Supplemental Digital Material Tables Table 1. Level of Evidence
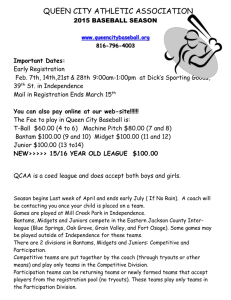
advertisement

Supplemental Digital Material Tables Table 1. Level of Evidence grade for studies comparing fusion with multidimensional supervised rehabilitation in CLBP patients with or without isthmic spondylolisthesis. Methodological Principle Brox Fairbank Fritzell Möller Study design Randomized controlled trial Cohort Study Case-series Statement of concealed allocation* Intention to treat* Independent or blind assessment Co-interventions applied equally Complete follow-up of >80% Adequate sample size Controlling for possible confounding Evidence Level † I I II II *Applies to randomized controlled trials only †Fritzell: while the intention to treat principle was used to analyze the differences between treatment groups, group changers and drop outs were excluded from all reported data. Because we used the raw data to calculate SMDs and RDs, we did not give credit. Table 2. Results of studies comparing fusion with rehabilitation in patients with CLBP with and without isthmic spondylolisthesis. Fusion Study Outcome N (%) or pre and post score Change score (CS)* Multidimensional supervised rehabilitation N (%) or Change score pre and post (CS)* scores With isthmic spondylolisthesis Möller (2000)/ Eckman (2005) Disability Rating Index† Pain (VAS)§ Patient-perceived outcome (much better or better) Clinician-perceived outcome (much better or better) At-work Pre: 48 ± 4.4‡ 1 yr: 29 ± 5.9‡ 2 yrs: 29 ± 5.8‡ 9 yrs: 33 ± 5.6‡ Pre: 63 ± 4.7‡ 1 yr: 35 ± 6.9‡ 2 yrs: 37 ± 7.2‡ 9 yrs: 40 ± 6.7‡ 2 yrs: 74% (56/75) 9 yrs: 82% 2 yrs: 73% (55/75) 9 yrs: NR Pre: 25% (19/77) 1 yr: 46% 2 yrs: 54% (41/75) 9 yrs: 51% 1 yr: 19 2 yrs: 19 9 yrs: 15 1 yr: 28 2 yrs: 26 9 yrs: 23 n/a n/a 1 yr: 21% 2 yrs: 29% 9 yrs: 26% Pre: 44 ± 6.2‡ 1 yr: 45 ± 8.8‡ 2 yrs: 44 ± 7.3‡ 9 yrs: 38 ± 9.5‡ Pre: 65 ± 7.4‡ 1 yr: 54 ± 9.7‡ 2 yrs: 56 ± 7.7‡ 9 yrs: 49 ± 10.4‡ 2 yrs: 43% (13/31) 9 yrs: 66% 2 yrs: 23% (7/31) 9 yrs: NR Pre: 38% (13/34) 1 yr: 48% 2 yrs: 55% (17/31) 9 yrs: 46% 1 yr: -1 2 yrs: 0 9 yrs: 6 1 yr: 11 2 yrs: 9 9 yrs: 16 n/a n/a 1 yr: 10% 2 yrs: 17% 9 yrs: 8% Without isthmic spondylolisthesis Brox (2003) ODI General function score Back pain (VAS) Leg pain (VAS) Emotional distress Life satisfaction Patients overall rating of success Physician overall rating of success Working full-time Fairbank (2005) ODI ODI: Chronic back pain pts only SF-36 physical SF-36 mental Fritzell (2001) Back pain (VAS) Leg pain (VAS) n = 35 Pre: 42.0 ± 11.0 1 yr: 26.4 ± 16.4 Pre: 35.9 ± 18.6 1 yr: 18.3 ± 17.3 Pre: 62.1 ± 14.5 1 yr: 39.4 ± 25.5 Pre: 43.5 ± 27.7 1 yr: 26.6 ± 28.1 Pre: 1.8 ± 0.5 1 yr: 1.5 ± 0.4 Pre: 5.4 ± 2.4 1 yr: 6.2 ± 2.4 1 yr: 71% (25/35) 1 yr: 69% (24/35) Pre: 26% (9/35) 1 yr: 23% (8/35) n = 138 Pre: 46.5 ± 14.6 2 yrs: 34.0 ± 21.1 n = NR Pre: 46.7 ± 14.5 2 yrs: 33.3 ± 20.8 n =115 Pre: 19.4 ± 8.8 2 yrs: 28.8 ± 14.9 n = 115 Pre: 43.2 ± 10.9 2 yrs: 47.4 ± 12.2 n = 195 Pre: 64.2 ± 14.3 2 yrs: 43.2 ± 25.2** n = 192 Pre: 35.3 ± 25.4 2 yrs: 29.0 ± 27.0** 1 yr: 0.8 n/a n = 26 Pre: 43.0 ± 13.0 1 yr: 29.7 ± 19.6 Pre: 44.6 ± 13.7 1 yr: 22.6 ± 18.9 Pre: 64.1 ± 13.7 1 yr: 48.7 ± 24.0 Pre: 34.0 ± 19.3 1 yr: 35.5 ± 30.6 Pre: 1.9 ± 0.6 1 yr: 1.6 ± 0.5 Pre: 4.8 ± 2.0 1 yr: 6.6 ± 2.1 1 yr: 65% (17/26) n/a 1 yr: 77% (20/26) 1 yr: 15.6 1 yr: 17.6 1 yr: 22.7 1 yr: 16.9 1 yr: 0.3 1 yr: -3% 2 yrs: 12.5 2 yrs: 13.4 2 yrs: 9.4 2 yrs: 4.2 2 yrs: 21.0 2 yrs: 6.3 Pre: 23% (6/26) 1 yr: 35% (9/26) n = 146 Pre: 44.8 ± 14.8 2 yrs: 36.1 ± 20.6 n = NR Pre: 45.4 ± 15.2 2 yrs: 37.2 ± 21.1 n =131 Pre: 20.0 ± 9.7 2 yrs: 27.6 ± 14.6 n = 131 Pre: 44.2 ± 12.6 2 yrs: 48.1 ± 12.6 n = 62 Pre: 62.6 ± 14.3 2 yrs: 58.3 ± 18.8** n = 