New Chapter
Shelley, for the chapter
Definition/Classification/Prevalence/Risk factors
Etiology
Imaging considerations (goes with Images)
Hydrocephalus
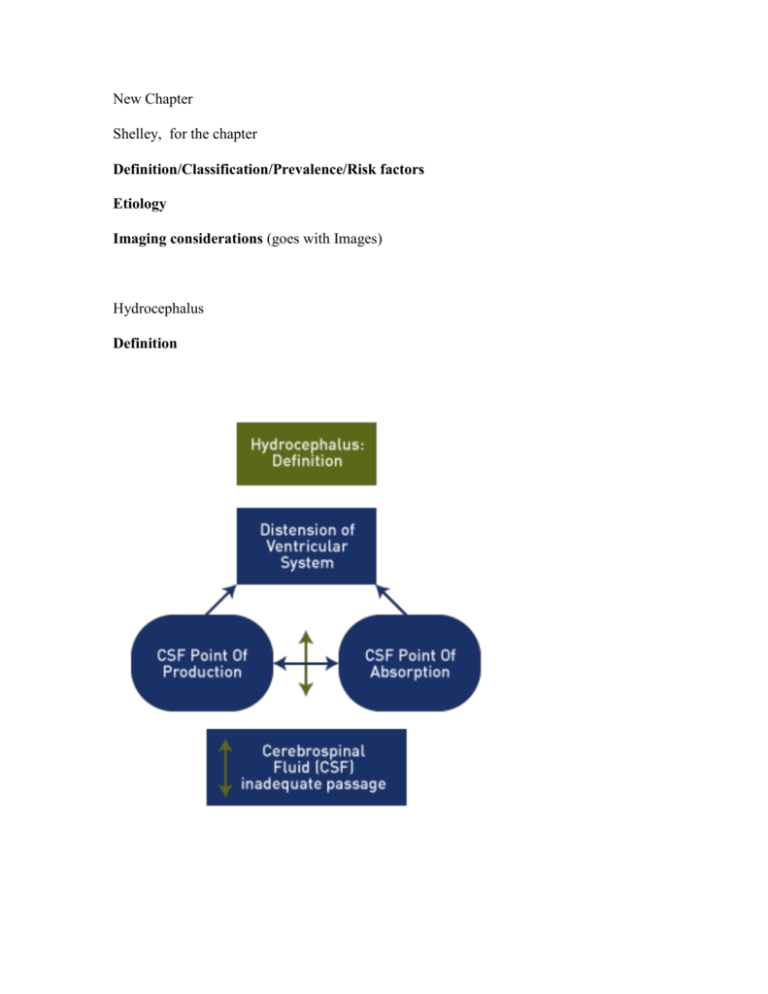
Definition
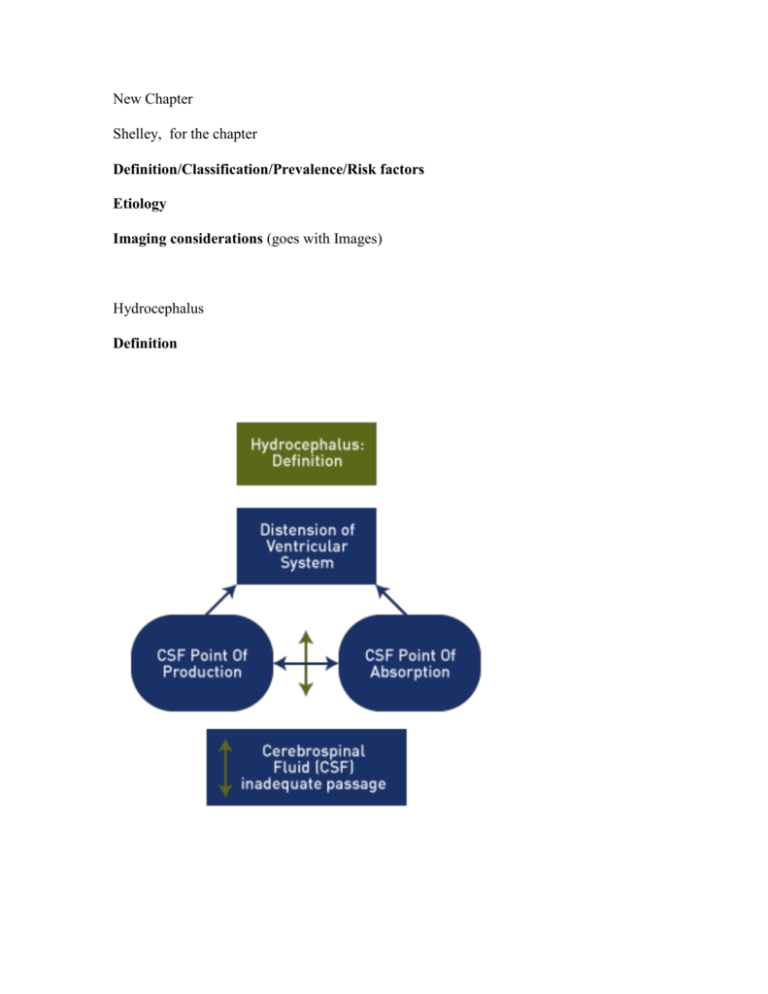
Recent reviews indicate a lack of consensus for the definition of hydrocephalus. [1] One
proposal suggests that hydrocephalus is present when there is active distension of the
ventricular system of the brain related to inadequate passage of CSF from its point of
production within the ventricular system to its point of absorption into the systemic
circulation. [1] This definition differs from that for ventriculomegaly, which suggests
dilation of the lateral ventricles only. Hydrocephalus is present when there is an increase
in the cerebrospinal fluid pressure. These distinctions may not always be apparent on the
initial ultrasound examination.
Classification
Hydrocephalus is usually further defined as communicating and non-communicating.
Communicating hydrocephalus and non-obstructive hydrocephalus are the same and
imply an impairment of CSF resorption, which normally occurs through the venous
system between the ventricles and the subarachnoid space. A number of causes have been
described including infectious, hemorrhagic and congenital.
Non-communicating or obstructive hydrocephalus is due to obstruction of CSF flow to
the subarachnoid space by external compression, narrowing or mass lesion.
Prevalence
The overall prevalence of congenital hydrocephalus in a European series is reported at
4.65 per 10,000 births. [3] The live birth rate was 47% and the termination of pregnancy
rate was 48%. [3] Most live births in the series were detected late in pregnancy.
Risk factors
Reported maternal risk factors for hydrocephalus include: lack of prenatal care,
multiparous gestation, diabetes, chronic hypertension, hypertension during gestation, and
alcohol use during pregnancy. Among patients with congenital hydrocephalus, 12.1%
identified an additional family member who was also diagnosed with hydrocephalus. [3]
Obesity and gestational diabetes may also increase the risk for isolated hydrocephalus.
[4]
Etiology
In a survey central nervous system (CNS) lesions associated with congenital
hydrocephalus diagnosed both prenatally and postnatally, 90.3% were considered
primary and 7.1% were considered secondary. [5] Among those with primary
hydrocephalus, 76.1% were associated with other CNS anomalies which included cystic
lesions, holoprosencephaly, and agenesis of the corpus callosum. [5]
The specific etiologies for hydrocephalus are numerous and diverse. Listed are categories
of factors which are implicated in either the etiology of congenital hydrocephalus or
show a close association.
