Inhaler Check Service Training Update – Group Work Tutor
advertisement

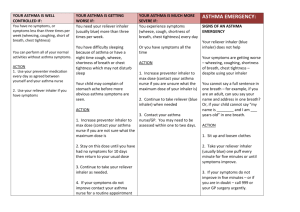
Inhaler Check Service Training Update – Group Work Tutor Notes Scenario 1: You invite a patient for a respiratory medicines use review (MUR). Information from the PMR: Male Aged 62, Salbutamol pMDI 200mcg 1-2 puffs PRN, Flixotide 250mcg accuhaler 2 puffs BD, Spiriva 18mcg capsules for inhalation 1 OD, Felodipine 5mg OD, Simvastatin 40mg ON, Co-codamol 30/500mg 1-2 qds, Amoxicillin 500mg TDS for 7 days Prednisolone 30mg for 7 days. Patient is also a current smoker. 1. What do you think is the patient’s likely respiratory diagnosis? A. Asthma B. COPD Patients age, smoking history, Rx for LAMA (Spiriva), suggest COPD. Short courses of antibiotics and oral corticosteroids suggest history of chest infections. NB: absence of a LABA with the ICS could suggest asthma however the LAMA and mucolytic are not appropriate for asthma. 2. From the patients medication history what action would you take during the MUR consultation: A. Check inhaler technique, enquire about medicine use and symptom control and discuss smoking cessation. B. Check inhaler technique, enquire about medicine use and symptom control and discuss smoking cessation. Contact GP regarding fluticasone use without a long-acting beta agonist (LABA). C. Check inhaler technique, check inspiration rate using in-check device, enquire about medicine use and symptom control, advise on purpose and use of medication, how to identify signs of an exacerbation, nutrition and smoking cessation. D. Check inhaler technique, check inspiration rate using in-check device, check for physical disability, enquire about medicine use and symptom control, advise on purpose and use of medication, how to identify signs of an exacerbation, vaccinations, nutrition and smoking cessation. E. Check inhaler technique, enquire about medicine use and symptom control and discuss smoking cessation. Review PMR history for frequency of oral corticosteroid use. 1. Check inhaler technique and inspiration rate using InCheck device – 3 different inhaler devices prescribed. When used alone a standard pMDI is rarely appropriate for older people as many have poor inhaler tech. Addition of a large volume spacer improves both acquisition and retention of drug and allows carers to assist people with cognitive or physical impairment. Some frail people cannot consistently achieve the minimum inspiratory flow rate for use of DPIs or breath actuated MDIs. 2. Co-codamol may be prescribed for OA – check for any physical disability affecting the hands. 3. An ICS should NOT be prescribed alone in COPD – pt should be referred to GP for a combination inhaler containing both ICS plus LABA. Although a clinical issue and technically out of the scope of an MUR however this does need bringing to the prescribers attention. 4. Explain that the purpose of most treatments for chronic obstructive pulmonary disease (COPD) is to control symptoms or to reduce the rate of exacerbations, but that only smoking cessation has been shown to slow the decline in lung function. 5. Stress the importance of correct use of maintenance medication. 6. Smoking cessation advice 7. Importance of vaccinations 8. Advice on nutrition – COPD patients with low BMI associated with worse outcomes. 9. Check PMR for frequent courses of oral corticosterioids – osteoporosis prophylaxis may be required. Again a clinical issue. 10.How to identify signs of an exacerbation: An exacerbation of COPD causes an acute deterioration of respiratory symptoms, particularly increased breathlessness and cough, and increased sputum volume and/or purulence. Exacerbations of COPD can be associated with the following symptoms: • Increased dyspnoea. • Increased cough; increased sputum purulence and increased sputum volume. • Upper airway symptoms (eg, colds and sore throats). • Increased wheeze and chest tightness. • Malaise. • Reduced exercise tolerance. • Fluid retention. • Increased fatigue. • Marked respiratory distress with dyspnoea and tachypnoea, acute confusion, increased cyanosis, peripheral oedema. Respiratory failure - may develop and may require non-invasive ventilation (NIV) Scenario 2: Your pharmacy technician informs you that a patient is eligible for the new medicine service (NMS) for newly prescribed inhalers. Rx: Salbutamol Easibreathe 200mcg 2 puffs BD Clenil modulate 100mcg pMDI 2 puffs BD Aerochamber device standard Patient is female, aged 26 and says her partner uses inhalers so she has an idea how to use them. 1. Which of the following best reflects what you would cover in the initial NMS consultation: A. You hand her the prescription and say you will give her a ring in a week to see how she is getting on. B. You hand her the prescription and ask her if you can arrange an appointment for her to come back in a week to see how she is getting on with the new medicines and check her inhaler technique. C. You explain that she has been prescribed two different inhalers and you need to show her how to use them. During the consultation you explain what the medicines are for, dosage regimens, possible side effects, counsel patient on inhaler technique and use the In-check device to demonstrate optimal inspiratory flow. Demonstrate use of spacer. Advise on minimising side effects, cleaning devices and check smoking status. D. You explain that she has been prescribed two different inhalers and you need to show her how to use them. During the consultation you explain what the medicines are for, dosage regimens, possible side effects, counsel patient on inhaler technique and demonstrate use of spacer. Advise on minimising side effects, cleaning devices and check smoking status. E. You explain that she has been prescribed two different inhalers and you need to show her how to use them. During the consultation you find out what the patient knows already about her diagnosis, prescribed medicines and inhaler devices and tailor your advice accordingly ensuring the patient knows; what the medicines are for, dosage regimens, possible side effects, optimal inhaler technique and optimal inspiratory flow. Advise on minimising side effects, cleaning devices and check smoking status. Patient centred consultation – find out what they know already and what they would like to get out of the consultation. Explain what the new medicines are for; salbutamol = ‘reliever’, Clenil = ‘preventer’ Dosage regimens Possible side effects How to use the Easibreathe inhaler; explain it is ‘breath actuated’, remove mouth piece, shale inhaler, hold upright & do NOT cover air holes, breathe in steadily, don’t stop breathing when the inhaler ‘clicks’ continue to breathe in slowly and deeply until lungs are full then hold breath for a count of 10. Wait several seconds before taking second dose. Replace mouthpiece cover. Demonstrate use of Clenil pMDI with aerochamber. If inhaling too quickly device will make a noise. Use InCheck dial device to demonstrate optimum inspiratory flow. Importance of rinsing mouth and spitting out after using clenil to minimise oral and systemic side effects. Wash inhalers and spacers regularly – air dry. Lifestyle advice During the consultation the patient is unable to achieve the optimal inspiratory flow rate (IR) for these devices consistently breathing in too quickly. 2. With rationale explain which of the following may be appropriate alternatives? A. Salbutamol pMDI inspiratory flow too quick + flixotide accuhaler B. Seretide accuhaler patient has been newly diagnosed with asthma patient needs a short acting beta 2 agonist – salmeterol is long acting – addition of a LABA is step 3 of treatment ladder C. Salbutamol nebs + ipratropium nebs – ipratropium SAMA not appropriate for asthma D. Salbutamol accuhaler + flixotide accuhaler – best choice both DPIs with a wider range of IR E. Ventmax MR tabs – possible option but may have systemic effects e.g. tachycardia