59 Pre: 35.6 ± 25.2 2 yrs: 42.6 ± 24.8** 1 yr: 13.3 1 yr: 22.0 1 yr: 15.4 1 yr: -1.5 1 yr: 0.3 1 yr: 1.8 n/a n/a 1 yr: 12% 2 yrs: 8.7 2 yrs: 8.2 2 yrs: 7.6 2 yrs: 3.9 2 yrs: 4.3 2 yrs: -7.0 Fusion Study Outcome ODI MVAS GFS Zung Return to work†† Patient-perceived rating (% improved)‡‡ Physician-perceived rating (excellent or good) Physician-perceived rating (excellent, good, or fair) Willing to go through again N (%) or pre and post score n = 197 Pre: 47.3 ± 11.4 2 yrs: 35.7 ± 18.0** n = 197 Pre: 63.7 ± 11.3 2 yrs: 45.6 ± 23.1** n = 194 Pre: 49.1 ± 15.9 2 yrs: 34.1 ± 22.4** n = 191 Pre: 39.1 ± 13.3 2 yrs: 31.4 ± 15.2** 2 yrs: 36% (57/160)** Change score (CS)* Multidimensional supervised rehabilitation N (%) or Change score pre and post (CS)* scores 2 yrs: 7.7 n/a n = 62 Pre: 48.4 ± 11.9 2 yrs: 45.6 ± 16.1** n = 61 Pre: 65.5 ± 11.5 2 yrs: 60.4 ± 17.2** n = 61 Pre: 47.6 ± 16.3 2 yrs: 45.5 ± 20.3** n = 61 Pre: 39.4 ± 13.9 2 yrs: 36.7 ± 14.5** 2 yrs: 13% (6/48)** 2 yrs: 62.6% (122/195)** n/a 2 yrs: 29.0% (18/62)** n/a 2 yrs: 45.5% (91/200)** n/a 2 yrs: 17.7% (11/62)** n/a 2 yrs: 78.0% (156/200)** n/a 2 yrs: 58.0% (36/62)** n/a 2 yrs: 75.1% (145/193)** n/a 2 yrs: 52.6% (30/57)** n/a 2 yrs: 11.6 2 yrs: 18.1 2 yrs: 15.0 2 yrs: 2.8 2 yrs: 5.1 2 yrs: 2.1 2 yrs: 2.7 n/a GFS: General Function Score; JOAS: Japanese Orthopedic Association Score; MVAS: Million Visual Analogue Score; n/a: not applicable; NR: not reported; ODI: Oswestry Disability Index; VAS: Visual Analogue Scale *Change score = post score – pre score; for outcome measures where a lower score represents a better outcome, the change score is multiplied by -1 so that a positive score always represents improvement. †Disability Rating Index (DRI): functional outcome score represents the mean of 12 VAS items: dressing, outdoor walking, climbing stairs, sitting for longer time, standing bent over a sink, carrying a bag, making a bed, running, light work, heavy work, lifting heavy objects, and participation in exercise or sports. Scores range from 0 (without difficulty) to 100 (impossible) mm. ‡Standard deviation calculated using the mean and 95% confidence interval as reported in the study. §Pain VAS reflects the overall pain index and does not distinguish between back and leg pain. The pain index was calculated by taking the mean of the VAS for “pain right now” and that for “worst pain last week”. Scores range from 0 (no pain) to 100 (intolerable pain) mm. **Data reported excluded group changers and dropouts (surgical: n = 201; nonsurgical: n = 63); although the authors included group changers were included in the test for interaction (NR). ††Return to work calculated by subtracting the number of patients who stopped working from those who went back to work; excludes patients who were on full time pension/ disability pension (surgical: n = 160; nonsurgical: n = 48). ‡‡Patient-rated improvement (“much better” or “better”) or no improvement (“unchanged” or “worse”) of back problems Table 3. Articles excluded Study Reason for exclusion Athiviraham 2007 Brox 2006, 2010 Chang 2005 1 degenerative spondylolisthesis and stenosis 2,3 prior surgery and or stenosis 4 stenosis with or without HNP Ghogawala 2004 5 degenerative spondylolisthesis and stenosis 6 Herkowitz 1991 Maine Lumbar Spine Study Atlas 1996, 2000, 20057-9 Malmivaara 200710 degenerative spondylolisthesis and stenosis degenerative spondylolisthesis and stenosis Matsudaira 200512 degenerative spondylolisthesis and stenosis no supervised rehabilitation, fusion versus laminectomy or discectomy degenerative spondylolisthesis and stenosis Molinary 200113 results not stratified by subgroup Malter 199811 Ohtori 2011 14 Weinstein 2007, 2008, 2010 1. 2. 3. 