Aqueductal stenosis is commonly cited as an important cause. Fetal hydrocephalus due to
aqueductal stenosis is classified into two main groups: congenital (X-linked, atresia, septa
and forking) and acquired (post-infectious or post-hemorrhagic, gliosis and tumors,
which also include hamartoma of the posterior fossa. [6] Aqueductal stenosis may be
associated with holoprosencephaly, hypoplasia or agenesis of the corpus callosum,
hippocampal and cerebellar dysplasia and absence of the dorsal median septum. [7]
Chiari type II malformation. [8]
In spinal myelomeningocele and Chiari type II malformation, the spinal lesion is above
the sacrum in over 90% of cases and an association with hydrocephalus is reported in
79% of cases. [9] The hydrocephalus in patients with myelomeningocele is due to
changes in the peri-aqueductal area. [10] These changes include
neuroepithelial/ependymal denudation in or near the aqueduct accounting for the
hydrocephalus. [11]
Irrespective of etiology a number of developmental brain abnormalities have been
described in association with hydrocephalus and include: callosal dysgenesis,
periventricular gray matter heterotopia, hippocampal and white matter hypoplasia,
cortical polygyration, and focal cerebral mantle disruption. [12] Dandy-Walker
malformation and a large posterior fossa cyst can also produce obstructive
hydrocephalus. [13]
Other Syndromes
Syndromes associated with hydrocephalus include: Aicardi syndrome (ventriculomegaly,
neonatal eye finings and infantile spasms and seizures) [14], Fowler syndrome
(vasculopathy and hydrocephaly-hydranencephaly) [15], and (MPPH) syndrome
(megalencephaly, polymicrogyria, and hydrocephalus) [16]. Other syndromes are listed
in the discussion under ventriculomegaly.
Infection
Congenital infections of the brain include most of the TORCH complex (toxoplasmosis,
rubella, cytomegalovirus, herpes, and varicella). [17] Toxoplasmosis is capable of
producing severe hydrocephalus. [18] In certain populations, fetal hydrocephalus is
diagnosed in a high number of women with IgM antibodies to parvovirus B-19 (19.5%)
and in women with positive serology for acute toxoplasmosis (7.3%). [19]
Hemorrhage
After birth, intraventricular hemmorrhage is a common cause of hydrocephalus due to
prematurity. However, intraventricular hemorrhage can occur prior to birth [20] while
hydroceophalus due to cryptic intraventricular hemmorhage may be more common than
previously suggested. [21] Fetal hydrocephalus may also result from pregnancies
complicated by idiopathic thrombocytopenic purpura [22], and fetomaternal alloimmune
thrombocytopenia [23]. Finally, iatrogenic fetal intraventricular hemorrhage due to
warfarin occurs in 4.3% of women on this anticoagulant. [24]
Genetic
Hydrocephalus is a complex neurological disorder and genetic factors may play a role in
development and pathogenesis. To date a number of genes have been identified in
animals but few are identified in humans. [25] The L1 syndrome with X-linked
hydrocephalus is characterized by hydrocephalus, abducted thumbs, spastic paraplegia,
and hypoplasia of the corpus callosum. [25] A number of L1CAM gene mutations have
been identified in affected families and specific mutations and neuroimaging results have
been described. [26] A spectrum of clinical findings is possible in families with X-linked
hydrocephalus [27], while new mutations continue to be described. [28]
Fanconi anemia complementation group B mutation may present as an X linked
VACTERL with hydrocephalus syndrome. [29] Ring chromosome 6 is associated with a
spectrum of clinical disorders which include hydrocephalus. [30]
Imaging Considerations Shelley, put this at the beginning of Images.
Fetal ventricular dilatation is a common or associated finding in intracranial and some
systemic conditions. As noted, the major intracerebral associations include: aqueductal
stenosis, Chiari II malformation, Dandy-Walker syndromes and agenesis of the corpus
callosum. [32]
In order to properly assess fetal hydroceiphalus and its related causes and associations,
visualization of the posterior fossa and the corpus callosum is necessary. [33,34]
The transverse axial view permits visualization, and measurement of the lateral ventricles
as well as critical head measurements. It affords a view of the contents within the
ventricle (blood, tumor) as well as an assessment of intracranial calcifications. The midsagittal view of the fetal brain best accomplishes visualization of the corpus callosum,
cavum septum pellucidum and posterior fossa.
In breech presentation and transverse lie of the fetus, the mid-sagittal view can be
obtained with a transabdominal scanning plane; with cephalic presentation, a transvaginal approach gives the best opportunity for mid-sagittal visualization. [35] The
visualization of the septum pellucidum in all instances is helpful. Coronal views are also
useful for defining the site of ventricular communication and confirming the absence of
the corpus callosum.
In cases of mild to severe ventriculomegaly and communication between the ventricles,
certain observations are helpful for diagnosis for diagnoisis of specific conditions. When
there is ventriulomegaly and non-cleavage of the cerebral hemispheres along with facial
anomalies, holoprosencephaly is the most likely diagnosis. [36] When the communication
of the lateral ventricles is through the third ventricle with normal appearing anterior and
posterior segments, hydrocephalus is the most likely diagnosis, either from enlargement
of the foramen of Monroe or disruption of the septum pellucidum. [36]
A more complete listing of the distinguishing features between holoprosencephaly and
hydrocephalus is presented. [36]
Variability is common in ultrasound and MRI interpretation of fetal CNS images. [37]
Prospective agreement was achieved in 60% of ultrasound diagnosis and 53% of MRI
diagnosis among obstetric sonologist and pediatric neuroradiologists. [37]
In a comparison between prenatal ultrasound and autopsy findings, observations were
identical in 68.1% of 339 pregnancies. Partial agreement was noted but additional
findings were recorded by autopsy in 24.2% of cases while different findings were
recorded between ultrasound and autopsy in 7.7% of cases.[38]
In another study comparing prenatal ultrasound with autopsy findings the overall rate of
agreement among CNS malformations was 62% and was highest in cranial/anencephaly
92% and lowest and hydrocephaly (39%). [39]
Major errors in antenatal ultrasound of intracranial structures include those related to
brain parenchyma, ventricular system and the choroid plexus. [40]
Typical ultrasound findings in fetal intracranial hemorrhage include: irregular echogenic
brain mass, intraventricular echogenic foci, periventricular echodensities;
ventriculomegaly; and post-hemorrhagic hydrocephalus. [41]
Ultrasound findings in fetal viral infections are nonspecific and systemic, while some
findings are specific to intracranial anatomic changes. [42] A systemic fetal viral
infection may be manifest by: growth restriction, ascites, hydrops, ventriculomegaly,
intracranial calcifications, hydrocephaly, microcephaly, cardiac anomalies,
hepatosplenomegaly, and echogenic bowel, placentomegaly, and abnormal amniotic fluid
volume. [42]
In the presence of ventriculomegaly, intracranial and hepatic calcifications,
cytomegalovirus ((CMV) should be suspected. [42] Cardiac anomalies may be present in
congenital rubella syndrome, while limb contractures and cerebral anomalies may
suggest infection with varicella zoster virus. [42]
Cerebral fetal ventricular structures can be visualized with 3-D sonography between 7
and 12 completed weeks. [43] Multiplanar 3-D images are an effective way to assess
critical CNS structures. The corpus callosum, fourth ventricle, cerebellar vermis as well
as other critical structures were identified by this method. [44]
References
1. A contemporary definition and classification of hydrocephalus.
[Literature Review].
Semin Pediatr Neurol.2009 Mar; 16 (1): 9-15.
Rekate HL.
Department of Pediatric Neurosurgery, Barrow Neurological Institute, Phoenix, AZ
85013, USA.(Email: harold.rekate@bnaneuro.net).
This review focuses on the problems related to defining hydrocephalus and on the
development of a consensus on the classification of this common problem.Such a
consensus is needed so that diverse research efforts and plans of treatment can be
understood in the same context.The literature was searched to determine the definition of
hydrocephalus and to identify previously proposed classification schemes.The historic
perspective, purpose, and result of these classifications are reviewed and analyzed.The
concept of the hydrodynamics of cerebrospinal fluid (CSF) as a hydraulic circuit is
presented to serve as a template for a contemporary classification scheme.Finally, a
definition and classification that include all clinical causes and forms of hydrocephalus
are suggested.The currently accepted classification of hydrocephalus into
"communicating" and "noncommunicating" varieties is almost 90 years old and has not
been modified despite major advances in neuroimaging, neurosciences, and treatment
outcomes.Despite a thorough search of the literature using computerized search engines
and bibliographies from review articles and book chapters, I identified only 6 previous
attempts to define and classify different forms of hydrocephalus.This review proposes the
following definition for hydrocephalus: hydrocephalus is an active distension of the
ventricular system of the brain related to inadequate passage of CSF from its point of
production within the ventricular system to its point of absorption into the systemic
circulation.Based on this definition (potential points of flow restriction) and on the view
of the CSF system as a hydraulic circuit, a classification system is proposed.The
acceptance of this proposed definition and classification schema would allow clinicians
and basic scientists to communicate effectively, to share information and results, and to
develop testable hypotheses.
