Objectives
advertisement

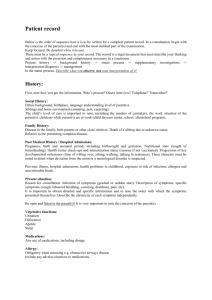
Objectives At the conclusion of MD5 course, students at all locations should be able to: Medical Interviewing Review basic interviewing skills Learn advanced interviewing skills Alcohol and substance use history Interviewing with an interpreter Sexual history Problem-focused interviewing Review of Organ Base Syatems Physical Exam Review the basic physical exam Learn the advanced physical exam for: Vital Signs Skin (in Dermatology) HEENT and neck Chest and lungs Breast Cardiovascular Abdomen Pelvic Musculoskeletal Neurologic Psychiatric Male genital and rectal Documentation Review format for recording the medical database Problem list Complete medical database – complete H & P Focused (SOAP) notes Review the organization of the inpatient and outpatient medical record Clinical Reasoning Review principles of clinical reasoning Learn clinical reasoning tools Differential diagnosis Branching diagrams Application of clinical epidemiology Learn to integrate clinical reasoning with data gathering and case presentation Clinical Procedures IV CPR thorancetesis lumbar puncture Suturing Oral Case Presentations Learn the organization and content of the full oral case presentation Learn other types of case presentations Problem focused case presentation (e.g. clinic visit) Very brief case presentation (e.g. consultation request) Professional Development Review core professional values Altruism Reliability Excellence, scholarship, and commitment to self directed learning Honor and integrity Compassion Leadership Respect for patients and for colleagues Learn about the impact of uncertainty and mistakes in medical practice Review the principles of medical ethics Review the professional boundaries between patients and physicians Learn how to care for yourself as you care for patients Learn how to use Evidence Based Medicine Special Topics Learn about: Care of patients with disabilities Care of patients of different cultural and ethnic backgrounds Complementary and alternative medicine Health issues related to human sexuality Caring for patients with life-threatening and terminal illness Pediatric communicatio About the Program Introduction to Clinical Medicine expresses the strongly patient-centered orientation of the medical school curriculum. The student is introduced to patients and is involved in patient care activities from day one. Students are introduced to the principles of patient care and management and examine what it means to be a physician and how one becomes a physician. The major content areas of the course include communication in the setting of illness, the unified concept of health and disease (the biopsychosocial model), basic clinical skills and the correlation of basic science with clinical medicine. ICM emphasizes the systematic acquisition of the clinical skills of interviewing, history taking, physical examination, elementary clinical problem solving and medical record keeping. Throughout the Year I-II continuum, the ICM clinical skills curriculum is integrated with basic science instruction. Students can therefore learn and apply basic science knowledge in the clinical setting. By encouraging a thorough understanding of the direct applications of basic science research to modern clinical medicine, instructors motivate the student to learn, use and retain more of the content and concepts presented in the basic science portions of the curriculum. A group of five or six students spends from four to eight hours each week with an instructor from the clinical faculty who remains with the group for one to two years. As the group deals with basic medical themes (death, pain and helplessness) and issues (patient responsibility, learning to live with ambiguity and uncertainty), instructors help students to cope with their own feelings. This format opens the door for student-faculty interaction and improvement of student-faculty communication. Instructors encourage students to take advantage of the learning experiences provided by their roles as helping and therapeutic persons. Students develop their ability to communicate with patients in the setting of illness and are guided by patient concerns to enhance their own growing knowledge, skills, abilities and responsibilities. Students are expected to acquire skills and habits of self-education and self-instruction which will prepare them for lifelong learning. The unified concept of health and disease presented in this course enables the student to comprehend the human organism in all its complexity. Using their clinical experiences as a teaching model, students are taught to consider the patient as an integrated whole and to view the patient's illness or disease as more than simply a disruption of physiologic processes or a collection of physical findings. Additional learning experiences occur through workshops and focus experiences. ICM workshops provide standardized instruction in history taking and physical examination, as well as integrated instruction in areas which cross disciplines. These include adolescent health, use of interpreters, patient education and ethics. Through focus experiences, students are encouraged to explore a variety of practice environments as well as community-based health and social services. For example, students may visit outpatient clinical settings, a geriatrics longterm care facility, a hospice care facility or homeless services organizations. Mission Statement Introduction to Clinical Medicine (ICM) is an interdisciplinary course extending over the first two years of medical school that is designed to emphasize patient-centered medical care. Through a focus on