April 14, 2015 Meeting Minutes
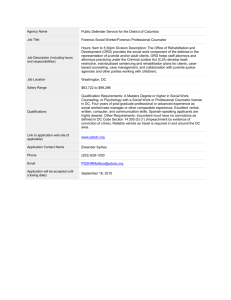
advertisement

Partners in Care Advisory Council Meeting Minutes 04-14-15 1) Welcome and Introduction: Carol, Sheila, and Connie welcomed everyone to the meeting and provided the group with an update from the workgroup that meets between meetings to summarize information collected at council meetings. Those attending were provided an opportunity to introduce themselves and share reasons why they joined the Council. Connie shared information from NAMI. She encouraged members to visit the website at NAMIhelps.org to access resources and hear about training opportunities. Connie provided multiple resource handouts for families, friends and staff attending the meeting. 2) Admission and Transfer Processes (Information given to families): Becky, SS Director, reviewed the welcome packet recently revised at the request of the Council. The family admission letter has been updated to include the many ways family members may choose to participate in meetings (e.g. conference call, in person or by Vidyo). A resource form will also be included to provide family members with a way to request information about community resources, commitment types, treatment planning, mental health diagnosis, etc. One family member shared that it would be helpful if there was a process in place for family members to be oriented into the Forensic mental health system. He stated that when his nephew was admitted he really didn’t even know what questions to ask. It was questioned if an orientation could be offered on a quarterly basis rather than relying on the annual Family Education seminar. All agree that it is important to also have staff call family members rather than just relying on sending the welcome letter. It was reiterated that although a Release of Information (ROI) is needed for staff to share personal information about a client, family is always able to provide information to staff (regardless of whether a release is signed). 3) Report from Program Directors on Options of Information to Send in Welcome Packets (also attached): Scott, MSH Program Director, asked the group to review several documents including the Campus map, MSH Admissions Unit Patient Handbook, Typical Day, and Visitor Guidelines and to come prepared to give input at the next meeting. If people like the resources we can work to replicate at all areas in MSH. Documents related to Transition Services are also asked to be reviewed prior to the next meeting, to discuss thoughts/suggestions. (THANK YOU IN ADVANCE). 4) What Can We Do To Change The Perception of St. Peter?: Discussion on the title of Security Counselor as being an oxymoron. “If someone is security, I wouldn’t necessarily feel like they are a person that I would bare my soul to”. Scott shared that he was a Security Counselor for 15 years and that the role is a balancing act. It would be good to look at the title and see if there’s something different that we could look at. Carol noted that Person-Centered Thinking training’s goal is that we need Page 1 of 10 to balance important to (understand goals/treatment plan) and important for (safety); engaged in both processes. Changes to Security Counselor would also involve Legislative and bargaining changes. Education requirements were asked about, and Scott responded that minimum qualifications note a High School Diploma. Preferred qualifications indicate a degree. Training at Forensic Services is three weeks long to review policies and procedures, techniques, Person Centered Thinking, and job coaching is provided on the units. There are Security Counselors and Security Counselor Leads (expected to give guidance to staff in the work area). Darius suggested Security Liaison/Officer as possible alternative titles. 5) How to Be More of a Hospital Resource Versus Restrictive Environment: Discussion Carol referenced the prior ranking process Partners completed in the effort to prioritize goals. One noted was how Forensic Services could work to be perceived more like a hospital vs. correctional facility. The role of Forensic Services is to be therapeutic and also address public safety. We can work on creating environment that is more of a treatment environment instead of a prison. Promote the work that individuals do in the community. Overview on work crews from Gregg. 1:6 staff to person-served ratio. Various companies and people are glad to see us. We work to community standards. (Main street watering, Bi-fun). Sheila talked about when her son first came here, and how it had felt that she had absolutely no voice. Hope was waning, and she was frustrated. Counsel has helped, developed relationship with people that work here. There is trust that her son will get what he needs here. Sheila’s voice is more positive, and will now contribute to how the program is perceived. Connie spoke and noted that it took are about 2 years to tell her family/friends that her son was at St. Peter. The Counsel assisted in helping her open up. She now educates those in the community about the 4 programs that are offered here, and hopes that is her small part in helping with the stigma. Charlotte spoke of not seeing her son since the holidays and how he was feeling sad and down. She noted that the facility and staff worked to assist in visits for them to have 2 visits with his elderly cat, which helped him so much. This shows that the program is changing for the better! Carol M., said that when she shared with others that her son was receiving care at St. Peter their response was “thank goodness! Hopefully he can get the help that he needs.” Carol thanked St. Peter, and noted that although people make a lot of nasty comments; she’s been really happy about her son’s care for the most part. Marisa asked about proactive media relations, and spreading a positive message (ie. positive stories to newspapers). Carol shared that this continues to be attempted, though ultimately newspaper choose what they would like to print, and they don’t pick up on those. Commissioner spoke with MPR two weeks ago, as they reached out to her. MPR Page 2 of 10 wanted to know changes that have occurred. Offered supportive data, and initiatives, including