PMID: 19410151
2. Congenital hydrocephalus:Prevalence, prenatal diagnosis, and outcome of pregnancy
in four European regions.
Eur J Paediatr Neurol.2010 Mar; 14 (2): 150-5.Epub 2009 May 2.
Garne E, Loane M, Addor MC, Boyd PA, Barisic I, Dolk H.
Paediatric Department, Kolding Hospital, DK-6000 Kolding,
Denmark.(Email:egarne@health.sdu.dk).
Objective:To describe prevalence, prenatal diagnosis and outcome for fetuses and infants
with congenital hydrocephalus.Methods:Data were taken from four European registries of
congenital malformations (EUROCAT).The registries included are based on multiple
sources of information and include information about livebirths, fetal deaths with GA >
or = 20 weeks and terminations of pregnancy for fetal anomaly (TOPFA).All cases from
the four registries diagnosed with congenital hydrocephalus and born in the period 19962003 were included in the study.Cases with hydrocephalus associated with neural tube
defects were not included in the study.Results:Eighty-seven cases with congenital
hydrocephalus were identified during the study period giving an overall prevalence of
4.65 per 10,000 births.There were 41 livebirths (47%), four fetal deaths (5%) and 42
TOPFA (48%).Nine percent of all cases were from a multiple pregnancy.Additional noncerebral major malformations were diagnosed in 38 cases (44%) and karyotype
anomalies in eight cases (9%).Median GA at TOPFA was 21 weeks.Among livebirths
61% were diagnosed prenatally at a median GA of 31 weeks (range 17-40 weeks) and
median GA at birth was 37 weeks.Fourteen liveborn infants (34%) died within the first
year of life with the majority of deaths during the first week after
birth.Conclusion:Congenital hydrocephalus is a severe congenital malformation often
associated with other congenital anomalies.CH is often diagnosed prenatally, although
sometimes late in pregnancy.A high proportion of affected pregnancies result in
termination for severe fetal anomaly and there is a high mortality in livebirths.2009
European Paediatric Neurology Society.Published by Elsevier Ltd.All rights reserved.
PMID: 19410489
3.Risk factors of congenital hydrocephalus:A 10 year retrospective study.
J Neurol Neurosurg Psychiatry.2009 Feb; 80 (2): 213-7.Epub 2008 Jul 24.
Van Landingham M, Nguyen TV, Roberts A, Parent AD, Zhang J.
Department of Neurosurgery, University of Mississippi Medical Center, Jackson, MS
39216-4505, USA.
Objective:To evaluate and identify the risk factors associated with the pathogenesis of
congenital hydrocephalus in a large specific population.Methods:An International
Classification of Diseases (ICD)-9 database search of patients with congenital
hydrocephalus treated at the University of Mississippi Medical Center between 1998 and
2007 was performed.All recruited patients were interviewed, assessing maternal age,
onset of prenatal care, geographic location of pregnancy, maternal diabetes and chronic
hypertension, pregnancy induced hypertension, pre-eclampsia, eclampsia, single or
multiparous gestation, maternal alcohol, tobacco and drug use, infection and trauma
during gestation, trauma or sexually transmitted disease at parturition, and other family
members with hydrocephalus.Results:In this 10 year retrospective study, several
significant risk factors were identified among 596 well defined cases of congenital
hydrocephalus.The identified risk factors included lack of prenatal care, multiparous
gestation, maternal diabetes, maternal chronic hypertension, maternal hypertension
during gestation and alcohol use during pregnancy.Of these patients with congenital
hydrocephalus, 12.1% identified an additional family member also diagnosed with
hydrocephalus.No differences in risk factors were identified between sporadic and
familial congenital hydrocephalus cases except for an increased incidence of multiparous
pregnancies and prenatal care in the first trimester in familial cases.Conclusions:A
number of key risk factors have been identified to be strongly associated with the
development of congenital hydrocephalus in an infant.The prevalence of familial patterns
of inheritance for congenital hydrocephalus suggests a broader role for genetic factors in
the pathogenesis of congenital hydrocephalus.
PMID: 18653551
4. Maternal obesity, gestational diabetes, and central nervous system birth defects.
Epidemiology.2005 Jan; 16 (1): 87-92.
Anderson JL, Waller DK, Canfield MA, Shaw GM, Watkins ML, Werler MM.
The University of Texas, Houston Health Science Center, School of Public Health,
Houston, Texas, USA.(Email: andersjl@etsu.edu).
Background:Maternal obesity and diabetes are both associated with increased risk of
congenital central nervous system (CNS) malformations in the offspring and may share a
common underlying mechanism.Our objective was to evaluate whether gestational
diabetes influenced the association of prepregnancy maternal obesity and risks for CNS
birth defects.Methods:This Texas population-based case-control study evaluated births
occurring January 1997 through June 2001.Data came from structured telephone
interviews.Cases (n=477) were mothers of offspring with anencephaly (n=120), spina
bifida (n=184), holoprosencephaly (n=49), or isolated hydrocephaly (n=124).Controls
(n=497) were mothers of live infants without abnormalities randomly selected from the
same hospitals as cases.Response rates were approximately 60% for both cases and
controls.We evaluated maternal obesity (body mass index > or =30.0 kg/m) and risks for
CNS birth defects, as well as whether gestational diabetes influenced the
risks.Results:After adjusting for maternal ethnicity, age, education, smoking, alcohol use,
and periconceptional vitamin use, obese women had substantially increased risks of
delivering offspring with anencephaly (odds ratio=2.3; 95% confidence interval=1.2-4.3),
spina bifida (2.8; 1.7-4.5), or isolated hydrocephaly (2.7; 1.5-5.0), but not
holoprosencephaly (1.4; 0.5-3.8).Odds ratios were higher for the joint effects of maternal
obesity and gestational diabetes, with evidence for interaction on a multiplicative
scale.Conclusions:Maternal obesity and gestational diabetes may increase the risk of
CNS birth defects through shared causal mechanisms.
PMID: 15613950
5. Nationwide survey of the etiology and associated conditions of prenatally and
postnatally diagnosed congenital hydrocephalus in Japan.
Neurol Med Chir (Tokyo). 2007 Oct; 47 (10): 448-52; discussion 452.
Moritake K, Nagai H, Miyazaki T, Nagasako N, Yamasaki M, Tamakoshi A.
Department of Neurosurgery, Shimane University School of Medicine, Izumo, Shimane,
Japan.
A nationwide survey in 2000 investigated the causative and associated central nervous
system (CNS) lesions of congenital hydrocephalus in Japan. The etiology and associated
diseases in 393 patients with congenital hydrocephalus were analyzed and compared
between 193 patients with prenatally diagnosed (fetal) hydrocephalus and 181 with
postnatally diagnosed (infantile) hydrocephalus. Of 393 patients of congenital
hydrocephalus, 355 (90.3%) had primary hydrocephalus and 28 (7.1%) had secondary
hydrocephalus. Of 355 patients with primary hydrocephalus, 85 (23.9%) had simple
hydrocephalus associated with no other CNS anomaly and 270 (76.1%) had complicated
hydrocephalus associated with other CNS anomalies. Destructive cystic lesions,
holoprosencephaly, and agenesis of the corpus callosum were significantly predominant
in fetal hydrocephalus. Arachnoid cyst was somewhat predominant in infantile
hydrocephalus. The majority of cases of congenital hydrocephalus were primary
hydrocephalus and two thirds were complicated hydrocephalus. Several complications
showed marked predominance in fetal hydrocephalus.
