Should any specific chest compression depth vs
advertisement
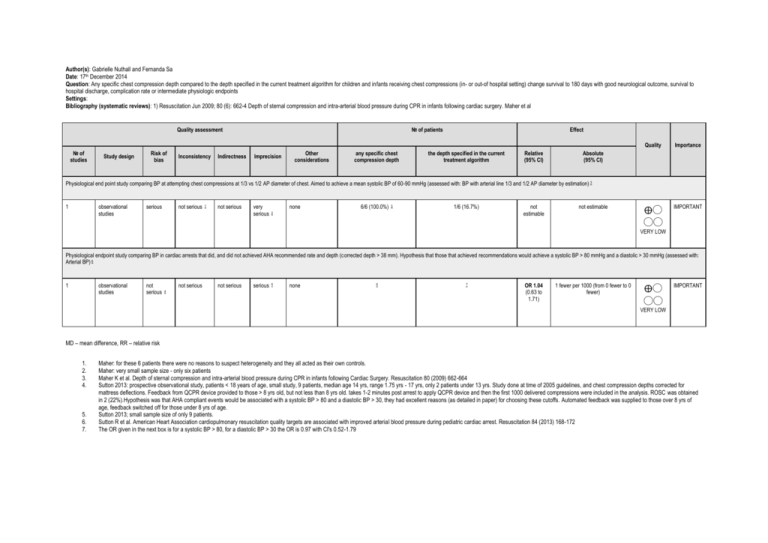
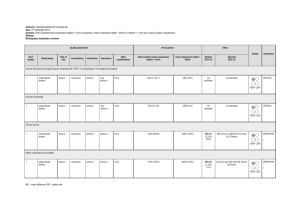
Author(s): Gabrielle Nuthall and Fernanda Sa Date: 17th December 2014 Question: Any specific chest compression depth compared to the depth specified in the current treatment algorithm for children and infants receiving chest compressions (in- or out-of hospital setting) change survival to 180 days with good neurological outcome, survival to hospital discharge, complication rate or intermediate physiologic endpoints Settings: Bibliography (systematic reviews): 1) Resuscitation Jun 2009; 80 (6): 662-4 Depth of sternal compression and intra-arterial blood pressure during CPR in infants following cardiac surgery. Maher et al Quality assessment № of studies Study design Risk of bias Inconsistency Indirectness № of patients Imprecision Other considerations any specific chest compression depth Effect the depth specified in the current treatment algorithm Relative (95% CI) Quality Importance ⨁◯ ◯◯ IMPORTANT Absolute (95% CI) Physiological end point study comparing BP at attempting chest compressions at 1/3 vs 1/2 AP diameter of chest. Aimed to achieve a mean systolic BP of 60-90 mmHg (assessed with: BP with arterial line 1/3 and 1/2 AP diameter by estimation) 3 1 observational studies serious not serious 1 not serious very serious none 6/6 (100.0%) 3 1/6 (16.7%) 2 not estimable not estimable VERY LOW Physiological endpoint study comparing BP in cardiac arrests that did, and did not achieved AHA recommended rate and depth (corrected depth > 38 mm). Hypothesis that those that achieved recommendations would achieve a systolic BP > 80 mmHg and a diastolic > 30 mmHg (assessed with: Arterial BP) 6 1 observational studies not serious not serious 4 not serious serious 5 none 6 7 OR 1.04 (0.63 to 1.71) 1 fewer per 1000 (from 0 fewer to 0 fewer) ⨁◯ ◯◯ IMPORTANT VERY LOW MD – mean difference, RR – relative risk 1. 2. 3. 4. 5. 6. 7. Maher: for these 6 patients there were no reasons to suspect heterogeneity and they all acted as their own controls. Maher: very small sample size - only six patients Maher K et al. Depth of sternal compression and intra-arterial blood pressure during CPR in infants following Cardiac Surgery. Resuscitation 80 (2009) 662-664 Sutton 2013: prospective observational study, patients < 18 years of age, small study, 9 patients, median age 14 yrs, range 1.75 yrs - 17 yrs, only 2 patients under 13 yrs. Study done at time of 2005 guidelines, and chest compression depths corrected for mattress deflections. Feedback from QCPR device provided to those > 8 yrs old, but not less than 8 yrs old. takes 1-2 minutes post arrest to apply QCPR device and then the first 1000 delivered compressions were included in the analysis. ROSC was obtained in 2 (22%).Hypothesis was that AHA compliant events would be associated with a systolic BP > 80 and a diastolic BP > 30, they had excellent reasons (as detailed in paper) for choosing these cutoffs. Automated feedback was supplied to those over 8 yrs of age, feedback switched off for those under 8 yrs of age. Sutton 2013; small sample size of only 9 patients. Sutton R et al. American Heart Association cardiopulmonary resuscitation quality targets are associated with improved arterial blood pressure during pediatric cardiac arrest. Resuscitation 84 (2013) 168-172 The OR given in the next box is for a systolic BP > 80, for a diastolic BP > 30 the OR is 0.97 with CI's 0.52-1.79