Men`s Health - (HME) Project
advertisement
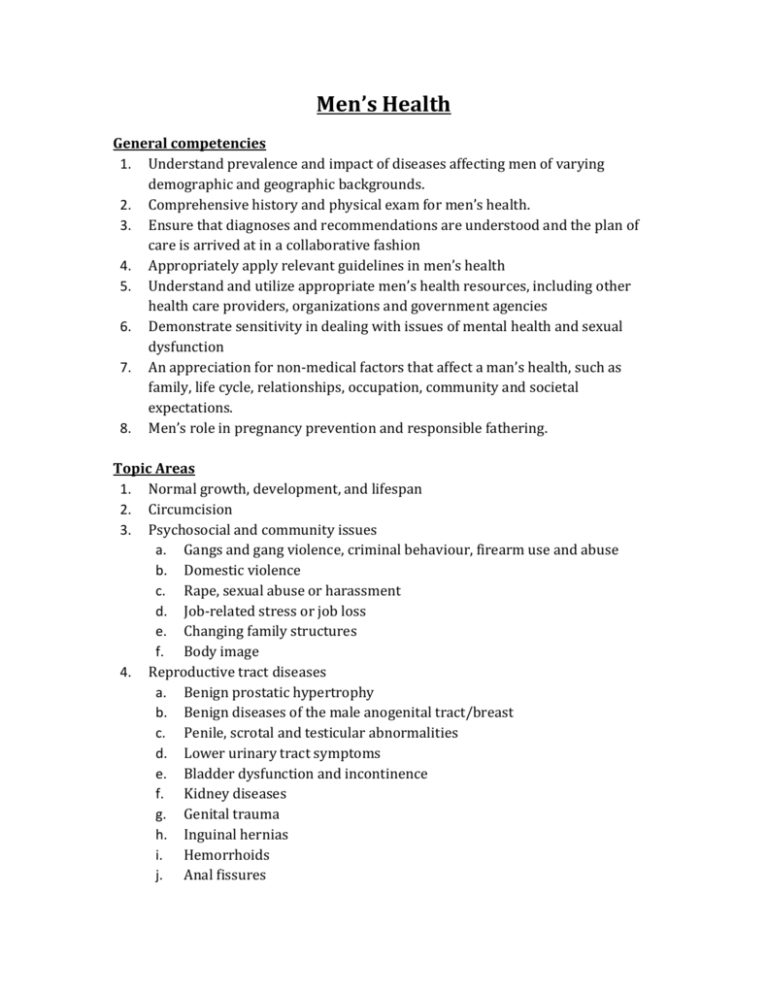
Men’s Health General competencies 1. Understand prevalence and impact of diseases affecting men of varying demographic and geographic backgrounds. 2. Comprehensive history and physical exam for men’s health. 3. Ensure that diagnoses and recommendations are understood and the plan of care is arrived at in a collaborative fashion 4. Appropriately apply relevant guidelines in men’s health 5. Understand and utilize appropriate men’s health resources, including other health care providers, organizations and government agencies 6. Demonstrate sensitivity in dealing with issues of mental health and sexual dysfunction 7. An appreciation for non-medical factors that affect a man’s health, such as family, life cycle, relationships, occupation, community and societal expectations. 8. Men’s role in pregnancy prevention and responsible fathering. Topic Areas 1. Normal growth, development, and lifespan 2. Circumcision 3. Psychosocial and community issues a. Gangs and gang violence, criminal behaviour, firearm use and abuse b. Domestic violence c. Rape, sexual abuse or harassment d. Job-related stress or job loss e. Changing family structures f. Body image 4. Reproductive tract diseases a. Benign prostatic hypertrophy b. Benign diseases of the male anogenital tract/breast c. Penile, scrotal and testicular abnormalities d. Lower urinary tract symptoms e. Bladder dysfunction and incontinence f. Kidney diseases g. Genital trauma h. Inguinal hernias i. Hemorrhoids j. Anal fissures 5. 6. 7. k. Gynecomastia l. Hypogonadism and other hormonal dysfunction m. Hematuria n. Andropause Neoplastic disease of the male genital tract and breast a. Penile carcinoma b. Testicular carcinoma c. Prostatic carcinoma d. Bladder carcinoma e. Renal carcinoma f. Breast carcinoma Reproduction a. Normal physiology and anatomy b. Infertility c. Contraception methods d. Effects of aging Sexuality a. Sexual orientation b. Sexual responses throughout life cycle c. Erectile dysfunction d. Ejaculatory dysfunction e. Changes in libido f. Variety of sexual behaviours g. Reproductive responsibility h. Testosterone deficiency For each topic area 1. Epidemiology 2. Anatomy 3. Pathophysiology/Etiology 4. Risk factors 5. History and physical exam 6. Diagnostic Tests 7. Differential diagnosis 8. Management 9. Psychosocial implications Highlighted teaching points 1. History and physical exam a. Comprehensive men’s health history (including relational, sexual and occupational history) b. Perform a systematic male physical examination i. Urogenital exam in infancy, childhood, adulthood, elderly ii. Tanner staging iii. Examination of penis, testicles, scrotal contents, inguinal canals, rectum, prostate, and breast 2. Diagnostic tests (including indications and interpretation) a. Testosterone testing b. Bone density testing c. PSA value, velocity and density d. Cancer staging (e.g. Gleason scores) e. Microscopic diagnosis of urine 3. Management (including indications) a. Foley catheter placement b. Neonatal circumcision c. Treatment modalities for penile condylomata d. Vasectomy and reversal 4. Counseling a. Alcohol and other substance use and abuse (including tobacco) b. Sexually transmitted infections (STIs) and teen pregnancy c. Motor vehicle safety, seat belt and helmet use d. Firearm safety e. Medication safety f. Exercise prescription g. Performance-enhancing drugs h. Contraception i. Domestic violence j. Parenting k. Indications, contraindications and current evidence concerning circumcision References: 1. American Academy of Family Physicians. (2008). Recommended Curriculum Guidelines for Family Medicine Residents, Men’s Health (Reprint No. 278), Leawood, Kansas. 2. College of Family Physicians of Canada. (2010). Defining Competence for the purposes of certification by the College of Family Physicians of Canada: The evaluation objectives in family medicine. Mississauga, ON.