the Counsel. There is also a Quarterly Community Liaison Meeting held at Forensic Services, (includes: St. Peter Police Department, Gustavus, Rivers Edge, bigger organizations in city) to help them stay engaged and informed. Coming up in May, there will be an After Hours Business Meeting with Chamber of Commerce held on campus to help promote who we are. Break Out Groups Talk openly about the mission of MSH, word of mouth. Change name of the facility to something other than Minnesota Security Hospital. Ensure staff knows why they are here. Advertise opening / the truth of the facility. Public Relations Department Set aside money for above. Educate counties, judges, attorneys about what we do. Publicize success stories without identifying documentation. Look at AMRTC-why do they have a positive image? Need to counteract negative media. Community involvement/Family involvement Virtual Tour of MSH/New Facility Get the truth known, not the sensationalism Have the building look nice-not like a prison When hiring people, ask different questions of background-not as many corrections Staff interactions with parents/family members (additional clinical training) Knowing the number of the Executive on Call (EOC) Consistency of rules (e.g. what can be brought in or not) Instituting an Auxiliary for fundraising efforts Change Security Counselor to Safety Counselor Opening campus to public (gates, trading post, etc.) Public website for hospital Olmstead Plan might alleviate this issue as people are integrated into the community and may not require hospitalization Improve outer yards, more inviting, flowers, vines, furniture, labyrinth, walking paths Bars on windows (dark) at Bartlett, entrance needs to be spruced up Number of people on each unit, too cramped Quiet hour every afternoon, no TV, radio, all in their own rooms Sign-in sheet for sensory rooms Colorful artwork, units need color! Nature/Natural elements, plants, etc. Visits (staffing & preparing), entrance intimidating, flexible in time & locations, look at new construction & think of options, is it enough? Staff being more informed on what/how to share information Emergency guardianships? Psychiatric Healthcare Directives? Mentally illness & dangerous Security Counselor – mind shift re: therapeutic relationship Family Therapy/Interventions (social supports) Privacy w/phone Page 3 of 10 Therapeutic animals Volunteers visiting patients, especially those who don't usually have visitors Staff or liaison personally connecting with a family member on their first visit thru security Ongoing volunteers at visiting sites during busier times (NAMI provides training for a program called 'NAMI in the Lobby') Emphasizing the extreme importance of first-contact people (ie. gate security people) Volunteers helping at Holiday times to wrap gifts, etc. (also NAMI is willing to include St. Peter in their Holiday gift donation drive). 6) Members as Advocates for Those Who do not Have Family Involvement. Prior to her maternity leave, Krista, Patient Advocate, discussed this topic in all Patient Advisory Council Meetings and asked that the message be carried back to the units. She shared that the members of Partners in Care wanted all to know that their service is not only for their loved ones, but for all that receive care at Forensic Services. She said the response was of appreciation and gratitude. 7) Evaluation Summary: The meeting was focused. The meeting was productive. The meeting was wellpaced. We made good progress. Strongly Agree Agree Neutral Disagree Strongly Disagree 7 3 0 0 0 7 3 0 0 0 9 1 0 0 0 8 2 0 0 0 What went well: The small group brainstorming was wonderful! Very great opportunity to share thoughts, ideas. Everything! Lord the collaboration. Loved getting to know the staff too. Small group discussion. Able to talk about concerns. Communication is excellent. It is quite obvious that staff cares and working to make this hospital a state of the art in care for patients. Agenda was covered well. I felt it was a productive meeting. The topics that were brought to the table were relevant and there was good discussion. Just wonderful to have staff coming to work with us. Really grateful. Page 4 of 10 What could be improved? Please include at least 2-3 Security Counselors at the meeting. Include Security Counselors in the group. Carol: I mentioned this to Julie & just want to ask/suggest that we consider including a direct care staff to this meeting. I think some of the family statements are so powerful & bring the humanity back to what we do it helps keep things in perspective. I know we would have RNs interested & I'm certain LPN/HSS would be interested. Not sure if it would be disrupted or disconnected if you only attended occasionally but just wanted to mention it. Also not sure how much bigger we want the group to be. Artwork done by patients. I can tell staff is putting in extra effort by the amount of forms they have produced. Seating of members should be arranged to mix the staff and parents, similar to discussion groups. Keep comments more topic focused. (Not about this meeting itself) Security Counselors need to have a higher level of education. What would be an agenda item you'd like to see at a future meeting? Group meeting content. How much time is spent in actual treatment programming? These meetings are one of the best efforts I have seen. At the moment I cannot think of anything more to mention other than what I did in the group meeting. Patient surveys on hospital vs. restrictive environment. Unit by unit to see patient direct results on our initiatives and give them perspective on how their feelings change as they move from unit to unit and their treatment plan progresses. Raising money for the hospital. Page 5 of 10 FORENSIC TRANSITION SERVICES Johnson Hall & Bartlett 1 North Contact Information Program Supervisors: Julie Roehm, Program Director: 507-985-2155 Robin Bode, Clinical Director: 507- 985- 2502 Jo Blaschko, RN Administrator: 507-985- 2404 How to contact your friend or family member: Johnson Hall: 507-985-2444 Bartlett 1 North: 507-985-2400 *Unit phones are staffed 24/7. Staff will page the individual or provide a message to return your call. PROGRAM DESCRIPTION