PP-BHS-QM-10-23-Out-of-County-Certification-and-Billing
advertisement

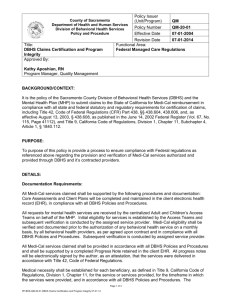
County of Sacramento Department of Health and Human Services Division of Behavioral Health Services Policy and Procedure Policy Issuer (Unit/Program) QM Policy Number QM-10-23 04-14-2009 Effective Date 07-01-2014 Revision Date Functional Area: Chart Review Non Hospital Services Title: Out of County Certification and Billing Procedure Approved By: (Signature on File) Signed version available upon request Kathy Aposhian, RN Program Manager, Quality Management BACKGROUND/CONTEXT: The Division of Behavioral Health Services (DBHS) and Mental Health Plan (MHP) claims Medi-Cal on behalf of the contracted provider. Designated MHP staff is responsible for the review process to assure the services provided are in compliance with state and federal statutory and regulatory requirements for the services provided and claimed for Medi-Cal reimbursement. MHP Quality Management staff provides site certification, credentialing and utilization review. PURPOSE: The purpose of this policy is to establish responsibilities and duties for accurate review and claiming of services by designated out of county providers based on the Contract agreement. DETAILS: Procedure: A. MHP Contract Monitor Responsibilities: 1. Identify the need for an out of county provider. 2. Send copy of the following documents to Quality Mangement (QM) a. Site Certification Letter from Host County b. Provider site current fire clearance. c. List of provider staff including: i. Name ii. Title iii. National Provider Identifier (NPI) Number iv. License Type and License Number d. Provider Contact person information i. Name ii. Phone number or e-mail address 3. Verify out of county provider’s host county billing rate. 4. Work with the contracts unit to prepare and send to the provider the SB 785 Contract and Packet document. 5. Verify all certification documents listed above are complete and accurate prior to service authorization. Page 1 of 4 PP-BHS-QM-10-23-Out of County Certification & Billing Procedure 07-01-14 6. Ensure service authorization for the requested services is provided 7. Provide applicable P & P to provider, as appropriate. B. MHP Administrative Officer (ASO): 1. Request provider number from DHCS and forward to QM. 2. Request program, unit rate and treatment code set up from Avatar Team. 3. Provide billing mechanism and instruction support for the provider, as needed. C. Quality Management Responsibilities: 1. Site Certification will: a. Create a provider file b. Verify Organization NPI, site certification, and fire clearance expiration date. c. Notify the MHP Contract Monitor if information requested is not received or is incomplete. 2. Staff Registration will: a. Verify licensed staff with appropriate board. b. Verify Individual NPI number. c. Verify staff is not on the OIG Excluded Persons list. d. Assign Billing ID number. e. Send Billing ID # to PDS OOC Admin Staff. 3. Quarterly, review sample of progress notes in coordination with the MHP Contract Monitor. 4. Conduct special reviews required by the MHP certification, problem resolution or compliance policies. D. MHP Services Data Entry Staff Responsibilities: 1. Verify monthly that the client has Medi-Cal. 2. Notify DBHS Contract Monitor if client does not have Medi-Cal or information is not received from the provider, as requested. 3. Notify QM Staff Registration if provider billing staff do not have a Billing ID#. 4. Upon receipt of the invoice, enter services into Avatar billing system. 5. Scan progress notes into the client’s chart in Avatar Clinical Workstation Station. Shred copies of the progress notes sent by provider according to the Avatar Document Management for Clinical Records Policy. 