4. 5. 6. 7. select population, no supervised rehabilitation 15-18 ; Park 2010 19 degenerative spondylolisthesis and stenosis Athiviraham A, Yen D. Is spinal stenosis better treated surgically or nonsurgically? Clin Orthop Relat Res. May 2007;458:90-93. Brox JI, Nygaard OP, Holm I, Keller A, Ingebrigtsen T, Reikeras O. Four-year follow-up of surgical versus non-surgical therapy for chronic low back pain. Ann Rheum Dis. Sep 2010;69(9):1643-1648. Brox JI, Reikeras O, Nygaard O, et al. Lumbar instrumented fusion compared with cognitive intervention and exercises in patients with chronic back pain after previous surgery for disc herniation: a prospective randomized controlled study. Pain. May 2006;122(1-2):145-155. Chang Y, Singer DE, Wu YA, Keller RB, Atlas SJ. The effect of surgical and nonsurgical treatment on longitudinal outcomes of lumbar spinal stenosis over 10 years. J. Am. Geriatr. Soc. May 2005;53(5):785-792. Ghogawala Z, Benzel EC, Amin-Hanjani S, et al. Prospective outcomes evaluation after decompression with or without instrumented fusion for lumbar stenosis and degenerative Grade I spondylolisthesis. J Neurosurg Spine. Oct 2004;1(3):267-272. Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am. Jul 1991;73(6):802-808. Atlas SJ, Deyo RA, Keller RB, et al. The Maine Lumbar Spine Study, Part II. 1-year outcomes of surgical and nonsurgical management of sciatica. Spine (Phila Pa 1976). Aug 1 1996;21(15):1777-1786. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. Atlas SJ, Keller RB, Robson D, Deyo RA, Singer DE. Surgical and nonsurgical management of lumbar spinal stenosis: four-year outcomes from the maine lumbar spine study. Spine (Phila Pa 1976). Mar 1 2000;25(5):556-562. Atlas SJ, Keller RB, Wu YA, Deyo RA, Singer DE. Long-term outcomes of surgical and nonsurgical management of lumbar spinal stenosis: 8 to 10 year results from the maine lumbar spine study. Spine (Phila Pa 1976). Apr 15 2005;30(8):936-943. Malmivaara A, Slatis P, Heliovaara M, et al. Surgical or nonoperative treatment for lumbar spinal stenosis? A randomized controlled trial. Spine (Phila Pa 1976). Jan 1 2007;32(1):1-8. Malter AD, McNeney B, Loeser JD, Deyo RA. 5-year reoperation rates after different types of lumbar spine surgery. Spine (Phila Pa 1976). Apr 1 1998;23(7):814-820. Matsudaira K, Yamazaki T, Seichi A, et al. Spinal stenosis in grade I degenerative lumbar spondylolisthesis: a comparative study of outcomes following laminoplasty and laminectomy with instrumented spinal fusion. J. Orthop. Sci. May 2005;10(3):270-276. Molinari RW, Gerlinger T. Functional outcomes of instrumented posterior lumbar interbody fusion in active-duty US servicemen: a comparison with nonoperative management. Spine J. May-Jun 2001;1(3):215-224. Ohtori S, Koshi T, Yamashita M, et al. Surgical versus nonsurgical treatment of selected patients with discogenic low back pain: a small-sized randomized trial. Spine (Phila Pa 1976). Mar 1 2011;36(5):347-354. Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med. May 31 2007;356(22):2257-2270. Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis. four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am. Jun 2009;91(6):1295-1304. Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med. Feb 21 2008;358(8):794-810. White AH, von Rogov P, Zucherman J, Heiden D. Lumbar laminectomy for herniated disc: a prospective controlled comparison with internal fixation fusion. Spine (Phila Pa 1976). Apr 1987;12(3):305-307. Park DK, An HS, Lurie JD, et al. Does multilevel lumbar stenosis lead to poorer outcomes?: a subanalysis of the Spine Patient Outcomes Research Trial (SPORT) lumbar stenosis study. Spine (Phila Pa 1976). Feb 15 2010;35(4):439-446.