PMID: 17965561
6. Fetal aqueductal glioneuronal hamartoma: A clinicopathological and
physiopathological study of three cases.
Clin Neuropathol. 2005 Jul-Aug; 24 (4): 155-62.
Marcorelles P, Fallet-Bianco C, Oury JF, van Wallenghem E, Parent P, Labadie G,
Lagarde N, Laquerrière A.
Pathology Laboratory, University Hospital, Brest, France. (Email:
pascale.marcorelles@chu-brest.fr).
Fetal hydrocephalus due to
Fetal aqueductal glioneuronal hamartoma: A clinicopathological and physiopathological
study of three cases.
Clin Neuropathol. 2005 Jul-Aug; 24 (4): 155-62.
Marcorelles P, Fallet-Bianco C, Oury JF, van Wallenghem E, Parent P, Labadie G,
Lagarde N, Laquerrière A.
Pathology Laboratory, University Hospital, Brest, France. (Email:
pascale.marcorelles@chu-brest.fr).
Fetal hydrocephalus due to aqueductal stenosis is classified into two main groups:
congenital (X-linked, atresia, septa and forking) and acquired (post-infectious or posthemorrhagic, gliosis and tumors). Material and Methods: We report three fetal cases
presenting with severe hydrocephalus, two of which being apparently sporadic, and the
third possibly inherited. On macroscopic examination, no associated malformations were
identified, either craniofacial dysmorphy, or visceral abnormalities. Neuropathological
study revealed massive hydrocephalus caused by narrowing of the Aqueduct of Sylvius.
Histological examination evidenced a nodular, well-demarcated mass producing into the
aqueductal lumen, and containing numerous immature proliferating glioneuronal cells.
Immunohistochemical analyses did not suggest a developmental abnormality of the
subcommissural organ but rather a hamartomatous malformative process. Results:
Hamartoma of the posterior fossa has been rarely reported. Post-natal cases have been
described in the cerebello-pontine angle or in the quadrigeminal plate, and have always
been diagnosed as pilocytic or low-grade astrocytomas. In our cases, the lesions could be
related to so-called pencil glioma, sometimes associated with type 1 neurofibromatosis
and, to our knowledge, have never been described prior to birth. The occurrence during
fetal life and the progressive maturation of the nodules are more likely in favor of a
hamartomatous process. Conclusion: Even though they could sporadically occur, an
accurate genetic counseling should be required in order to ensure that there is no familial
history of Recklinghausen disease, and to provide a more precise evaluation of recurrence
risk.
PMID: 16033131
7. Congenital aqueductal stenosis due to downregulation of a dorsalizing gene.
The FASEB Journal. 2008; 22: 59.4.
Sarnat HB, Flores-Sarnat L.
Department of Pathology (Neuropathology), University of Calgary Faculty of Medicine;
Department of Paediatrics, Alberta Children’s Hospital, Calgary, Canada.
Congenital aqueductal stenosis is a frequent cause of fetal hydrocephalus. We studied 9
human fetuses at midgestation with aqueductal stenosis for clues to etiology. Two had
holoprosencephaly. Associated dysgeneses in all 9 included hypoplasia or agenesis of the
corpus callosum; hippocampal and cerebellar dysplasias; absence of the dorsal median
septum, confirmed by vimentin. The sagittal intercollicular fissure was absent or shallow
with collicular continuity across the midline. In 2 cases, only the rostral mesencephalon
was involved. These findings suggest downregulation of a gene acting in the dorsoventral
gradient of the vertical axis of the neural tube, and also in rostrocaudal and mediolateral
gradients.
PMID: N/A
Link: http://www.fasebj.org/cgi/content/meeting_abstract/22/1_MeetingAbstracts/59.4
8. Fetal hydrocephalus: Prenatal treatment.
Childs Nerv Syst. 2003 Aug; 19 (7-8): 561-73. Epub 2003 Aug 8.
Cavalheiro S, Moron AF, Zymberg ST, Dastoli P.
Section of Pediatric Neurosurgery, Federal University of São Paulo, Rua Botucatu
591/42, 04023-062 São Paulo, Brazil. (Email: iscava@uol.com.br).
Patients and Methods: From January 1986 to January 2001, 85 cases of hydrocephalus
were referred to the Pediatric Neurosurgery and Fetal Medicine Sections of the São Paulo
Federal University and the Santa Joana Maternity Hospital in São Paulo, Brazil. Thirtynine of these cases concerned fetuses ranging from 24 to 32 weeks' gestation, who
underwent intrauterine treatment. The hydrocephalus etiologies consisted of: aqueduct
stenosis (18 cases), intraventricular hemorrhage (8 cases), Dandy-Walker malformation
(4 cases), Chiari type II (4 cases), and other diverse etiologies (5 cases). Twenty fetuses
underwent repeated cephalocentesis: 18 received a ventriculo-amniotic shunt and in 1
case endoscopic third ventriculostomy was performed. The follow-up period varied
between 1 and 14 years (median 5 years). Out of 39 patients, 26 have been considered as
normal (IQ above 70), 6 have mild or moderate handicaps (IQ from 35 to 70), and 7 are
severely handicapped (IQ below 35). After birth, 38 patients underwent
ventriculoperitoneal shunting with low-pressure valves. Conclusion: In the absence of
chromosomopathies, when the gestational age ranges between 24 and 32 weeks,
progressive fetal hydrocephalus of a non-infectious origin can obtain benefit from
intraventricular decompression performed during the fetal period. New methods of
diagnosis and treatment should be developed, especially in those countries where
interruption of gestation is not permitted by law, for the benefit of those families who,
due to social or religious factors, do not accept abortion.
PMID: 12908113
9. Assessment of neurosurgical outcome in children prenatally diagnosed with
myelomeningocele and development of a protocol for fetal surgery to prevent
hydrocephalus.
Childs Nerv Syst. 2007 Apr; 23 (4): 421-5. Epub 2007 Jan 17.
Zambelli H,Carelli E , Honorato D, Marba S, Coelho G, Carnevalle A, Iscaife A, da Silva
E, Barini R, Sbragia L.
Discipline of Neurosurgery-Fetal Medicine Group, Universidade Estadual de CampinasUNICAMP, Rua Alexander Fleming, 181, Barão Geraldo, Campinas-SP, Brazil. (Email:
hzambelli@uol.com.br).
Introduction: Prenatal diagnosis of myelomeningocele (MMC) has permitted a better
planning for optimum management of the disease. More recently, it has allowed for a
possible intrauterine repair of the spinal defect. Objective: To describe neurosurgical
outcome in children with myelomeningocele and follow-up at a referral center in Fetal
Medicine. Patients were characterized for the development of a protocol suitable for fetal
surgery, and fetuses who were possible candidates for intrauterine surgery were
identified. Materials and Methods: A retrospective descriptive analysis was performed of
98 cases of fetal myelomeningocele, seen at CAISM-UNICAMP, from January 1994 to
December 2002, identifying cases with a possible indication for fetal surgery. Results:
Mean gestational age at diagnosis was 29 weeks (17-39); level of lesion was above the
sacral region in 92.84%; association with hydrocephalus occurred in 78.57%. During
clinical course, 82.5% of patients had neurogenic bladder and 60% had neural and mental
deficits. Potential intrauterine repair rate was 11.57%, using criteria from the protocol
developed in our service. Conclusion: Myelomeningocele is associated with severe and
frequent sequelae. In virtually 12% of our cases, fetal surgery could have been offered as
a therapeutic option.
PMID: 17226038
10.Pathogenesis of cerebral malformations in perinatal spina bifida aperta.
Cerebrospinal Fluid Research. 2007: 4 (Suppl 1): S9.
de Wit OA, den Dunnen WF, Sollie KM, Brouwer OF, Sival DA.
Department of Pediatric Neurology, Department of Pathology and Laboratory Medicine,
Department of Obstetrics, and Department of Pediatrics, University of Groningen,
University Medical Centre Groningen, the Netherlands.
