EMCaseFacilitatorGuideVaginalBleedingCase1
advertisement

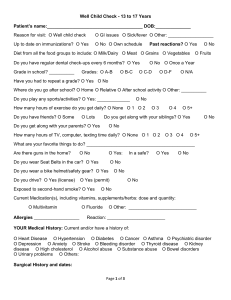
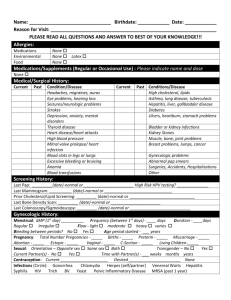
CASE: VAGINAL BLEEDING CASE 1 (MENORRHAGIA, LIKELY FIBROIDS) Tonya is a 49yo African-American female being wheeled into the ED by her daughter. She presents to triage saying she’s been having vaginal bleeding for 1 week with some cramping and feels weak. It is a weekday evening, and you are at a small ED facility where there are 24-hr onsite laboratory, limited after-hours radiology and GYN on-call consultation services available. TRIAGE QUESTIONS What are the first steps in triaging Tonya? What is necessary to assign an ESI? (N) Airway, Breathing, Circulation; objective assessment and targeted subjective questioning focusing on signs/symptoms of acuity/hemodynamic instability o Neuro – LOC, confusion, weakness? o CV – lightheaded, dizzy, palpitations? o Resp – SOB? o GYN – how many pads/tampons? LMP? Sexual activity? Possibility could be pregnant? Vital signs – orthostatics if indicated Pain assessment – (O)PQRST model as an example o Onset, provoke/palliate, quality, radiation, severity, timing Pregnancy assessment **Starting the process to determine pregnancy at triage is very important o LMP & collect urine at triage anticipating need for urine hCG o POC pregnancy test if available o If no standing protocol for RN to place urine hCG, ask provider to place order now Screening for violence, trauma ABCs are intact. Tonya reports vaginal bleeding consistently for the past week, going through 2-3 pads/hour for the past 2 days. She feels lightheaded and dizzy, has a “pounding heart”, SOB, nausea, lower abdominal cramping and weakness. Her LMP was 2 weeks ago and was heavy. She is sexually active, and when asked if she could be pregnant, she says “Oh no, I’m too old for that.” Tonya screens negative for violence or trauma. VS: T 97.8, HR 110, BP 105/50, RR 28, 96% on room air Pain: 2/10, crampy ache, non-radiating, started with bleeding and constant since What ESI (Emergency Severity Index) level would you assign Tonya and why? (N) ESI = 2, based on vaginal bleeding, SOB and tachycardia Is there any other information important to gather at triage? (N) EKG – based on her SOB and HR 110 What would you communicate to the primary nurse? How would you orient Tonya & her daughter to the next steps of care? (N) Communication to primary nurse – verbal is necessary given high risk (ESI 2), but may only use EDIS (electronic patient tracking system) o Example: “Female, CC: heavy vaginal bleeding and abdominal pain x 1 week, tachycardic, tachypneic” o Need for private, monitored, highly visible treatment room capable for pelvic exam Communication to Tonya/daughter o Need for urine sample; need to assess for pregnancy o Taking to private ED treatment room; need to change into gown; offer pads/chux o Plans for blood work and pelvic exam o Inform staff if feeling worse o All in compassionate, non-judgmental manner 1 PRIMARY NURSE ASSESSMENT Once triaged, what nursing steps should occur before initial provider assessment (i.e. care, assessment)? (N) Nursing care o Immediate resuscitative actions – 2 large bore IVs, O2, monitor o Anticipate next steps/Nursing protocoled orders Urine, for hCG and UA (if not obtained in triage) Blood work, obtain appropriate color-top tubes (T&S, CBC, CMP, coags, ?β-hCG) IVF ready Prepare for pelvic exam (supplies, equipment, chaperone, etc.); change into gown Nursing assessment o Additional HPI, focused ROS o Targeted OB/GYN history Gravida/Para When was last sexually active? Method of contraception? Hx previous ectopic pregnancy? hx previous STI? o Screening for violence/trauma (if not done at triage) o Medication review, allergy assessment o Reassessment from triage findings Tonya was placed in monitored treatment room and changed into a gown. On your initial nurse assessment, you note a middle-aged woman, laying on a gurney in mild-to-moderate distress. She appears fatigued and pale. She says she felt really dizzy when she was getting into the gown and feels like she has to stay lying down. Her daughter is present. On additional questioning, she is G2P2 (both vaginal deliveries), no history of ectopic pregnancy or STIs. She is sexually active with 1 male partner and they do not use contraception. VS reassessment reveals HR 135, BP 86/42, RR 26, 95% on RA What would you communicate with the provider? (N) Notify provider of immediate needs Update provider on changes in condition since triage Summarize pertinent findings (SBAR approach is one example of systematic way to provide report) Example “Tonya is a 49yo female in room 3 for vaginal bleeding for 1 week, heavy for past 2 days. She was tachycardic and tachypneic at triage; now she’s more symptomatic. Her SBP dropped from 98 to 86 and HR increased from 110 to 135. I have the crash cart at the bedside, O2 going, on a monitor, placed 2 large bore IVs, and NS IVF ready to start.” The provider orders IVFs and after 500cc NS on a pressure bag and with Tonya lying flat and feeling slightly better VS reassessment reveals HR 105, BP 98/52, RR 20, 99% on 2L NC The provider is now in to assess Tonya. PROVIDER ASSESSMENT What historical questions would you ask Tonya during your assessment? (P) See question list below Targeted HPI & ROS (to complement what has already been asked/obtained) Medical and surgical histories OB/GYN history, including menstrual & sexual histories Family history – cancer, coagulopathy, CAD 2 Social history – tobacco, illicit drugs, alcohol Appropriate questions to ask for vaginal bleeding history: 1. LMP? Was it normal? Are periods regular? 