Forensic Transition Services (FTS) is the non-secure treatment program within Forensic Services. We serve adults committed as Mentally Ill and Dangerous who have been approved for transfer by the Special Review Board. The program is located in two sites: Johnson Hall and Bartlett 1 North. Although the physical plant structures are very different, FTS strives to operate as one program rather than two distinct units. Program staff provide direct service to persons on both units. Each individual has a treatment team that includes behavior analyst, social work, psychology, recreation therapy, and nursing, in addition to other ancillary professional services, dependent on client needs. Psychiatric services are provided on a consultative basis by a psychiatric nurse practitioner. Patients meet with their psychiatric provider a minimum of once every three months, with more frequent contacts as clinically indicated. As an open program, the FTS mission is to provide community reintegration and discharge preparation services. Unless clinically contraindicated, individuals have unsupervised grounds liberty and independently attend programs at various sites on campus. Patients attend groups, activities, work therapy and psychiatric appointments outside of the unit to reflect what they will experience following discharge. A key treatment component is Therapeutic Pass Planning, a structured process that includes community living skills, pass plan development and risk assessment. As individuals progress in treatment and become eligible for pass plan, off campus passes with family or significant others can be requested. If a family member’s home would be a good place for visits, staff will first conduct an interview and home visit. If your family member is eligible to visit home, staff will discuss the procedures with you in detail. It is our hope to assist you in having a positive visiting experience with your family member. The attached includes some important visitor information, but is not all inclusive. Please do not hesitate to contact the supervisors noted above, or other team member with any questions, concerns or feedback. We look forward to working with you in our efforts to support your family member’s continued treatment progress. Page 6 of 10 Typical Day for a Patient at Minnesota Security Hospital. Patients at the Minnesota Security Hospital are involved in a variety of activities on a daily basis. Each day can be different, whether it is a week day or a weekend or holiday. Different treatment environments also have different schedules. A “typical” day for a patient on a week day would look something like this. Patients generally wake up around 6:30 am to get medications, prepare for their day and then eat breakfast at 7:00 am. After breakfast, patients will then prepare for their days activities. Each client has an individual schedule constructed around their needs. Patients are served lunch on their units around noon. They will then continue on with their individual schedule. Patient will then begin returning to their units around 4 pm to take medications and to relax before the evening meal around 5 pm. After the evening meal, they will engage in individual and group recreational activities either on or off the unit. Some specific “pieces” or components of patient schedules are listed below. These lists are not all inclusive. Treatment Groups Individual Therapy Sessions Education Opportunities Vocational Programming Opportunities Therapeutic Recreational Opportunities o Gym activities o Art Activities o Library o Open social times and games o Canteen o Music opportunities One to One meetings with: o Security Counselor o Nurses o Psychiatric Providers o Medical Doctors o Behavioral Analysts o Social Workers Page 7 of 10 Forensic Transition Services Visitor Information Transition Services staff encourages visiting and contact from family and friends. We ask that you visit outside programming hours (after 3pm Mon-Fri) but can make exceptions if needed. Visiting areas are available in both Johnson Hall and Bartlett Hall1-North. If you would like to visit at Gluek Park or in the Sunrise building, please have your family member ask staff to reserve the location. For privacy purposes visitors are not allowed to walk around campus. We ask that you check in with staff at the beginning of each visit. If you are bringing items for patients please make staff aware. Children are welcome to visit family members but must be supervised at all times. The campus is non –smoking. Tobacco, Tobacco products or E-cigarettes are not allowed in any building. Family pets may be allowed to visit (off unit), if pre-approved by treatment staff and a current copy of the pet’s vaccinations are on file. Cell phones and cameras are not allowed in any patient area or residential building on campus. For privacy purposes we ask that you leave these in your car during any visits. If there are concerns about items that may be considered contraband, staff may ask to inspect handbags and/or belongings Page 8 of 10 Physical contact during visit: A kiss and hug will be allowed at the beginning and the conclusion of the visit. Hand holding on or above the table, having an arm around the shoulder, and leaning the head on a shoulder are allowed. With prior team approval, patients can hold children six years of age and under on their lap. Visitor Responsibilities All visitors are expected to dress in an appropriate manner. No revealing clothing is allowed. Sunglasses, headwear, and coats/jackets are not allowed in the visiting room. To ensure the safety of all patients, visitors, and staff, please comply with the visitor process, rule, and staff direction. We take out safety and security responsibilities of patients, staff, and visitors very seriously. We appreciate your cooperation in this process and welcome any questions or concerns. Please note: The buildings and grounds of the St. Peter Regional Treatment Center are tobacco-free. Minnesota law prohibits the possession of tobacco, alcohol, or firearms at the facility. If you have any questions related to visiting please call the Minnesota Security Hospital Visitor Office at 507-985-2516. Page 9 of 10 Page 10 of 10