the unified concept of disease, the student will gain an understanding of himself/herself as a developing physician in relation to the patient. Our mission is to develop students who consider the patient as an integrated whole and who acquire competence in the basic clinical skills of medical interviewing and physical exam. Goals of the Program The principle goals of the ICM program are to 1) help the student understand disease and begin to develop clinical competence in medical interviewing and physical examination skills and 2) to understand patients and their experiences of illness in the context of the unified concept of health and disease – that in every illness in every patient there are biological, socioeconomic, cultural, psychological and emotional components. We aim to counteract the potentially dehumanizing effect of the student-to-physician process by favoring an approach to medicine that stresses a patient-centered rather than diseasecentered approach to medical care. We believe that to practice sound, scientific medicine one must go beyond the molecular level and organ system to better understand and work with the individual patient in the context of his or her family and the larger community. Program Curriculum The Introduction to Clinical Medicine (ICM) Program extends over the first two years of training in the Keck School of Medicine at the University of Southern California. ICM is an interdisciplinary course designed to emphasize the patient-centered orientation of the curriculum. Attitudes, knowledge and clinical skills in ICM are taught within the framework of the following program goals and objectives which are meant to make a significant contribution to each student’s achieving of the Keck School of Medicine’s “Educational Program Objectives.” Program Goals 1. Introduce students to the unified concept of health and disease – that in every illness in every patient there are biological, socioeconomic, cultural, psychological and emotional components. 2. Provide opportunities for students to interact with patients, peers and faculty to foster development of communication skills, clinical skills and professionalism. 3. Provide patient care experiences that correlate with basic and behavioral science to foster development of an integrated knowledge base and the skills of clinical decision making. Program Objectives By the end of the two-year continuum, in the context of the ICM Program Goals, students should be able to: 1. Demonstrate sensitivity to the feelings and attitudes of patients and families in all patientstudent physician interactions. 2. Participate fully in all small-group activities demonstrating effective communication with peers, faculty and patients. 3. Elicit a medical history and perform an accurate, complete and sensitive physical examination, and to interpret specified abnormal physical findings. 4. Demonstrate proper written documentation of a history, physical examination, problem list, summary, initial plans and case discussion. 5. Present the medical history and physical examination verbally in both formal and summary fashions. 6. Demonstrate professionalism through consistent performance in developing clinical skills, completion of milestones, timely submission of all requested assignments and evaluations and full participation in all required activities. Year I Weekly ICM sessions: The course is taught in the setting of a small group of students and an instructor from the clinical faculty. The groups work with patients in a variety of clinical settings in which each student will have numerous opportunities to interview patients either on a one-on-one basis, with a student partner or with the entire ICM group together. The instructor will sit in with one student during each morning session and give an evaluation to that student. Students will learn to develop skill and sensitivity in interviewing patients with the objective of obtaining all the important data concerning the patients' major problems, while developing a deeper understanding of the impact of illness in their patients’ lives. Students will learn to present verbally a summary of the interview, presenting the major organic and psychosocial problems in the small group discussions. They will have an opportunity to discuss difficult points in the interview in a post interview session facilitated by the instructor. Later in the ICM continuum, students will also learn to examine patients while remaining respectful of their privacy and sensitive to their possible discomfort. Using the patient as the stimulus for discussion, basic medical themes are woven into the discussion of individual patients after each student interview. For example, in the student's encounter with the terminally ill patient, the student learns to recognize the physical and emotional needs of the patient, and at the same time is helped to become more aware of his own feelings and attitudes about death and dying, pain and suffering. Students are encouraged to develop these themes in their discussions of their pathients and are helped to develop adaptive solutions dealing with many of these critical issues in their professionalization. Students will also learn to correlate patient care experiences with basic and behavioral science. Using the patient as the impetus for learning, students will recognize and describe relevant basic and behavioral science information. Year I Afternoon workshop sessions: ICM is also scheduled on selected Thursday afternoons throughout the year. The workshops focus on certain aspects of interviewing or important clinical themes. Among the workshops, there is a series of Interviewing Techniques Workshops during which students will have an opportunity to practice their interviewing skills with standardized patients, under the guidance of their clinical instructors. There is also a series of system-based workshops where students will learn specific interviewing and physical examination skills referable to the particular organ system. 