Left untreated, heatstroke can lead to complications, such as brain damage and organ failure. It's also possible to die from heatstroke. There are steps you can take to reduce the risk of getting heat exhaustion and heatstroke: stay out of hot sun, particularly between 11am and 3pm walk in the shade, apply sunscreen and wear a hat avoid extreme physical exertion have plenty of cold drinks, but avoid caffeine and alcohol eat cold foods, particularly salads and fruit with a high water content take a cool shower, bath or body wash sprinkle water over your skin or clothing, or keep a damp cloth on the back of your neck. 3. PASSPORT AND PARACETAMOL? Going on holiday is exciting, with lots of things to plan, but taking certain essential items can help maximise your time in the sun. It may not be top of your planning list alongside passport and tickets, but a visit your local pharmacy before heading off either home or abroad should feature in your preparations. Firstly, talk to your local pharmacist if you are on medication for a condition such as asthma, diabetes or a heart problem, to find out if you need a repeat prescription to take with you. Secondly, put together a basic first aid kit to deal with any minor health issues while you’re away. Again your pharmacy can help with that. Putting these two things on your holiday ‘to do’ list will avoid unnecessary worries or time spent buying medicines or other first-aid supplies whilst you’re away. The last thing you want to be doing while you’re on holiday is searching around for painkillers, antihistamines or plasters. A basic first aid kit will help with minor ailments, such as stomach upsets, allergies, headaches, sunburn, insect bites, aches and sprains and strains. The really useful interactive first aid kit guide at www.nhs.uk can help ensure you have everything you need, or talk to your local pharmacy for advice. North If you’re travelling in Europe be sure to take a European Health Insurance Card (EHIC), available free at https://www.ehic.org.uk . It will enable you to access stateprovided healthcare across most of Europe at a reduced cost, or sometimes for free. It will also cover treatment until you return to the UK. Before going abroad, be sure to check the rules about the types and quantities of medicines you are allowed to take. Some medicines available over the counter in the UK may be controlled in other countries and vice versa. 4. DON’T LET ALLERGIES TAKE THE SPRING OUT OF YOUR STEP Spring and summer are the time of year when allergies such as asthma, eczema and hay fever can get much worse, with symptoms including sneezing, coughing, skin rashes and shortness of breath. But there’s no need to get bogged down by runny noses, itchy eyes, irritated skin and tickly throats. Allergy sufferers can prepare for the spring and summer months by getting the medicines they need from their local pharmacist – who can also offer expert advice to help people manage their health during warmer months. If symptoms persist, despite the use of over-the-counter medicines, you should get in touch with your GP who may then offer tests to identify the cause. For more information about hay fever and allergies, visit http://www.nhs.uk/ 5. WE ALL LIKE A SUNNY DAY… And the opportunities that nice weather brings for activities, outdoor living, fresh air and fun. When thinking about laid back, sunny days it’s easy to switch off to messages about health risks but there’s a real chance that you or someone you know could be negatively affected by the heat. Children and babies, older people and those with long term health conditions – especially heart and breathing problems - are particularly at risk. Hot days and warm nights can have a significant effect on health. Main risks are: dehydration overheating, which can make symptoms worse for people who already have problems with their heart or breathing heat exhaustion and heat stroke North sunburn. Knowing how to keep cool and manage health conditions during hot weather can save lives. Most likely to be affected are: older people, especially over 75 babies and young children people with a serious condition, especially heart or breathing problems people with mobility problems, e.g. people with Parkinson's disease or who have had a stroke people on certain medications, including those that affect sweating and temperature control people who misuse alcohol or drugs people who are physically active – at work or leisure. To stay cool and reduce health risks: Stay out of direct sunlight between 11am and 3pm (hottest part of the day). Always use a sunscreen with a high protection factor. Have cool baths or showers or splash yourself with cool water. Placing your wrists under cool running water can help. Drink cold drinks regularly, such as water and fruit juice. Avoid tea, coffee and alcohol. Wear loose, cool clothing and a hat outdoors. Check up on friends, relatives and neighbours who may be less able to look after themselves. If someone feels unwell, get them somewhere