Background: Spina bifida aperta (SBA) is associated with cerebral morbidity, such as
hydrocephalus, Chiari II malformation, and cortical dysplasia. Insight in the pathogenesis
of these malformations is incomplete. In fetal SBA, such information may help to
improve pre- and early postnatal treatment strategies. In perinatal SBA, we investigated
the time of initiation of concurrent cerebral malformations. Materials and Methods: In 7
SBA fetuses and 1 neonate [16–40 (median 28) weeks gestational age (g.a.)], we crosssectionally investigated the histology of the aqueduct [n = 5], cerebral convexity and
parenchyma [n = 8] by haematoxylin-eosin and nestin staining. The meningomyelocele
was located at cervical [n = 1], thoracic [n = 3] and lumbar [n = 4] spinal level. Cerebral
histology was intra-individually associated with fetal ultrasound parameters (ventricular
size, head circumference and Chiari II malformation). The mean and median duration
between fetal ultrasound and histological assessment were both 4 days. Results: In SBA
fetuses of all gestational ages, histological malformations at the aqueduct
(hemosiderophages/gliosis [5/5] and forking/slit like deformities [5/5]) were present. In
the two youngest fetuses (16 and 21 weeks g.a.), we observed peri-aqueductal ependymal
denudation, progenitor cell loss and heterotopia. From the 2nd half of pregnancy
onwards, Chiari II malformation concurred with ventriculomegaly [4/6] and successively,
with macrocephaly from 37 weeks g.a. onwards [3/3]. In absence of arachnoidal fibrosis,
delivery-related haemorrhages were present in all fetuses (at the fossa posterior and/or
cerebrum in 6/7 and 5/7 fetuses, respectively). In the only patient that succumbed during
the first week after birth (39 weeks g.a.), raised intracranial pressure concurred with
arachnoidal fibrosis at the convexity. Conclusion: In fetal SBA, the earliest periaqueductal alterations precede the development of hydrocephalus. During the 2nd half of
pregnancy, ventriculomegaly appeared unrelated to CSF malabsorption. After birth,
however, CSF malabsorption may increasingly contribute to the development of highpressure hydrocephalus. These data may implicate that peri-aqueductal ependymal
denudation and progenitor cell loss occur by a mechanism independent of high-pressure
hydrocephalus or ventricular distention.
PMID: N/A
Link: http://cerebrospinalfluidresearch.com/content/4/S1/S9
11. Pathogenesis of cerebral malformations in human fetuses with meningomyelocele.
Cerebrospinal Fluid Res. 2008 Mar 1; 5: 4.
de Wit OA, den Dunnen WF, Sollie KM, Muñoz RI, Meiners LC, Brouwer OF,
Rodríguez EM, Sival DA.
Department of Pediatrics, University Medical Center, University of Groningen,
Hanzeplein 1, 9700 RB, Groningen, The Netherlands. (Email: d.a.sival@bkk.umcg.nl).
Background: Fetal spina bifida aperta (SBA) is characterized by a spinal
meningomyelocele (MMC) and associated with cerebral pathology, such as
hydrocephalus and Chiari II malformation. In various animal models, it has been
suggested that a loss of ventricular lining (neuroepithelial/ependymal denudation) may
trigger cerebral pathology. In fetuses with MMC, little is known about
neuroepithelial/ependymal denudation and the initiating pathological events. The
objective of this study was to investigate whether neuroepithelial/ependymal denudation
occurs in human fetuses and neonates with MMC, and if so, whether it is associated with
the onset of hydrocephalus. Methods: Seven fetuses and 1 neonate (16-40 week
gestational age, GA) with MMC and 6 fetuses with normal cerebral development (22-41
week GA) were included in the study. Identification of fetal MMC and clinical
surveillance of fetal head circumference and ventricular width was performed by
ultrasound (US). After birth, MMC was confirmed by histology. We characterized
hydrocephalus by increased head circumference in association with ventriculomegaly.
The median time interval between fetal cerebral ultrasound and fixing tissue for histology
was four days. Results: At 16 weeks GA, we observed neuroepithelial/ependymal
denudation in the aqueduct and telencephalon together with sub-cortical heterotopias in
absence of hydrocephalus and/or Chiari II malformation. At 21-34 weeks GA, we
observed concurrence of aqueductal neuroepithelial/ependymal denudation and
progenitor cell loss with the Chiari II malformation, whereas hydrocephalus was absent.
At 37-40 weeks GA, neuroepithelial/ependymal denudation coincided with Chiari II
malformation and hydrocephalus. Sub-arachnoidal fibrosis at the convexity was absent in
all fetuses but present in the neonate. Conclusion: In fetal SBA,
neuroepithelial/ependymal denudation in the telencephalon and the aqueduct can occur
before Chiari II malformation and/or hydrocephalus. Since denuded areas cannot reestablish cell function, neuro-developmental consequences could induce permanent
cerebral pathology.
PMID: 18312688
12. Focal cerebral mantle disruption in fetal hydrocephalus.
Pediatr Neurol. 2007 Apr; 36 (4): 236-43.
Humphreys P, Muzumdar DP, Sly LE, Michaud J.
Department of Pediatrics (Neurology Division), Children's Hospital of Eastern Ontario,
and University of Ottawa, Ottawa, Ontario, Canada. (Email: phumphreys@cheo.on.ca).
A variety of developmental brain anomalies have been described in individuals with fetal
hydrocephalus, regardless of etiology. Examples include callosal dysgenesis,
periventricular gray matter heterotopia, hippocampal and white matter hypoplasia, and
cortical polygyration. The present report draws attention to another anomaly not reported
in previous case series of fetal hydrocephalus: focal cerebral mantle disruption. Neonatal
imaging findings (where available) and post-shunt, stable-state magnetic resonance
imaging, or pathological findings were reviewed in 77 subjects with fetal hydrocephalus
(55 myelomeningocele, 16 sporadic aqueductal stenosis, 6 miscellaneous). Of these, 12
subjects (15.6%) demonstrated a combination of absence of the septum pellucidum and
severe thinning or absence of the posteromesial cerebral mantle. On axial sequences, this
combination created the illusion of a common ventricle, as in lobar holoprosencephaly.
All 12 subjects had massive hydrocephalus at birth, accompanied in 7 by posteromesial
ventricular diverticula. Two subjects, and one other subject with distinct lateral
ventricles, demonstrated unilateral or bilateral mantle clefts suggestive of schizencephaly.
Close radiological (n = 2) or pathological (n = 1) inspection showed that the clefts were
only partially lined with gray matter and contained a transverse gliotic membrane. These
findings are consistent with the hypothesis that massive early fetal hydrocephalus may
completely disrupt cerebral mantle formation, particularly in the posteromesial
hemispheres.
PMID: 17437906
13.Fetal MRI of a severe Dandy-Walker malformation with an enlarged posterior fossa
cyst causing severe hydrocephalus.
Fetal Diagn Ther. 2005 Nov-Dec; 20 (6): 524-7.
Teksam M, Ozyer U, McKinney A, Kirbas I, Cakir B.
Baskent University Medical School, Department of Radiology, Ankara, Turkey. (Email:
mehmett@baskent-ank.edu.tr).
We present a case of severe Dandy-Walker malformation with enlarged posterior fossa
cyst extruding through the incisura of the tentorium and causing severe hydrocephalus. A
posterior fossa malformation was suspected by ultrasonography and was further
evaluated by fetal magnetic resonance imaging (MRI). Fetal MRI demonstrated that there
were no associated anomalies and the decision was made to continue with labor instead
of terminating the pregnancy. The precise diagnosis and absence of associated anomalies
revealed by MRI aided in parent counseling and obstetrical management. Copyright (c)
2005 S. Karger AG, Basel.
PMID: 16260889
14. Aicardi syndrome mimicking intrauterine hydrocephalus.
Brain Dev. 2009 Sep; 31 (8): 638-40. Epub 2008 Nov 11.
Muthugovindan D, Kossoff EH, Sakonju A, Johnston MV.
