BLOOD TRANSFUSION If a person experiences severe
advertisement

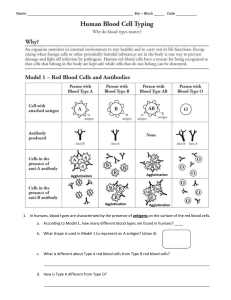
BLOOD TRANSFUSION If a person experiences severe hemorrhaging, or blood loss, as a result of an injury they can become anemic and hypotensive. Anemia is a condition that one can develop as he or she looses extreme amounts of blood and the blood left in his or her circulatory system lacks enough healthy red blood cells, commonly referred to as erythrocytes, to move throughout the blood stream. Erythrocytes bear the element Iron, which is also a component of hemoglobin, an oxygen-rich protein that allows erythrocytes to transport and bind chemicals like oxygen, and then transfer oxygen to oxygen-deficient cells through of the bloodstream. Without sufficient erythrocytes and hemoglobin in the bloodstream due to an extreme loss of blood, the cells still alive within the bloodstream will not receive enough oxygen, likely die over time, and the lack of erythrocytes will cause low blood pressure within the individual, known as hypotension. Blood transfusions are a typical procedure used to replace blood that is lost when a serious injury occurs. The procedure consists of a small needle inserted into a blood vessel through which an individual receives healthy blood. Erythrocytes contain antigens, or expressed proteins, that can be found on the surface of each of their cells. An antigen can be recognized by one’s immune system as an “intruder” if an antibody (protein), secreted by B-lymphocytes of that cell circulating through blood plasma, attaches to said antigen. Antibodies produced by a cell signal for the removal of any antigen they attach to by sending a signal to the cell’s T-cells, which remove the “dangerous/foreign” erythrocyte. Every person has a blood type of A, B, AB, or O. Some people’s erythrocytes contain an additional marker, called Rh factor, and scientists classify these cells as either “positive” (meaning it has Rh factor) or “negative” (without Rh factor). For each blood type, the antigens located on each cell are the markers of that blood type. As a result, a cell’s antibodies will correspond with its own antigens, meaning the cell will only produce antibodies through it’s B lymphocytes that can signal the destruction and removal of antigens from other erythrocytes that are not normally present on that cell’s surface. If this were not the case, antibodies produced by a cell would essentially destroy its own cell, as its antibodies would “flag” antigens that are meant to be on that blood cell and the cell’s T-cells would receive instruction to remove the antigens needed for the blood cell to survive. If a person belongs to blood group B-, she would have B antigens with anti-A and anti-Rh antibodies. If an erythrocyte is Rh positive, the recipient can receive both positive and negative blood types, but since the B- blood type lacks the Rh antigen, it cannot receive any blood with the Rh antigen because it contains an Rh antibody that would mark and remove that antigen upon arrival into the B- bloodstream. Blood transfusions will only work if the person who is going to receive blood has a group of blood cells that don’t have any antibodies that work against the donor blood's antigens. Therefore, blood type B- can only receive blood from individuals with B- blood or O- blood, because the recipient’s cells contain a B antigen and B-lymphocytes that synthesize anti-A and antiRh antibodies. “Negative” blood types can never receive from “positive” blood types because they contain Rh antigens, and negative blood types have antibodies to remove these. B- also cannot accept from A- or AB- blood types because B- blood contains anti-A antibodies. Therefore if the wrong blood type, such as O+ was injected into someone with B- blood, anti-Rh antibodies (from B- blood), secreted by B-lymphocytes, would flag the donor blood's (O +) Rh antigens and lead to an attack on the donor’s antigens. This “attack” is commonly referred to as agglutination. Through agglutination, erythrocytes labeled as “foreign” are clumped together in the presence of an antibody, as the antibody binds multiple erythrocytes together to create a large complex that can be easily removed from the bloodstream. The danger in agglutination is that agglutinated blood cells can clog blood vessels and cease circulation of the blood through the bloodstream to various parts of the body, and in reality have fatal consequences for any patient. Therefore if a friend with a B- blood type ever were to have a serious injury and need a blood transfusion, O+ blood would not be the correct blood type to infuse into your friend’s veins, and in fact, could lead to more serious physical and medical consequences.