NHS Doncaster Community Pharmacy Inhaler Check
advertisement
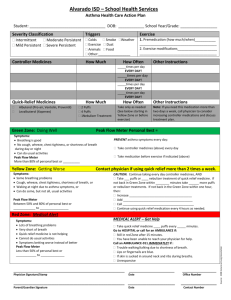
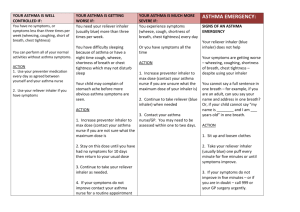
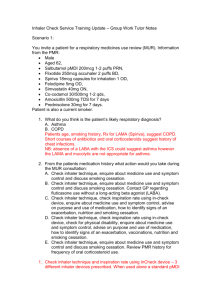
NHS Doncaster Community Pharmacy Inhaler Check Service Evaluation involves discussion about diagnosis, pattern of use of different medicines and review of inhaler technique. May 2014 The In-Check DialTM device is used to help demonstrate to patients the optimum IR required to maximise use of their prescribed inhaler device. Background Asthma and Chronic Obstructive Pulmonary Disease (COPD) are common respiratory conditions. Asthma affects up to 5.4 million people in the United Kingdom (UK) and is still killing people. The number of reported deaths in the UK is the highest in Europe.1 COPD is estimated to affect 3 million people in the UK, with deaths in England double the European average.2 Aims of the Service To help patients to optimise the use of inhaled medication and improve respiratory management. Service Evaluation Aim and Objectives: To evaluate a community pharmacy inhaler check service. To identify the number of patients using the service, inhaler use issues and interventions provided by community pharmacists, exploring patient satisfaction with the service and ideas for service development. Between April 2013 and February 2014 there were 313 emergency admissions for asthma with an inpatient cost of £306,127 and 869 emergency admissions due to COPD at a cost of £1,871,651.3 Setting: Twenty-nine community pharmacies across Doncaster. The mainstay of treatment for both asthma and COPD is inhaled therapy. Short-acting bronchodilators (‘reliever’ inhalers) are used to relieve breathlessness. Maintenance treatment is with ‘preventer’ inhalers e.g. inhaled corticosteroids. There are many different inhaler devices e.g. metered dose inhalers (MDIs) and dry powder inhalers (DPIs). Different devices require different inspiration rates (IRs). Methods: A mixture of research methods were used for data collection: audit of 616 consultations and analysis of 577 patient satisfaction questionnaires. Audit and questionnaire results were analysed using descriptive statistics, qualitative comments using a thematic approach. Limitations: Information and investigator bias, and poor piloting and design of the data collection tools limited the methods used. Rationale for the service Suboptimal inhaler use can result in poor condition control (leading to increased prescribing costs for reliever inhalers and unnecessary hospital admissions) as well as medicine waste. Community pharmacists are taught as part of their undergraduate course about different inhaler devices and there are examples of community pharmacy respiratory projects across the country demonstrating the role of community pharmacists in optimising inhaled medicine use. Evaluation Results Overall Scheme Cost and Period Covered Total cost of the service from January-March 2014 including initial set-up/training costs and evaluation: £7561.50 A&E Attendances and Admissions Avoided The pilot Pharmacy Local Professional Network for NHS South Yorkshire & Bassetlaw developed a respiratory support service that ran from September 2012 until the March 2013. Service evaluation found that community pharmacists helped over 1000 patients who were not using their inhaler correctly achieve the optimum IR during one consultation.4 The short time period the service has been running for make it difficult to identify whether or not the service has had an impact on A&E attendances/admissions. Doncaster Local Pharmaceutical Committee (LPC) secured funding from NHS Doncaster to recommission this service from January to March 2014 using Winter funding. This report provides a summary of the findings from evaluation of the service. Previous Inhaler Technique Instruction Diagnosis Two-thirds of patients reported asthma as their condition with nearly a quarter reporting COPD. A significant minority were unsure of their diagnosis. Most patients had received previous instruction. Inhaled Therapy The majority of patients (82.2%, n=616) were prescribed a MDI. Sixty percent were using one type of inhaler only. The range was from 1-3 types. Community Pharmacy Inhaler Check Service Patients presenting in the pharmacy to collect a prescription for an inhaled medicine are targeted for a consultation with a community pharmacist trained in the use of the In-Check DialTM device. The consultation Patient Performance – Inspiration Rate Change 400 patients had an initial inspiration rate out of the target range for their device. Over 98% of patients achieved target range by the end of their consultation. 1 MDI inspiration rate results Patient Questionnaire Results Patient feedback was positive. Patient Evaluation Would recommend service… Advice given was useful Use of inhaler has improved More confident about meds Understand more about meds Explained how medicines worked Understand more about cond 0% 20% 40% 60% 80% 100% The majority of patients using a MDI were over the target range regardless of diagnosis. Percentage of Patients Uncertain Strongly Agree Agree Disagree Strongly Disagree “Thought I was good using inhalers but learnt a lot from the pharmacist that will help me” Patient MDI use and previous inhaler instruction Recommendations for development/improvement This service should be continued and developed further to empower the pharmacist to supply a spacer with/without mask, include full assessment of condition control, follow-up consultations to monitor performance and outcomes, see patients after asthma attacks/exacerbations and develop an exacerbation management service. The data collected should be reviewed and recorded electronically and the tool thoroughly piloted to improve data collection for future evaluation. The service should be promoted. Conclusion The evaluation demonstrates the need for regular inhaler technique checks. Many patients had not achieved optimum IR for their inhaler device on initial assessment, however the community pharmacists were able to support almost all these patients to achieve the optimum IR by the end of their consultation. Community pharmacists have a key role in improving inhaler technique and inhaled medicines use, complying with recommendations made in current guidelines for asthma and COPD. A statistically significant relationship (p>0.001) was found between patients prescribed MDIs not achieving the optimum IR rate on initial assessment and reporting that they had not had any previous instruction. Condition Control There were high reports of regular preventer use from the majority of patients. Almost half of patients reported needing to use their reliever inhaler once or twice daily or more, which can be an indicator of poor condition control. The service is beneficial to patients and the wider NHS; improving inhaler use can improve condition control improving quality of life, reducing hospital admissions and even deaths, funding should continue. Interventions Provided by the Pharmacist References Sixty-three percent of patients (n=388) were given at least one intervention by the pharmacist. The most common intervention provided was inhaler instruction. There was little need to contact the GP/practice nurse. 1. Royal College of Physicians. Why Asthma Still Kills. NRAD. 2014. 2. NHS. An Outcomes Strategy for COPD & Asthma. NHS 2012. 3. NHS Doncaster CCG. 4. N.Gray NHS South Yorkshire & Bassetlaw Community Pharmacy Respiratory Project. 2013 For further information contact: doncasterlpc@gmail.com 2 3