Department of Neurology, Johns Hopkins Medical Institutions, Baltimore, MD 21287,
USA. (Email: dmuthug2@jhmi.edu).
Congenital enlargement of the cerebral ventricles is now commonly recognized in utero
due to the availability of high resolution prenatal ultrasonography. It is important to
distinguish between congenital hydrocephalus and ventricular enlargement due to
malformations, infections or other destructive processes because these disorders can have
markedly different prognoses. We report an infant diagnosed with Aicardi syndrome in
the newborn period based on brain MRI and ophthalmological findings after she was
referred for evaluation of hydrocephalus seen on fetal ultrasound. Aicardi syndrome most
commonly comes to medical attention because of seizures later in infancy.
PMID: 19004586
15.Fowler syndrome presenting as a Dandy-Walker malformation: A second case report.
Pediatr Dev Pathol. 2009 Jan-Feb; 12 (1): 68-72.
Al-Adnani M, Kiho L, Scheimberg I.
Department of Histopathology, The Royal London Hospital, England, United Kingdom.
(Email: madnani8@hotmail.com).
Fowler syndrome, also known as proliferative vasculopathy and hydrocephalyhydranencephaly, is a lethal condition characterized by hydrocephalus associated with
progressive destruction of central nervous system tissue as a result of an unusual and
characteristic proliferative vasculopathy. The occurrence of Fowler syndrome in
consanguineous families and recurrence in both sexes are suggestive of an autosomal
recessive transmission. We present the second case of Fowler syndrome presenting as a
Dandy-Walker malformation, in a consanguineous family.
PMID: 18702566
16.Megalencephaly, polymicrogyria, and hydrocephalus (MPPH) syndrome: A new case
with syndactyly.
J Child Neurol. 2008 Aug; 23 (8): 916-8. Epub 2008 May 12.
Pisano T, Meloni M, Cianchetti C, Falchi M, Nucaro A, Pruna D.
Division of Child Neurology and Psychiatry, Azienda Ospedaliero-Universitaria di
Cagliari, Cagliari, Italy.
Megalencephaly, polymicrogyria, and hydrocephalus (MPPH) syndrome is characterized
by megalencephaly, perisylvian polymicrogyria, postaxial polydactyly, and
hydrocephalus. Seven cases have been reported. This report presents a new sporadic
patient with megalencephaly, polymicrogyria, and hydrocephalus syndrome, a girl born
to healthy, nonconsanguineous parents at 38 weeks. Macrocephaly (+4 standard
deviation) was present at birth. She had syndactyly instead of the postaxial polydactyly
reported in the other patients. Neurologic examination showed severe diffuse hypotonia
and profound developmental delay. Magnetic resonance imaging revealed enlarged
lateral and third ventricles, with cavum septi pellucidi et vergae, bilateral abnormal white
matter intensity, and diffuse polymicrogyria, most prominent in both the frontal and
perisylvian regions. A visual evoked potential study showed increased latencies, probably
caused by white matter abnormalities. At 16 months, she has never had seizures and
shows profound psychomotor retardation. Results of metabolic and genetic studies were
normal.
PMID: 18474936
17.Screening for infectious diseases.
Childs Nerv Syst. 2003 Aug; 19 (7-8): 429-32. Epub 2003 Jun 14.
Gerber S, Hohlfeld P.
Department Gynecology and Obstetrics, CHUV, 1011 Lausanne, Switzerland. (Email:
Stefan.Gerber@chuv.hospvd.ch).
Introduction: Fetal brain injury is an essential cause of lifelong morbidity. Infection
appears as a cause of brain damage. Apart from chorioamnionitis, screening for infectious
diseases must be considered in pregnancies with a risk of congenital infection or cases
with abnormal cerebral ultrasound findings. Discussion: Congenital infections include
most of the major components of the TORCH complex: toxoplasmosis, rubella,
cytomegalovirus, herpes, and varicella. Seronegative mothers can develop primary
infection, which carries a risk of vertical transmission. The timing of the infection is a
critical point, because fetal damage often depends on the gestational age at which acute
maternal infection took place and occurs more likely in the first half of pregnancy.
Antenatal ultrasound can detect brain abnormalities, like hydrocephalus, periventricular
leukomalacia, calcifications or hemorrhage. Maternal serologic tests must be performed
to look for an infectious etiology; the most frequent agents are the components of the
TORCH complex. But additional serology must include parvovirus B19, HIV, and
coxsackieviruses.
PMID: 12811485
18.Too late prenatal diagnosis of fetal toxoplasmosis: A case report.
Fetal Diagn Ther. 2005 May-Jun; 20 (3): 190-3.
Nowakowska D, Respondek-Liberska M, Golab E, Stray-Pedersen B, Szaflik K,
Dzbenski TH, Wilczynski J.
Department of Fetal Maternal Medicine, Research Institute Polish Mother's Memorial
Hospital, Lodz, Poland. (Email: dnowakowska@hotmail.com).
Objective: We describe a case of severe fetal hydrocephalus due to toxoplasmosis which
could not be diagnosed until late gestational age due to the lack of a serologic
surveillance program during pregnancy; moreover, this case points to the usefulness of
molecular biology tools in the diagnostic process. Abnormal ultrasound in the 2nd
trimester was noticed and Toxoplasma gondii was demonstrated in amniotic fluid at the
28th week of gestation both by PCR and by mice inoculation. Fansidar and folinic acid
were administered. The newborn suffered from progressive hydrocephalus, seizures, and
pathological muscular tonus; ultrasound examination showed massive cerebral
calcifications. Ophthalmologic examination revealed bilateral choroidoretinitis.
Congenital toxoplasmosis was confirmed by the detection of anti- T. gondii IgM and IgA
in the neonatal serum. Conclusion: The presented case is an example of severe fetal
toxoplasmosis diagnosed and treated in utero. Copyright (c) 2005 S. Karger AG, Basel.
PMID: 15824496
19.Analysis of complications during pregnancy in women with serological features of
acute toxoplasmosis or acute parvovirosis.
Ginekol Pol. 2008 Mar; 79 (3): 186-91.
Marcinek P, Nowakowska D, Szaflik K, Spiewak E, Małafiej E, Wilczyński J.
Klinika Medycyny Matczyno-Płodowej i Ginekologii, Instytutu Centrum Zdrowia Matki
Polki i III Katedry Połoznictwa i Ginekologii, Uniwersytetu Medycznego w Lodzi.
Objectives: Toxoplasma gondii and parvovirus B19 (PVB19) infections in a healthy adult
are usually asymptomatic. Congenital toxoplasmosis is the cause of hydrocephalus,
chorioretinitis and intracranial calcifications. Hydrops remains the most common
complication during the fetal PVB infection. The aim of the study was to analyze the
complications during pregnancy in women with serological features of acute
toxoplasmosis or acute parvovirosis. Material and Methods: In our study, we have
included 1800 pregnant women, hospitalized in Department of Fetal-Maternal Medicine
and Gynecology Research Institute, Polish Mother's Memorial Hospital (RIPMMH) in
Lodz, (Poland) between 2000-2007. Anti-T.gondii antibodies were tested by ELISA
Vidas Toxo IgG, ELISA Vidas IgM (BioMerieux) and Platelia Toxo-A Anti-PVB19
antibodies were detected by NovaLisa Parvovirus B19 Recombinant IgG-ELISA and
IgM-ELISA (NOVATEC). Results: Prevalence of IgG anti-PVB19 among pregnant
women was 35% (n=633). IgG anti-T.gondii was noticed in 55.5% (n=910) of women.
Serological features of acute parvovirosis were demonstrated in 13.5% (n=243) of the
patients and 74.2% (n=256) of women suffered from acute toxoplasmosis. Fetal
hydrocephalus or ventriculomegaly was diagnosed in 19.5% (n=64) of the pregnancies
with IgM anti-PVB19 and in 7.3% (n=79) women with serological features of acute
toxoplasmosis. In 8.5% (n=28) of the patients with IgM anti-PVB19 and 9% (n=5) of the
pregnant women with IgM and/or IgA anti-T.gondii, fetal hydrops was detected.