2. Onset of bleeding? 3. Duration of bleeding? 4. # soaked pads or tampons/hour? 5. Any tissue or clots passed? 6. Vaginal discharge or fluid other than blood? 7. Pain? cramping? back pain? 8. OB history: G___ (# of pregnancies, vaginal or C/S) P___ (#live births) AB____(# abortions – spontaneous/elected) 9. History of previous ectopic pregnancy? 10. Are you sexually active? With men, women or both? When were you last sexually active? 11. History of sexually transmitted infections? 12. Method of contraception: oral contraceptives, implant, *tubal ligation, *IUD, barrier. Used consistently? 13. Attempting to get pregnant/fertility treatment? 14. Any recent GYN procedures? 15. Last meal? 16. Allergies? 17. Medications? (specifically ASA, warfarin, etc.) *confers increased risk for ectopic pregnancy What elements of the physical exam would you perform? What key findings are you looking for? (P) Physical exam with pelvic exam; pelvic exam to specifically evaluate for o Signs of trauma o Quantification of bleeding o Presence of clots/tissue o Pelvic organ tenderness or mass How do you prepare for the pelvic exam? How do you prepare Tonya for the pelvic exam? (N&P) (N) Gather and set-up supplies and equipment o Appropriate room and exam table o Proper positioning of patient o Collection basin/chux o Light source, speculums, lubrication, swabs, gauze, loop forceps, vaginal pack, specimen collections (N&P) Ensure appropriate female chaperone (N&P) Attend to privacy o Private room, exam table with foot of bed away from door, pull curtain, sign on door/locked door o Appropriate gowning and draping (P) Explanation of pelvic exam process, obtain verbal consent (N&P) Allow Tonya to empty bladder While the provider is assessing Tonya, the female nurse is gathering supplies for the pelvic exam (detailed above). 3 Tonya tells the provider she’s been passing clots for 2 days, but no tissue. No vaginal discharge. ROS is confirmed from nurse assessment, but Tonya and says that her SOB seems to be getting better since she’s been here. She has no past medical nor surgical histories, no recent GYN procedures. She’s allergic to penicillin. She takes only vitamin D. She last ate 6 hours before coming. Her family history is non-contributory, and she denies tobacco, alcohol or drug use. The nurse relays negative pregnancy test results. The female nurse serves as the chaperone, supplies are ready, exam steps have been described, and Tonya has given verbal consent for pelvic exam. Her privacy has been attended to. Physical exam (provide elements requested) GEN: fatigued and pale, mild distress, but A&O HEENT: OP clear, conjunctival pallor, dry mucous membranes CV: tachycardic, regular rhythm, 3/6 systolic murmur heard throughout precordium PULM: CTAB ABD: soft, non-distended, diffuse lower abdominal tenderness, no rebound or guarding, no CVAT, no HSM PELVIC: External inspection: normal external genitalia, no lesions, no signs of trauma Speculum: moderate bleeding visible at introitus, using swabs and gauze to clear blood and clots shows moderate bleeding from a closed cervical os, Bimanual: no CMT, bulky enlarged mildly tender uterus to ~12 week pregnancy, no adnexal tenderness, no masses RECTAL: no bleeding SKIN: pallor NEURO: non-focal, GCS-15 Vaginal packing is placed How would you summarize your findings and plan to Tonya? (P) Key exam findings Concerns Next steps in care Example “Tonya, my concerns are that you are showing signs of blood loss causing your low blood pressure and fast heart rate. I noticed on your pelvic exam that you are still bleeding quite heavily with some tenderness when I touch your uterus. Your uterus is also a bit larger that expected. For all of these reasons, I’d like to send your blood work for testing and there’s a strong chance that you’ll need a blood transfusion. I put some gauze in your vagina to control the bleeding, so if you notice any leaking, please let the nurse know. I’m going to touch base with the gynecologist to get their opinion. We’ll also plan to admit you to the hospital for observation and more testing.” WORKING DIFFERENTIAL DIAGNOSIS AND EVALUATION What is your differential diagnosis? What is your lead/working diagnosis and why? (P) Prioritize life, limb or fertility threats o Symptomatic anemia: GYN – menorrhagia (fibroids, aborting fibroid, polyp); lead diagnosis HEME/ONC– coagulation disorder, malignancy o Hemodynamic instability: CARDIAC – ACS 4 Based on the working differential diagnosis of the provider, what would you anticipate being ordered? (N) Blood work (appropriate color-top tubes already collected) Blood products UA (urine already collected) Imaging GYN consult Keep