cool to rest and give plenty of water to drink. Seek medical help if symptoms such as breathlessness, chest pain, confusion, weakness or dizziness don't go away. More information is available at www.nhs.uk and you can call NHS 111 24/7 for further advice. North APPENDIX B – SOCIAL MEDIA MESSAGES AND TWEETS Please shorten links via Bit.ly before using. Hay fever It is estimated that more than *10 million people in the UK suffer from hay fever – don’t suffer unnecessarily. Your local pharmacist can give you fast, free, expert help and advice. You can find more information on hay fever at http://www.nhs.uk/conditions/hayfever/Pages/Introduction.aspx Is pollen causing you pain? Your local pharmacy can help ease the symptoms with expert advice and a range of over-the-counter remedies, without the need to book an appointment. You can find information on how to treat hay fever at http://www.nhs.uk/Conditions/Hay-fever/Pages/Treatment.aspx Hay fever can make asthma worse and leave you feeling really poorly. Talk to your local pharmacist about how antihistamines can prevent an allergic reaction before it even starts. You can find more information on hay fever at http://www.nhs.uk/Conditions/Hayfever/Pages/Symptoms.aspx Think you have hay fever? You don’t need a diagnosis from your GP. Get fast, free, expert help and advice from your local pharmacy. You can find more advice on hay fever at http://www.nhs.uk/conditions/hay-fever/Pages/Introduction.aspx Struggling with hay fever this summer? Visit your local pharmacy for help. You can find more information on hay fever http://www.nhs.uk/conditions/hay-fever/Pages/Introduction.aspx Hay fever tweets Suffer from #hayfever? Your pharmacist can give you fast, free, expert help & advice. More advice and #summerhealth info at http://www.nhs.uk/conditions/hay-fever/Pages/Introduction.aspx #hayfever Is pollen a pain? Your local pharmacy can help ease symptoms #summerhealth with advice on over-the-counter remedies #hayfever #summerhealth #hayfever can make #asthma worse. Talk to your pharmacist about how antihistamines can prevent allergic reactions. Think you have #hayfever? Don't see your GP. Get fast, free, expert advice from your pharmacist. More at http://www.nhs.uk/conditions/hay-fever/Pages/Introduction.aspx Red eyes & runny nose for summer parties? Stop #hayfever by visiting your pharmacy or going online for advice http://www.nhs.uk/conditions/hay-fever/Pages/Introduction.aspx Sprains and Make sure you warm up properly before exercising to avoid sprains North strains and strains this summer. Find out more at http://www.nhs.uk/Livewell/fitness/Pages/how-to-warm-up.aspx Over done it in the gym? For advice on dealing with those aches and pains why not visit http://www.nhs.uk/Conditions/Sprains/Pages/Introduction.aspx Trying to get fit for your holiday? Make sure you warm up properly before exercising to avoid sprains and strains this summer. Find out more at http://www.nhs.uk/Livewell/fitness/Pages/how-to-warmup.aspx Got those trainers on, ready to get fit for the summer? Why not find out first how to avoid sprains and strains. Visit http://www.nhs.uk/Livewell/fitness/Pages/how-to-warm-up.aspx Been inspired by Wimbledon? Make sure you warm up properly before playing sports to avoid sprains and strains this summer. Find out more at http://www.nhs.uk/Livewell/fitness/Pages/how-to-warmup.aspx Hitting the gym, tennis courts, football pitch, or streets this summer? Make sure you warm up and warm down properly to avoid sprains and strains this summer. Find out more at http://www.nhs.uk/Conditions/Sprains/Pages/Prevention.aspx Minor sprains and strains can usually be treated with self-care techniques, such as PRICE therapy (protection, rest, ice, compression and elevation). Find out more about PRICE therapy at http://www.nhs.uk/Conditions/Sprains/Pages/Introduction.aspx Sprains and strains tweets Make sure you warm up before exercise to avoid a #sportinginjury. Find out more about #sprainsandstrains at http://www.nhs.uk/Livewell/fitness/Pages/how-to-warm-up.aspx #sprainsandstrains Over done it a bit in the gym? For advice on dealing with #sportinginjury #sprainsandstrains or #sportinginjury visit http://www.nhs.uk/Conditions/Sprains/Pages/Introduction.aspx Want to get fit for holiday? Make sure you warm up before exercising to avoid #sprainsandstrains this summer http://www.nhs.uk/Livewell/fitness/Pages/how-to-warm-up.aspx Jumpers for goal posts? Overdone the footie in the park? For advice on dealing with #sportinginjury #sprainsandstrains visit http://www.nhs.uk/Conditions/Sprains/Pages/Treatment.aspx Inspired by #Wimbledon? Make sure you warm up before playing sport to avoid #sprainsandstrains http://www.nhs.uk/Livewell/fitness/Pages/how-to-warm-up.aspx North Minor #sprainsandstrains can usually be treated with self-care techniques, such as PRICE therapy. Find out more at http://www.nhs.uk/Conditions/Sprains/Pages/Introduction.aspx Sprained ankle? Pulled muscle? If you have a #sportinginjury, visit