YL7
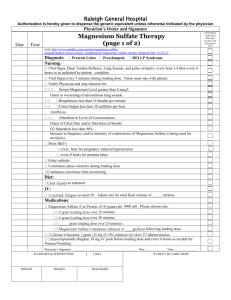
advertisement

YL7 ACUTE CARE [MEDICINE] GENERAL PRINCIPLES IN THE EMERGENCY MANAGEMENT OF AN ACUTELY POISONED PATIENT What are the 6 PRINCIPLES in the approach to the poisoned patient? Toxicology is an exaggeration of pharmacology GENERAL APPROACH I. Emergency Stabilization II. Clinical Evaluation III. Decontamination IV. Elimination of Absorbed Substance V. Administration of Antidotes VI. Supportive Therapy and Observation NOTE! The 6 principles also comprise the OUTLINE of this lecture. I. Emergency Stabilization When should you NOT give oxygen to a poisoned patient? What is the IV fluid of choice in treating poisoned patients? Maintain adequate airway Provide adequate oxygenation/ventilation - Exceptions: watusi, paraquat - Paraquat is a herbicide; forms oxygen radicals that destroy lung tissue; the more oxygen, the more lung tissue destroyed - watusi contains yellow phosphorous; smoking stool sign; do not give O2 because it ignites in body temperature Maintain adequate circulation - Starting fluids: NSS in adults, 0.3 NaCL in children - NSS: if BP is low, give isotonic fluids to bring up the blood pressure - D5 LR: can also be used. But poisoned patients are usually acidotic, you shouldn’t give lactose If a previously well patient has seizures, he has no history of epilepsy, what medication can be given as a therapeutic trial apart from the usual anticonvulsants? A. Treat convulsions Diazepam 5mg IV - Do NOT mix with D5 containing solutions—the diazepam will crystallize - Aspirate until you get blood, then inject the diazepam, then push with plain NSS Seizures of unknown origin—pyridoxine (80-120 mg/kg) - because Isoniazid is an over the counter drug, can cause convulsions by inhibition of GABA throuh inhibition of pyridoxine production - pyridoxal phosphate is essential for GABA production What is appropriate dose of naloxone in patients presenting with what appears to be a metabolic coma in the ER? B. Treat coma D50-50 - The single most common cause of decreased sensorium - Hypoglycaemia is LIFE-THREATENING! Group 08 06 March 2012 Allan R. Dionisio, MD Naloxone 2 mg IV (pedia 0.1 mg/kg) - Textbooks will tell you to give 0.2 mg IV – good for pure agonists but NOT EFFECTIVE for mixed agonist/antagonists - .4 mg dose is usually given to morphine-like opiates, for pure agonists - for mixed agonist-antagonist: 2 mg Thiamine 100 mg IV - To treat or prevent Wernicke’s encephalopathy Correct metabolic abnormalities - Electrolytes - Acid-base abnormalities II. Clinical Evaluation A. Time of Exposure Tell whether to decontaminate or not Most ingestions beyond 2 hours are not worth decontamination Clinical effectiveness of gut decontamination appears to be insignificant beyond 1 hour post-ingestion Exceptions: - Meds that slow down gut motility—ex. Loperamide - Slow release meds—ex. Verapamil SR - Enteric coated preparations—ex. Enteric coated aspirin B. Mode of exposure tells what to decontaminate must know the route of contamination C. Intake of other substances Always keep co-ingestants in the back of your mind Look for incongruences between ssx and hx more often than not, a patient can come with different toxicants, must look at history and presentation D. Circumstances prior to poisoning Get MULTIPLE testimonies Collaborate with at least 2 sources, get as many sources as you can E. Current medications and past medical of PATIENT and FAMILY Most suicidals get anything within reach Most children get anything within reach best place to look at is medicine box/cabinet F. Any home remedies taken Milk makes lipophilic toxicants get absorbed faster (ex. Benzodiazepines) Egg yolk enhances watusi/firecracker absorption Aspiration pneumonia is frequent in kerosene/hydrocarbon ingestions given household emetics - Caustic agents: can severely burn patient if patient vomits and aspirates - Paroxysms of coughing can most likely point to inhalation to lungs LENSbello KEESHduyongco anne gomez ross groves GIAN gutierrezJANINA musicoCORRINE