NPO for possible surgical need What is your approach to narrowing your differential diagnosis? What key exam findings help you; what labs, and/or imaging would you obtain? (P) Key exam findings o Atraumatic o Moderate bleeding from closed os o Bulky enlarged mildly tender uterus to ~12 week pregnancy Labs – CBC, coags, CMP, T&C, UA, cardiac enzymes Imaging (recall your facility has limited after-hours radiology, including US) o CXR o TVUS – Does anybody feel an emergent TVUS is indicated which may mean transfer? What would it tell you? What wouldn’t it tell? Would this change your management? In this case, TVUS can be ordered, but it isn’t emergent (based on presentation & exam findings) and could be pursued in the morning. o CT or MRI – indication for these? What would they tell you? TVUS preferred, but not emergent o Indications for emergent imaging includes: Evaluation for ectopic pregnancy, tubo-ovarian abscess, ovarian torsion, significant pain, etc Results are as follows: WBC 10,000 Hgb 7.4 Hct 21.2 Platelets 350,000 INR: 1 Na 136 Cl 97 HCO3 23 K 4.2 BUN/Cr 13/0.9 Glucose 101 Cardiac enzymes: negative MANAGEMENT How do you interpret the labs? (P) Symptomatic anemia (suspected acute; as Hgb/Hct 3 years ago was 13.2/39) What are your next steps in the ongoing management of Tonya? (P) Support hemodynamics Obtain consent and order to transfuse 2 units PRBCs GYN consultation What information do you communicate to the consultant? (P) 49 yo female with vaginal bleeding and symptomatic hypotension, tachycardia, SOB EKG without ischemic changes, cardiac enzymes negative 5 LFTs normal UA: 3+ blood o/w negative T&C 2 units PRBC CXR: negative Exam shows moderate vaginal bleeding which was packed, minimal pelvic organ tenderness, ~12 week-size bulky uterus Hemoglobin is 7.4 and she is being transfused with 2 units PRBCs; normal platelets and coags Patient is responding to IVF and blood products What are your next steps in the ongoing management of Tonya? (N) Reassess – including check vaginal packing Support hemodynamics – IVF, transfuse PRBC, recheck H&H Update provider to status and response to treatment How would you summarize the plan of care to Tonya and her daughter? (N) Ongoing need for reassessments, including vaginal packing checks Transfusion and post-transfusion labs GYN consult Provider working diagnosis After 1L NS and the first of 2 units PRBCs, Tonya continues to report feeling better. Her vaginal packing was changed once by the provider. VS Reassessment reveals HR 100, BP 102/60, RR 18, 99% on 2L NC GYN consult – agree with resuscitation, transfusion, and vaginal packing. Recommend IV estrogen, keep NPO, GYN will be in to evaluate and repeat pelvic exam. Plan for admission. *Treatment considerations: -if there was an embolic history, would avoid IV estrogen and favor provera -if significant N/V, may avoid high-dose OCPs or may need antiemetic prior -amount of bleeding may influence IV vs PO treatment; also anticipation of procedure would influence avoiding PO IV estrogen is started in the ED based on dosing recommendations from GYN. GYN is expected within the hour. HANDOFF/DISPOSITION What are the proper handoff procedures in this scenario? (P&N) Admission criteria based on hemodynamic instability, need for continuous monitoring, potential intervention, further workup (P) Admission process followed (P&N) Reassessment, update provider to changes (N) Verbal report to accepting service (P&N) Communicate plan to Tonya and daughter (P&N) Tonya was admitted to the General Medicine unit with GYN consultation and had an uncomplicated 3-day inpatient admission. Her bleeding stopped with IV estrogen. She did not require additional blood products. She had a TVUS which demonstrated multiple submucosal and subserosal uterine fibroids. Tonya underwent an endometrial biopsy which was negative. Uterine fibroids were the suspected cause of her menorrhagia and resultant symptomatic anemia. She was placed on combined oral contraceptive therapy and will follow-up with GYN as an outpatient for discussion of further treatment options. 6 KEY LEARNING POINTS – VAGINAL BLEEDING CASE 1 Unstable patients should be identified immediately, triaged appropriately and placed in a resuscitative bed All female patients with abdominal pain, pelvic pain, and/or vaginal bleeding who are <52 years of age should have pregnancy assessed at triage Life and fertility threatening conditions must be recognized Emergency providers should perform a pelvic exam prior to specialty consultation when a patient complains of vaginal bleeding When performing a pelvic exam, adhering to patient dignity, privacy and appropriate female chaperone requirements are crucial It is important to ensure adequate pelvic exam set-up and anticipate the need for additional supplies (i.e. vaginal packing) in the setting of heavy vaginal bleeding Not all acute vaginal bleeding warrants an emergent TVUS; indications include evaluation for ectopic pregnancy, tuboovarian abscess, ovarian torsion, significant pain, etc. The plan of care should be effectively communicated to patient and family as well as among ED staff throughout the encounter 7