SELF-ASSESSMENT of COMPANION ANIMAL MEDICAL RECORDS
advertisement
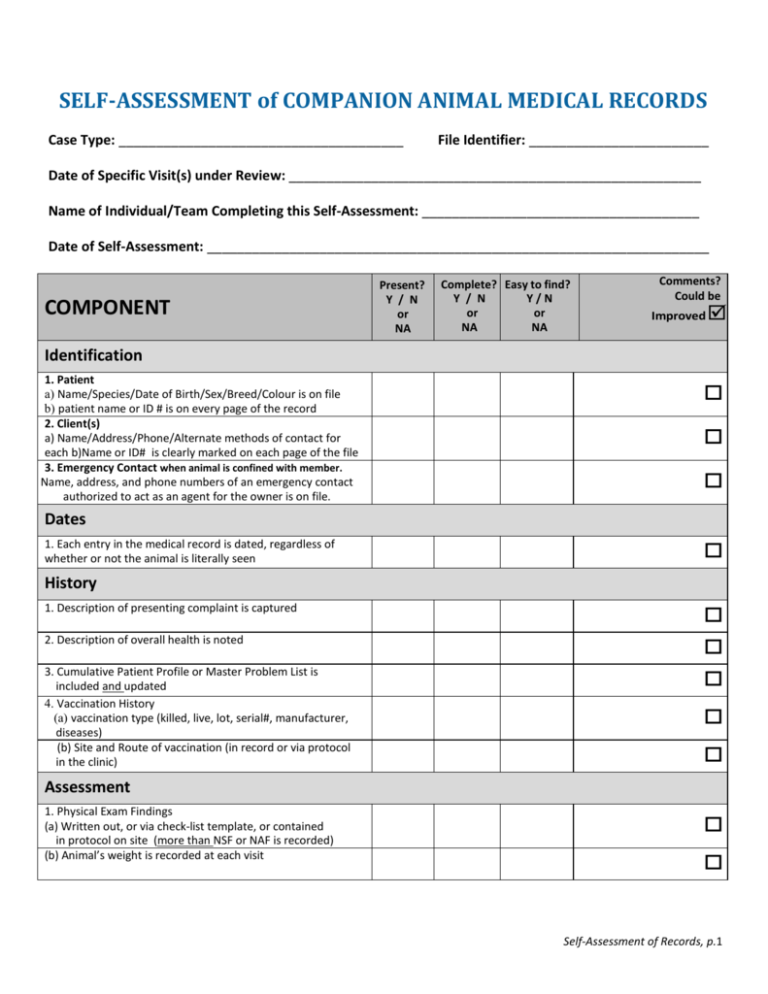
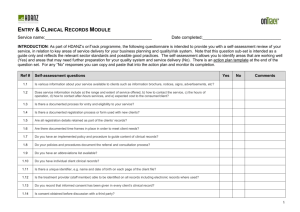
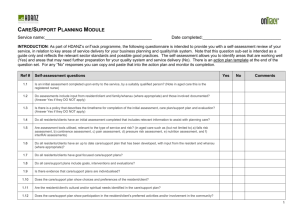
SELF-ASSESSMENT of COMPANION ANIMAL MEDICAL RECORDS Case Type: ______________________________________ File Identifier: ________________________ Date of Specific Visit(s) under Review: _______________________________________________________ Name of Individual/Team Completing this Self-Assessment: _____________________________________ Date of Self-Assessment: ___________________________________________________________________ COMPONENT Present? Y / N or NA Complete? Easy to find? Y / N Y/N or or NA NA Comments? Could be Improved Identification 1. Patient a) Name/Species/Date of Birth/Sex/Breed/Colour is on file b) patient name or ID # is on every page of the record 2. Client(s) a) Name/Address/Phone/Alternate methods of contact for each b)Name or ID# is clearly marked on each page of the file 3. Emergency Contact when animal is confined with member. Name, address, and phone numbers of an emergency contact authorized to act as an agent for the owner is on file. Dates 1. Each entry in the medical record is dated, regardless of whether or not the animal is literally seen History 1. Description of presenting complaint is captured 2. Description of overall health is noted 3. Cumulative Patient Profile or Master Problem List is included and updated 4. Vaccination History (a) vaccination type (killed, live, lot, serial#, manufacturer, diseases) (b) Site and Route of vaccination (in record or via protocol in the clinic) Assessment 1. Physical Exam Findings (a) Written out, or via check-list template, or contained in protocol on site (more than NSF or NAF is recorded) (b) Animal’s weight is recorded at each visit Self-Assessment of Records, p.1 COMPONENT Present? Y / N or NA Complete? Y / N or NA Easy to find? Y/N or NA Comments? Could be Improved (c) Differential diagnoses are listed (d) Provisional/final diagnosis included (e) Diagnostics: Record of diagnostic plans to clarify assessment; results retained in record; results interpreted and interpretation noted Treatment Plans 1. Plan of action, including follow-up plans, recorded 2. Drug treatments: Name of drug/strength/dose/quantity/directions for use; repeats/warnings are all included 3. Detailed surgical notes or protocols are present 4. Anesthetic / analgesic notes or monitoring forms are present 5. In-hospital monitoring notes are present 6. Fluid therapy: type/rate/route/amount received/medications added are detailed Client Communications and Professional Advice 1. There are signed consent forms for procedures (not just surgical consent forms). 2. Cost estimates are used for all diagnostic tests or procedures (not just surgical procedures). 3. There is an indication that discussion took place and informed consent was obtained 4. Declined diagnostic investigations and treatment plans are recorded 5. Ongoing communications documented for hospitalized patients 6. Homecare or Discharge Instructions were provided and documented in the record (copy in the record or reference to a template). 7. Client Education information/forms were provided and are Documented (either by copy or reference to a template). 8. Personal and telephone / FAX / email communication with /messages for clients are included and documented by date. 9. Referral letters/ reports are included in the record, and follow-up communication with owner is documented Reports A copy of all reports prepared with regard to the patient (vaccination certificates, referral letters, etc) Self-Assessment of Records, p.2 COMPONENT Present? Y / N or NA Complete? Y / N or NA Comments? Could be Easy to find? Y/N or NA Improved Fees and Charges Fees and charges are noted in file, with those for drugs listed separately from those for advice or other services. Radiographs Radiographs are permanently identified with: name of veterinarian or facility; patient ID; date; indication of L or R side of the animal; indication of time for sequential studies Logs Appropriate logs/registers are maintained for: anesthetic/surgery/radiology/controlled drugs/ketamine/targeted drugs Comments? RECORDS MANAGEMENT Y N N/A Could be improved Medical records are legible. Records are kept in a systematic manner. Changes in records are clearly indicated as changes. Entries in the record are initialed. Records are retained for 5 years after the date of the last entry. A Records Security protocol is in place and staff is trained. A policy on Privacy/Personal Information Protection is visible to clients and understood by staff. A procedure is in place for the transfer of medical information. ASSESSMENT OUTCOME As a result of this exercise, I / we have discovered or decided the following: Areas for improvement in record keeping Plans to address these areas 1. 1. 2. 2. 3. 3. 4. 4. 5. 5. Self-Assessment of Records, p.3