6. File invoice documents by fiscal year. E. Out of County Provider responsibilities: 1. Ensure medical record documentation includes the following: a. Admission assessment is completed to include: i. Health and psychiatric histories; ii. Psychosocial skills; iii. Current psychological, educational, vocational, and other functional limitations; iv. Medical needs, as reported. b. Treatment Plan specifies specific treatment needs and goals. i. Descriptions of specific services to address the identified treatment needs and goals. ii. Treatment Plan is signed and dated by program staff and client. c. Outpatient (Non Day Treatment Intensive programs) Progress Notes: Page 2 of 4 PP-BHS-QM-10-23-Out of County Certification & Billing Procedure 07-01-14 i. Accurately record all direct, collateral, and case management brokerage services with, and on behalf of client. ii. Progress notes must describe interventions used, response of the client to those interventions, and progress toward treatment goals. iii. Provider must sign each progress note. 2. Day Treatment Intensive and Day Rehabilitation (DTI, DR): Provide the Weekly Summary Progress Report, signed by the Program Director or designee. This documentation must include the following: a. Progress or lack of progress towards the treatment goals; b. Barriers identified that impact progress towards those goals; c. Interventions that were tried during the previous month; d. Receptivity by client; e. If lack of progress was noted, indicate new interventions initiated; f. Follow-up and future treatment plans. 3. All providers, upon discharge, provide summary documentation indicating client and program staff collaboration including: a. Outline of services provided; b. Goals accomplished; c. Reason and plan for discharge; d. Referral follow-up plans. 4. All providers will submit progress notes to DBHS Contract Monitor with each invoice and/or upon request. Designated Quality Management staff and MHP Contract Monitor will collaboratively conduct a Quality Assurance process at least on a quarterly or more frequently, if needed. 5. All providers will submit an assessment and treatment plan as soon as they are complete, to the DBHS contract monitor. 6. For providers delivering DTI/DR services, provider will submit to the DBHS contract monitor, the weekly schedule with the first invoice submitted to the county. F. Provider Billing Procedures: 1. Outpatient Services: Submit monthly billing invoice with the following elements included: a. Client Name; b. Specify the number of minutes an approved service was provided and the associated treatment codes for the services provided; c. Diagnosis and diagnosing staff; d. Staff name who provided the service. 2. DTI/ DR: Complete monthly invoice of services provided. The following elements must be completed in addition to those specified above: a. Documentation of the reason the client was absent (due to leave of absence (LOA), hospitalization, etc.). Those dates are specifically excluded from billing. b. Documentation of “unavoidable Absences” (defined as unplanned absences from services), including reasons for absence, amount of time beneficiary participated in services for that day, and whether the amount of time is greater than 50% of the total scheduled DTI/DR time. c. Provider will verify the billing dates are consistent with the client participation in the program as evidenced by his/her signature on the billing invoice documents. 3. Submit completed invoice to the designated DBHS Children’s services staff by the 15th of every month, including supporting clinical/progress notes to verify billing. Page 3 of 4 PP-BHS-QM-10-23-Out of County Certification & Billing Procedure 07-01-14 4. Provider is responsible to maintain a complete clinical record for all services. Such a record will be made available to the MHP in the event of any clinical, fiscal or quality assurance audit to meet all State and Federal regulations. All denials and audit exceptions shall be reconciled by DBHS in accordance with existing procedures. 5. If needed, submit reassessment plan to the Child and Family Access Team, two weeks prior to the expiration of the current authorization. Services rendered without a valid authorization are not reimbursable by the MHP. REFERENCE(S)/ATTACHMENTS: Title 9 Article 3.5, §531,532-541, 1840.332-1840.354 SB 785 RELATED POLICIES: No. 20-10 MHP Claims Certification and Program Integrity No. 05-04 Instruction for Completion of Day Program Attendance Sheet No. 00-07 Avatar Document Management for Clinical Records DISTRIBUTION: Enter X X X DL Name Enter X Mental Health Staff Adult Contract Providers Children’s Contract Providers Alcohol and Drug Services Mental Health Treatment Center Specific grant/specialty resource CONTACT INFORMATION: Paul Vossen, MFT Out of County Program Coordinator VossenP@SacCounty.net Tiffany Greer, LCSW Quality Management Program Coordinator Adult and Children’s Program Liaison QMInformation@SacCounty.net Page 4 of 4 PP-BHS-QM-10-23-Out of County Certification & Billing Procedure 07-01-14 DL Name