http://www.nhs.uk/conditions/sprains/pages/introduction.aspx for advice Bites and Stings Have you been stung this summer? Follow some basic tips to help improve symptoms - http://www.nhs.uk/conditions/bitesinsect/pages/introduction.aspx Don’t scratch it. Most insect bites and stings are harmless and will heal after a few days. Find out more about how to treat a bite or sting - http://www.nhs.uk/conditions/bitesinsect/pages/introduction.aspx Beware of stings and bites by the barbeque. Make sure you have a full first aid kit on standby http://www.nhs.uk/tools/pages/firstaidtoolkit.aspx If you’ve ever been stung when you’re out and about, you’ll know it’s not much fun. Find out how to treat symptoms http://www.nhs.uk/conditions/bites-insect/pages/introduction.aspx Want to prevent stings and bites when you’re out and about? There are a number of precautions you can take. To find out more visit http://www.nhs.uk/Conditions/Bites-insect/Pages/Prevention.aspx Bites and stings tweets Been landed with a #bite or #sting this summer? Follow some basic tips to help symptoms at http://www.nhs.uk/conditions/bitesinsect/pages/introduction.aspx For most people an insect #bite or #sting is harmless & will heal in a few days. See how to treat them here http://www.nhs.uk/conditions/bites-insect/pages/introduction.aspx To treat a #bite or #sting have a first aid kit on standby – find out more at http://www.nhs.uk/tools/pages/firstaidtoolkit.aspx Taking antihistamine and using a cold compress can reduce swelling and itching of a #bite or #sting. http://www.nhs.uk/tools/pages/firstaidtoolkit.aspx Want to prevent a #bite or #sting when you’re out & about? There are a number of things you can do http://www.nhs.uk/Conditions/Bites-insect/Pages/Prevention.aspx #bite #sting Summer health advice Don’t let food poisoning ruin your summer holiday. In most cases, you can treat yourself without seeking medical advice by taking the following self-care advice http://www.nhs.uk/Conditions/Food- North poisoning/Pages/Treatment.aspx All ready for the summer holidays? Don’t forget your first aid kit. Find out what you need here http://www.nhs.uk/tools/pages/firstaidtoolkit.aspx Going abroad this summer? Be prepared…Find out what travel health essentials you need to stay safe and healthy abroad http://www.nhs.uk/Livewell/travelhealth/Pages/Travelhealthkit.aspx So you’re all packed for your summer holiday but have you packed your travel health essentials? Find out what you need here http://www.nhs.uk/Livewell/travelhealth/Pages/Travelhealthkit.aspx Got a summer bug and don’t know what to do? Don’t go to your GP, find out how you can self-care at home http://www.nhs.uk/conditions/vomitingadults/pages/introduction.aspx If you’re going abroad this summer, don’t forget that travelling with some basic medicine cabinet essentials can save you a lot of holiday heartache http://www.nhs.uk/tools/pages/firstaidtoolkit.aspx If you’re looking forward to a holiday away with the family, make sure you’re prepared with your travel health essentials http://www.nhs.uk/Livewell/travelhealth/Pages/Travelhealthkit.aspx Summer health advice tweets Spent too much time in the sun? Stay in the shade, drink water and apply aftersun #summerholiday #sunburn All ready for your #summerholiday? Don’t forget your first aid kit. #summerholiday http://www.nhs.uk/tools/pages/firstaidtoolkit.aspx Find out about the travel health essentials you need to stay safe & healthy on your #summerholiday http://www.nhs.uk/Livewell/travelhealth/Pages/Travelhealthkit.aspx Passport, tickets, paracetamol and plasters, your #summerholiday essentials are here http://www.nhs.uk/Livewell/travelhealth/Pages/Travelhealthkit.aspx Upset stomach & the runs? Don’t go to your GP, feel better at home - http://www.nhs.uk/conditions/vomitingadults/pages/introduction.aspx Got #sunburn? Cover up, wear a high factor sunscreen and drink plenty of water #summerholiday Dizzy, with a dry mouth and headache? You may be dehydrated. Stay in shade & drink water for a #summerholiday recovery Looking forward to a family #summerholiday? Make sure you have the right first aid kit with you http://www.nhs.uk/Livewell/travelhealth/Pages/Travelhealthkit.aspx Holiday prescriptions / Going abroad this summer? Don’t forget your repeat prescriptions and first aid kit - http://www.nhs.uk/tools/pages/firstaidtoolkit.aspx North Over the counter travel advice Holiday prescriptions / over the counter travel advice tweets #firstaid #summerholiday Make sure you’re prepared for summer holiday blisters, cuts and rashes – remember to pack your first aid kit http://www.nhs.uk/tools/pages/firstaidtoolkit.aspx Not sure what first aid supplies you might need for a holiday abroad? Talk to your local pharmacy or visit http://www.nhs.uk/tools/pages/firstaidtoolkit.aspx Are you on medication for a long term condition? Make sure you speak to your pharmacist before going abroad so you have everything you need. Going on a #summerholiday abroad? Don’t forget repeat prescriptions & #firstaid kit http://www.nhs.uk/Livewell/travelhealth/Pages/Travelhealthkit.as px #beprepared Be prepare for #summer holiday blisters, cuts and bruises – remember to pack your #firstaid kit http://www.nhs.uk/tools/pages/firstaidtoolkit.aspx Not sure what #firstaid supplies you need for your #summerholiday? Talk to your local pharmacy or visit http://www.nhs.uk/Livewell/travelhealth/Pages/Travelhealthkit.as px On medication for a long term condition & going abroad? Your pharmacy can advise what you need #summerholiday North APPENDIX C – SUMMER HEALTH FACTS AND FIGURES Sprains and strains 1. In a sprain, one or more ligaments (tissue that connects two or more bones at a joint) is stretched or torn. 2. A strain is a stretch or tear to a muscle or a tendon (tissue that connects muscle to bone). 3. Two common sites for a strain are the back and the hamstring muscle in the back of the thigh. 4. It is most common for sprains to occur in the ankle. 5. Many things can cause a sprain - falling, twisting, or getting hit can force a joint out of its normal position. 6. PRICE therapy is recommended for minor sprains and strains. 7. You should not stop using a sprained joint. The injury will heal quicker if you begin to move the joint as soon as you can without experiencing significant pain. 8. Advice for muscle strains can be different. Depending on your injury, you may be advised to keep your injured muscle still for the first few days. 9. After an ankle sprain you will generally be able to walk 1-2 weeks after the injury, use your ankle fully after 6-8 weeks, and return to sporting activities after 8-12 weeks. 10. The time it can take to recover from a muscle strain can vary considerably. Some people can recover within a few weeks, whereas others may not be able to return to their normal activities for several months. Hay fever 1. It is estimated that there are more than 10 million people with hay fever in England. 2. There are around 30 types of pollen that could cause hay fever. North 3. 90% of people in Britain with hay fever are allergic to grass pollen. 4. Around 25% of people in Britain with hay fever are allergic to pollen from trees, including oak, ash, cedar and birch. 5. People with an allergy to birch often also experience an allergic reaction to apples, peaches, plums and cherries, as these types of fruit contain a similar protein to birch pollen. 6. It is possible to be allergic to more than one type of pollen. 7. In the UK, the pollen count season usually starts late March through to September. However, it can sometimes begin as early as January, or end in November. 8. Pollen count seasons: a. tree pollen – late March to mid-May b. grass pollen – mid-May to July c. weed pollen – end of June to September 9. Studies have shown that hay fever can severely affect a person’s quality of life, leading to time off work and school, and affecting children’s school exam results. 10. People who suffer rhinitis are at increased risk of developing asthma. Stings and bites 1. In the UK, bugs that bite include midges, mosquitoes, fleas, spiders, mites and ticks. 2. Insects that sting include bees, wasps and hornets. 3. An insect sting typically causes an intense, burning pain, quickly followed by a patch of redness and a small area of swelling around the sting. This usually eases and goes within a few hours. 4. In the UK most allergic reactions are caused by wasp stings. 5. Bee and wasp venoms are different. People who are sensitised and 'allergic' to wasp venom are rarely allergic to bee venom. North 6. When an insect bites, it releases saliva which causes the skin around the bite to become red, swollen and itchy. 7. In rare cases, some people can have a serious allergic reaction (anaphylaxis) to a bite or sting that requires immediate medical treatment. Sun exposure 1. Vitamin D is essential for healthy bones, and we get most of our vitamin D from exposure to sunlight. 2. A lack of vitamin D – known as vitamin D deficiency – can cause bones to become soft and weak, which can lead to bone deformities. 3. Short periods of sun exposure – about 10 to 15 minutes for most lighterskinned people - without sunscreen during the summer months (April to October) are enough for most people to make the right amount of vitamin D. 4. People with darker skin will need to spend longer in the sun to produce the same amount of vitamin D, as those with lighter skins. 5. The longer you stay in the sun, especially for prolonged periods without sun protection, the greater your risk of skin cancer. Skin cancer is one of the most common cancers in the UK, and too much sun increases your risk. 6. It is recommended to stay covered up for most of the time you spend outside and use sunscreen with a sun protection factor (SPF) of at least 15. 7. In 2010, around 100,000 people were diagnosed with skin cancer in the UK, and more than 12,000 skin cancers were malignant melanoma, the most serious type of skin cancer. 8. Each year, around 2,200 people die from skin cancer. May 2015