Intrauterine death was diagnosed in 4.5% (n=15) of the cases with acute PVB19 infection
and in 2.3% (n=6) of the patients with acute toxoplasmosis. Amniotic fluid disorders
were noticed more often in women with acute parvovirosis (polihydramnion 15.5%,
n=51; oligohydramnion 8.5%, n=28; ahydramnion 6.3%, n=21) than in those with active
toxoplasmosis (polihydramnion 3.4%, n=9; oligohydramnion 3.4%, n=9; ahydramnion
0%). We have examined also the influence of T.gondii and PVB19 infections on an
intrauterine growth restriction, preterm delivery, and spontaneous abortions. Conclusions:
In conclusion, infections of T.gondii and PVB19 are a very common cause of
complications in pregnancy. Due to high prevalence rate of IgG antibodies in Poland, it is
necessary to consider routine serological testing in pregnancy.
PMID: 18592853
20. A case of congenital hydrocephalus associated with fetal intraventricular
hemorrhage.“
Korean J Perinatol. 2008 Sep; 19 (3): 303-307.
Choi SK, Jeong YJ, Lee SY, Choi JS, Wee JS, Ahn HY, Shin JC.
Department of Obstetrics and Gynecology, College of Medicine Catholic University of
Korea, Seoul, Korea. (Email: jcshin@catholic.ac.kr).
Intraventricular hemorrhage is common in premature infants, and post-hemorrhagic
hydrocephalus may follow. Rarely, intraventricular hemorrhage can occur in utero and
may lead to congenital hydrocephalus. In most cases no underlying disease is identified.
The fetus may be compromised by intrauterine hypoxia leading to hemorrhage. Fetal
hydrocephalus can be identified by ultrasonography, but the hemorrhagic lesion can be
identified with high sensitivity by magnetic resonance imaging. There are neurologic
deficit in neonate with fetal hydrocephalus. Early surgical treatment is recommended for
neurodevelopmental outcome. We experienced a case of congenital hydrocephalus
associated with fetal intraventricular hemorrhage in our hospital. We report the case with
a brief review of the literature.
PMID: N/A
Link: http://www.koreamed.org/SearchBasic.php?DT=1&RID=505302
21.Fetal hydrocephalus caused by cryptic intraventricular hemorrhage.
Brain Pathol. 2010 Mar; 20 (2): 391-8. Epub 2009 May 20.
Lategan B, Chodirker BN, Del Bigio MR.
Department of Pathology, University of Manitoba and Health Sciences Centre, Winnipeg,
Canada.
Cryptic intracerebral hemorrhage as an etiological factor in fetal hydrocephalus has been
postulated but not described at autopsy. Four fetuses with overt hydrocephalus diagnosed
by in utero ultrasound examination were examined at autopsy at 19-22 weeks gestation.
Although a hemorrhagic etiology was not evident on ultrasound, hemosiderin-containing
macrophages and associated reactive changes were found to obstruct the otherwise wellformed cerebral aqueduct in all four. Coagulopathy due to thrombocytopenia was
implicated in one case. Anomalies involving other parts of the body were identified in
two cases, although a direct link to the hydrocephalus was not obvious. The abnormality
was isolated in one case. In three cases, possible sites of hemorrhage in the ventricles
were identified. This abnormality represents a significant proportion of the fetuses
examined for hydrocephalus in our referral center. We discuss the importance of careful
autopsy examination in the diagnosis of cryptic intracerebral hemorrhage and the
implications for counseling.
PMID: 19476
22.Fetal hydrocephalus in a pregnancy complicated by idiopathic thrombocytopenic
purpura.
J Ultrasound Med. 2006 Jun; 25 (6): 777-80.
Kim MW, Choi HM.
Department of Obstetrics and Gynecology, Inje University Ilsanpaik Hospital, Goyang-si,
Gyeonggi-do 411-706, Korea.
Idiopathic thrombocytopenic purpura (ITP) is an autoimmune disorder in which the
platelets of patients are destroyed by autoantibodies. It commonly affects young women,
and obstetricians frequently come across these patients. There have been concerns about
whether vaginal delivery may predispose the fetus to intracranial hemorrhage, and it has
led many obstetricians to use cesarean delivery to prevent intracranial bleeding. The
incidence of intracranial hemorrhage, however, in neonates born to the mother with ITP
has been reported to be less than 1%. Moreover, intrauterine intracranial hemorrhage
regardless of mechanical stress at delivery seems to be very rare. We report a pregnancy
complicated by ITP in which intrauterine intracranial hemorrhage was diagnosed
prenatally in the third trimester.
PMID: 16731895
23.Congenital posthemorrhagic hydrocephalus: A case of fetomaternal alloimmune
thrombocytopenia.
Fetal Diagn Ther. 2007; 22 (5): 321-4. Epub 2007 Jun 5.
Póvoa AM, Ramalho C, Machado AP, Matias A, Montenegro N.
Prenatal Diagnosis Center, Department of Gynecology and Obstetrics, Cardiovascular I
& D Unit, Medical Faculty of Porto, Hospital S. João, Porto, Portugal. (Email:
amargpf@hotmail.com).
Fetal/neonatal alloimmune thrombocytopenia (NAIT) results from fetomaternal
mismatch for human platelet alloantigens leading to antibody-mediated destruction of
fetal platelets. This is one of the most common causes of severe thrombocytopenia in the
newborn with an incidence of 1/800-1,000. In the most severe cases, NAIT may result in
intracranial hemorrhage and may lead to death or neurologic sequelae. We report a case
of fetal hydrocephalus caused by NAIT and discuss the importance of making an accurate
prenatal diagnosis to improve the management of the current pregnancy and the outcome
of subsequent pregnancies. Screening of female siblings of affected cases is
recommended in order to detect at-risk individuals. Copyright 2007 S. Karger AG, Basel.
PMID: 17556816
24. Warfarin-induced fetal intracranial subdural hematoma.
[Note: Article discusses Hydrocephalus].
J Clin Ultrasound. 2008 Sep; 36 (7): 451-3.
Oswal K, Agarwal A.
NCS Diagnostics, P-41, Kishore Vidya Vinode Avenue, Baghbazar, Kolkata.
Antenatal intracranial hemorrhage is a rare cause of intrauterine fetal death, with an
incidence of 4.6-5.1% in autopsy studies of stillborn fetuses. Warfarin-associated fetal
bleeding is also a rare problem, with an incidence of 4.3% in the literature. We present a
case of warfarin-induced subdural hematoma occurring in the second trimester. (c) 2008
Wiley Periodicals, Inc.
PMID: 18361465
25. Genetics of human hydrocephalus.
[Literature Review].
J Neurol. 2006 Oct; 253 (10): 1255-66. Epub 2006 Jun 13.
Zhang J, Williams MA, Rigamonti D.
Dept. of Neurosurgery, The Johns Hopkins University School of Medicine, 600 N. Wolfe
Street, Phipps 100, Baltimore, MD 21287, USA. (Email: jhzhang@jhmi.edu).
Human hydrocephalus is a common medical condition that is characterized by
abnormalities in the flow or resorption of cerebrospinal fluid (CSF), resulting in
ventricular dilatation. Human hydrocephalus can be classified into two clinical forms,
congenital and acquired. Hydrocephalus is one of the complex and multifactorial
neurological disorders. A growing body of evidence indicates that genetic factors play a
major role in the pathogenesis of hydrocephalus. An understanding of the genetic
components and mechanism of this complex disorder may offer us significant insights
into the molecular etiology of impaired brain development and an accumulation of the
cerebrospinal fluid in cerebral compartments during the pathogenesis of hydrocephalus.
Genetic studies in animal models have started to open the way for understanding the
underlying pathology of hydrocephalus. At least 43 mutants/loci linked to hereditary
hydrocephalus have been identified in animal models and humans. Up to date, 9 genes
associated with hydrocephalus have been identified in animal models. In contrast, only
one such gene has been identified in humans. Most of known hydrocephalus gene
products are the important cytokines, growth factors or related molecules in the cellular
signal pathways during early brain development. The current molecular genetic evidence
from animal models indicate that in the early development stage, impaired and abnormal
brain development caused by abnormal cellular signaling and functioning, all these
cellular and developmental events would eventually lead to the congenital hydrocephalus.