sisoncaly tongson Page 1 of 4 GENERAL PRINCIPLES IN THE EMERGENCY MANAGEMENT OF AN ACUTELY POISONED PATIENT G. Odors One can use sense of smell to determine poison Bitter almonds—cyanide Fruity odor—DKA, isopropyl alcohol Oil of wintergreen—methylsalicylate Rotten eggs—sulphur dioxide, hydrogen sulfide Garlic—arsenic, zinc phosphide (rat poison), watusi Mothballs—camphor H. Colors Red skin—rifampicin, anticholinergics - Rifampicin: orange urine, sweat, tears, saliva if overdosed - Anticholinergics: “Red as a beet” - Aside from antihistamines, an interesting poision is Angel’s Trumpet which also has an anticholinergic effect Gray gums—lead, mercury - Other toxic effects: Abdominal colic, Gingival lines Green urine—formaldehyde Blue skin and lips—methemoglobin - Turns the blood dark because cells cannot carry oxygen Cherry red lips—carbon monoxide NOTE: Pay Attention to Autonomic SSx! I. Hypertension MNEMONIC: CT SCAN Cocaine Theophylline Sympathomimetics Caffeine Anticholinergics Nicotine J. Hypotension MNEMONIC: CRASH Clonidine Reserpine and other antihypertensives Antidepressants Sedative-hypnotics Heroin and other opiates K. Bradycardia MNEMONIC: PACED Propanolol and other beta blockers Anticholinesterases - E.g. malathione Clonidine, calcium channel blockers Ethanol Digitalis L. Mydriasis MNEMONIC: AASIA Antihistamines Antidepressants Sympathomimetics Isoniazid Anticholinergics Group08 MEDICINE M. Miosis MNEMONIC: COPS Cholinergics, clonidine Opiates, organophosphates Phenothizines, pilocarpine Sedative-hypnotics N. Toxidrome 1. Anticholinergics - Dry as a Bone - Hot as a Hare - Mad as a Hatter - Red as a Beet - Blind as a Bat 2. DUMBELS (anticholinesterases) - Diarrhea, diaphoresis - Urinary incontinence - Miosis, muscle fasciculations - Bradycardia, bronchoconstriction - Emesis - Lacrimation - Salivation use of malathione you will have a very “wet” patient manifestations of “acetylcholine gone wild!” 3. Isoniazid - Seizures - Coma - Acidosis 4. Aspirin - Mixed metabolic acidosis and respiratory alkalosis in an unknown poisoning - Tinnitus - Tachycardia O. Lab Exams 5-10 ml heparinized blood 5-10 mlclotted blood 100 ml urine Gastric aspirate All poisoning patients are potentially medico-legal, hence the importance of laboratory exams Seal the samples with candle wax III. Decontamination A. External Decontamination Dermal: Discard clothing, bathe with alkaline soap Eye: Irrigate with free flowing water for 30 minutes Avoid neutralizing solutions in caustic exposures Protect yourself! Correct dose of activated charcoal and sodium sulfate Exothermic reaction happens if you try to put base in a caustic reaction by acid Always use protective gloves in contaminating LENSbello KEESHduyongco anne gomez ross groves GIANgutierrezjaninamusicoCORRINEsisoncaly tongson Page 2 of 4 MEDICINE GENERAL PRINCIPLES IN THE EMERGENCY MANAGEMENT OF AN ACUTELY POISONED PATIENT B. Gastric Decontamination Insert NGT;Trendelenburg position Lavage with NSS NOTE these DOSAGES! (1) Activated charcoal Adults: 100 GRAMS in 200ml water Children: 1g/kg as a slurry (2) Sodium Sulfate Adults: 15 GRAMS in 100 ml water Children: 250mg/kg as a 10% solution in water Contraindications to NGT/lavage - Caustics, kerosene less than 1 ml/kg, frank convulsions Charcoal - NOTE: Not effective for alcohol, cyanide, iron, lithium, pertroleum distillates - Contraindicated in watusi and caustics Sodium Sulfate is contraindicated in: - Caustics - Ileus - Electrolyte imbalance - Patients with heart failure - Patients with kidney failure NOTE: Alternative to sodium sulfate is sorbitol 1-2 g/kg Note that you are inducing diarrhea in sodium sulfate Do not give in patients with heart failure due to sodium content Sodim sulfate is osmotic and will induce diarrhea; should not be given in patients with ileus Sorbitol, which is usual a suppository, can be given orally as an alternative for sodium sulfate Do not give charcoal for heavy metals (not effective) and caustics and watusi (you will only fuel the flame) C. Multiple Dose