1. main symptoms of internal diseases. An introductory lecture to the course of propedeutics of internal diseases. Importance of history taking for making correct diagnosis. Segments of patient´s history. Main symptoms and signs of internal diseases. Pain. Dyspnoe. Cough. Palpitations. Nausea and vomiting. Constipation. Diarrhoe. Recquired knowledge: anatomy, physiology 2. Overall condition of the patient, the state of consciousness. Mental state of the patient, consciousness, growth, nutrition, standing and walking and their disturbances, voice and speech and their disturbances, body temperature measurement and different types of temperature curves. Recquired knowledge: anatomy, physiology 3. Findings on the skin. Physical examination of the head and the neck (part I). Examination of the skin - colour, tonus, moisture, temperature, affections. Hair and nails. Shapes of head, hair cover, face, eyes, nose, mouth and throat. Physical examination, normal findings. Recquired knowledge: anatomy, physiology of skin, head and neck 4. Physical examination of the head and the neck (part II). Physical examination of the eyes and the throat. Examination of eyes, eyelids, nose, mouth, throat. Inspection, percussion, palpation, auscultation. Mobility of the neck, vessels, lymfatic nodes, thyreoid gland. Pathological findings. Recquired knowledge: anatomy, physiology of head and neck 5. Symptomatology of the cardiovascular diseases. Physical examination of the heart (physiological findings). History, important complaints. Changes in chest shape, inspection, percussion. Finding the heart borders. Palpation, auscultation - physiological findings. Recquired knowledge: anatomy, physiology of circulation 6. Physical examination of the heart (physiological findings - part II), pathological findings. Auscultation of the heart, basic heart sounds, extra sounds, murmurs. Physiological and pathological findings. Blood pressure measurement. Recquired knowledge: anatomy, physiology of circulation 7. Acquired and congenital heart diseases in the adults. Heart valve disease - mitral stenosis, mitral regurgitation, aortic stenosis, aortic regurgitation - clinical presentation, physical examination. Congenital heart defects septal defects, Fallot´s tetralogy, Ebstein´s anomalia, ductus arteriosus persistens, coarctation of the aorta. Clinical presentation, physical examination. Recquired knowledge: anatomy, physiology of circulation 8. Symptomatology of the pulmonary diseases. Physical examination of the lungs (physiological findings). Physical examination of the lungs - observation (changes in chest shape), palpation, percussion, auscultation. Recquired knowledge: anatomy, physiology of ventilation 9. Physical examination of the lungs (physiological findings - part II), pathological findings. Pathological findings during physical examination. Effusions, inflammation, oedema. Recquired knowledge: anatomy, physiology of ventilation 10. Symptomatology of the gastrointestinal diseases. Physical examination of the abdomen (physiological findings). Inspection, percussion, auscultation, palpation and per rectum examination. Superficial and deep palpation. Importance of excellent knowledge of normal findings to be able to recognize pathology. Importance of history. Recquired knowledge: anatomy, physiology of gastrointestinal tract 11. Physical examination of the abdomen (physiological findings - part II), pathological findings. Inspection, percussion, auscultation, palpation and per rectum examination. Superficial and deep palpation. Importance of excellent knowledge of normal findings to be able to recognize pathology. Importance of history. Recquired knowledge: anatomy, physiology of gastrointestinal tract 12. Physical examination of the abdomen (pathological findings). Physical examination, pathological findings. Important complaints: pain, dyspepsia, dysphagia, pyrosis, bowel movement disorders. Recquired knowledge: anatomy, physiology of gastrointestinal tract 13. Symptomatology and affections of the limbs. Physical examination of the limbs. Common complaints. Oedemas, claudications, rest pain, trophical changes. Inspection, palpation, auscultation. Examination of joints and mobility. Upper and lower extremities. Recquired knowledge: anatomy, physiology of limbs 14. Examination methods in cardiology. History, common complaints. Physical examination. ECG, echocardiography, stress examination. CT and MR imaging. Biochemical markers. Recquired knowledge: anatomy, physiology of circulation 15. Basics of electrocardiography. Recording the ECG. Reading and interpretation of ECG records. Basic dysrrhytmias, disturbances of conduction, acute and chronic ischaemic changes. Recquired knowledge: anatomy, physiology of circulation 16. Examination methods in gastroenterology and hepatology. History, common complaints. Physical examination. Ultrasound, X-ray, CT and MR imaging. Endoscopic and biochemical methods. Recquired knowledge: anatomy, physiology of gastrointestinal tract 17. Examination methods in endocrinology - clinical presentation, basic examination, differences in adult patients. History, common complaints. Clinical presentation and examination of basic disturbances. Ultrasound, CT and MR imaging. Biochemical markers and tests. Differences in children and adult patients. Recquired knowledge: anatomy, physiology of glands