Activated Charcoal Adults: 50 g in 150 ml water retained in stomach q6h PO or per NGT x 48h Children: 0.5g/kg as a slurry q6h PO or per NGT x 48 hr Give sodium sulfate every morning to evacuate the charcoal Use half the dose of activated charcoal for multiple dosing When charcoal is given, water is reabsorbed; charcoal becomes a “brick” if sodium sulfate is not given Toxicants Eliminated by Multiple Dose Activated Charcoal NOTE those in BOLD. These are only the common ones which cover for 8% of the cases that we see. These toxicants undergo enterohepatic circulation Salicylates Quinine Methamphetamine and Theophylline ecstasy Amitryptilline Diazepam and other Dextropropoxyphene benzodiazepines Digitoxin and digoxin Phenobarbital Disopyramide Digoxin Nadolol Carbamazepine Phenybutazone Dapsone Phenytoin Group08 Phenobarbital Piroxicam Sotalol D. Urine PH Manipulation Alkalinize for weak acids: - Salicylates, Barbiturates , INH (isonicotinic acid hydrazide) - To alkalinize–Sodium Bicarbonate 1 meq/kg/dose until urine pH >7.5 Acidify for weak bases - Amphetamines, phenytoin, theophylline - To acidify – ascorbic acid 1g (pedia 20mg/kg) IV q6h until urine pH <5.5 No need to memorize; just NOTE the target pH Check the pKAs to determine if it is a weak acid or a weak base Usually, those with “amines” are basic E. Dialysis When do you dialyze? (includes pharmacokinetic parameters which say that dialysis is possible) 1. Low volume distribution - Low Vd means that the chemical is mostly found in the blood 2. Low protein binding 3. Toxin is dialysable 4. Benefit outweighs risks of dialysis Dialyzable Toxicants (NOTE!) - Barbiturates - Ethylene glycol - INH - Lithium - Ethanol, methanol, isopropanol - Salicylates IV. ANTIDOTES A. Pyridoxine (Vitamin B6) Specific antidote for INH poisoning Give IV bolus dose equal to amount of INH ingested If dose of INH is not known, give 120 mg/kg of pyridoxine and repeat as necessary to control seizures As much as 52g has been given safely Maintain on 10 mg/kg/d in 3dd x 6 weeks If vitamin B1/B6 combination do not give more than 1 g Vit B1 at any one bolus; repeat every 5 minutes until total required B6is given B. Atropine Physiologic antidote for cholinesterase inhibitors 1-2 mg (pedia 0.01mg/kg) IV q q15 min until: - HR > 100 - Pupils >4 mm - Dry oral mucosa - Hypoactive bowel sounds Once full atropinized, gradually increase intervals—speed of downloading the dose depends on whether carbamate or organophosphate WOF: hyperpyrexia, tachyarrhythmias, hallucinations, flushing. Stop atropine and hydrate patient until symptoms wear off. LENSbello KEESHduyongco anne gomez ross groves GIANgutierrezjaninamusicoCORRINEsisoncaly tongson Page 3 of 4 GENERAL PRINCIPLES IN THE EMERGENCY MANAGEMENT OF AN ACUTELY POISONED PATIENT MEDICINE C. Naloxone Specific antidote for opiate poisoning 2 mg IV initially. Repeat q 5 min until awake or until max of 10 mg total given Once awake, give 2/3 of the wake up dose as a drip every hour D. Flumazenil Specific antidote for benzodiazepine overdose Anexate 0.5 mg/5 ml - 0.1 mg in 4 ml D5W IV over 15 seconds q 1 min; max of 2 mg Maintain on 0.1-0.2 mg/hour as IV drip QUICK REVIEW! (1) Pyridoxine: INH Poisioning (2) Atropine: Cholinesterase Inhibitors (3) Nalozone: Opiate poisoning (4) Flumazenil: Benzodiazepine overdose V. SUPPORTIVE THERAPY AND OBSERVATION 80% of poisoned patients survive with aggressive supportive therapy alone Your management is NOT COMPLETE unless you address the PSYCHOSOCIAL factors leading to poisoning For suicidals: Counseling, co-management with psychology - If no mental health professional, you should be that professional Patients who attempt suicide deserve compassion, not ridicule or condemnation For accidental poisoning TOXICOVIGILANCE (home, workplace, community) VI. ASIDE: SPIRAL CURRICULUM go to the same stuff, learn more about it in a deeper way same slides but with variation Group08 LENSbello KEESHduyongco anne gomez ross groves GIANgutierrezjaninamusicoCORRINEsisoncaly tongson Page 4 of 4