Owing to our very primitive knowledge of the genetics and molecular pathogenesis of
human hydrocephalus, it is difficult to evaluate whether data gained from animal models
can be extrapolated to humans. Initiation of a large population genetics study in humans
will certainly provide invaluable information about the molecular and cellular etiology
and the developmental mechanisms of human hydrocephalus. This review summarizes
the recent findings on this issue among human and animal models, especially with
reference to the molecular genetics, pathological, physiological and cellular studies, and
identifies future research directions.
PMID: 16773266
26. Molecular mechanisms and neuroimaging criteria for severe L1 syndrome with Xlinked hydrocephalus.
J Neurosurg. 2006 Nov; 105 (5 Suppl): 403-12.
Kanemura Y, Okamoto N, Sakamoto H, Shofuda T, Kamiguchi H, Yamasaki M.
Institute for Clinical Research and Department of Neurosurgery, Osaka National
Hospital, Osaka, Japan.
Object: Mutations in the gene that codes for the human neural cell adhesion molecule L1
(L1CAM), are known to cause a wide variety of anomalies, now understood as
phenotypic expressions of L1 syndrome. The correlations between genotype and
phenotype, however, are not fully established. The authors report the results of a
nationwide investigation of L1CAM gene mutations that was performed to improve the
understanding of L1-mediated molecular mechanisms of X-linked hydrocephalus and to
establish neurorimaging criteria for this severe form of L1 syndrome. Methods: Ninetysix genomic DNA samples from members of 57 families were obtained from the
Congenital Hydrocephalus Research Committee. By using polymerase chain reaction and
direct DNA sequencing, the authors identified 25 different L1CAM gene mutations, 20 of
them novel, in 26 families with X-linked hydrocephalus. All the mutations were L1CAM
loss-of-function mutations, and all the patients had severe hydrocephalus and severe
mental retardation. In all cases, specific abnormalities were visible on neuroimaging: a
rippled ventricular wall after shunt placement, an enlarged quadrigeminal plate, a large
massa intermedia, and hypoplasia of the cerebellar vermis (anterior or total). The patients
also had adducted thumbs, spastic paraplegia, and hypoplasia of the corpus callosum,
which are characteristic of L1 syndrome. Conclusions: The L1CAM loss-of-function
mutations cause a severe form of L1 syndrome, unlike the milder form produced by
mutations in the L1CAM cytoplasmic domain. We also identified neurorimaging criteria
for this severe form of L1 syndrome. These criteria can be used to predict loss-offunction mutations in patients with X-linked hydrocephalus and to help in diagnosing this
syndrome.
PMID: 17328266
27. Prenatal diagnosis in a family with X-linked hydrocephalus.
Prenat Diagn. 2005 Oct; 25 (10): 930-3.
Panayi M, Gokhale D, Mansour S, Elles R.
National Genetics Reference Laboratory, Regional Genetics Service, St Mary's Hospital,
Manchester, UK. (Email: maria.panayi@cmmc.nhs.uk).
The neural cell adhesion molecule L1 is a transmembrane glycoprotein belonging to the
immunoglobulin superfamily of cell adhesion molecules (CAMs). Its expression is
essential during embryonic development of the nervous system and it is involved in
cognitive function and memory. Mutations in the L1CAM gene are responsible for four
related L1 disorders; X-linked hydrocephalus/HSAS (Hydrocephalus as a result of
Stenosis of the Aqueduct of Sylvius), MASA (Mental retardation, Aphasia, Shuffling
gait, and Adducted thumbs) syndrome, X-linked complicated spastic paraplegia type I
(SPG1) and X-linked Agenesis of the Corpus Callosum (ACC). These four disorders
represent a clinical spectrum that varies both between and within families. The main
clinical features of this spectrum are Corpus callosum hypoplasia, mental Retardation,
Adducted thumbs, Spastic paraplegia and Hydrocephalus (CRASH syndrome). Since
there is no biochemically assayed disease marker, molecular analysis of the L1CAM gene
is the only means of confirming a clinical diagnosis. Most L1CAM mutations reported to
date are point mutations (missense, nonsense, splice site) and only a few patients with
larger rearrangements have been documented. We have characterised a rare intragenic
deletion of the L1CAM gene in a sample of DNA extracted from a chorionic villus
biopsy (CVB) performed at 12 weeks' gestation. Copyright 2005 John Wiley & Sons,
Ltd.
PMID: 16088863
28. A novel L1CAM mutation in a fetus detected by prenatal diagnosis.
Eur J Pediatr. 2010 Apr; 169 (4): 415-9. Epub 2009 Aug 16.
Piccione M, Matina F, Fichera M, Lo Giudice M, Damiani G, Jakil MC, Corsello G.
U.O. Pediatria e Terapia Intensiva Neonatale, Dipartimento Materno Infantile, Università
degli Studi di Palermo, Palermo, Italy. (Email: piccionemaria@libero.it).
X-linked hydrocephalus is due to mutations in the L1 neuronal cell adhesion molecule
(L1CAM) gene. L1 protein plays a key role in neurite outgrowth, axonal guidance, and
pathfinding during the development of the nervous system. We report on a familial case
diagnosed by prenatal ultrasonographic examination, with cerebellar hypoplasia, agenesis
of the corpus callosum, and the bilateral overlapping of the second and third fingers of
the hand. Sequencing of the L1CAM gene showed a novel missense mutation in exon 14:
transition of a guanine to cytosine at position 1777 (c.1777G>C), which led to an amino
acid change of alanine to proline at position 593 (Ala593Pro) in the sixth
immunoglobulin domain of the L1 protein. The L1CAM mutation testing should be
considered in fetuses with ultrasonographic signs of hydrocephalus and a positive family
history compatible with X-linked inheritance. We agree with previous reports that
suggest also considering limb abnormalities other than adducted thumbs in addition to
classical neurological disgenesis, as characteristic for L1-disease.
PMID: 19685344
29. Fanconi anaemia complementation group B presenting as X linked VACTERL with
hydrocephalus syndrome.
J Med Genet. 2006 Sep; 43 (9): 750-4. Epub 2006 May 5.
Holden ST, Cox JJ, Kesterton I, Thomas NS, Carr C, Woods CG.
Department of Clinical Genetics, 7th Floor New Guy's House, Guy's Hospital, St Thomas
Street, London SE1 9RT, UK. (Email: simon.holden@gstt.nhs.uk).
Background: The VACTERL with hydrocephalus (VACTERL-H) phenotype is
recognised to be a severe manifestation of autosomal recessive Fanconi anaemia. Several
families have been described in which the VACTERL-H phenotype segregates as an X
linked syndrome. The mutations which cause X linked VACTERL-H syndrome are not
known. Objective: To determine if mutations in FANCB, which are known to cause
Fanconi anaemia complementation group B, are a cause of X linked VACTERL-H
syndrome. Methods: A three generation pedigree with X linked VACTERL-H syndrome
was investigated. X inactivation was tested in carrier females, and fibroblasts from an
affected male fetus were analysed for increased sensitivity to diepoxybutane. FANCB
coding exons and flanking splice sites were screened for mutations by direct sequencing
of polymerase chain reaction (PCR) fragments amplified from genomic DNA. cDNA
from affected fetal fibroblasts was analysed by PCR and direct sequencing using specific
exonic primers. Results: A FANCB mutation which results in a premature stop codon by
causing skipping of exon 7 was identified. Chromosomes from the affected fetus showed
increased sensitivity to diepoxybutane, and carrier women were found to have 100%
skewed X inactivation in blood. Conclusions: Mutations in FANCB are a cause of X
linked VACTERL-H syndrome. The data presented are of relevance to the genetic
counselling of families with isolated male cases of VACTERL-H and Fanconi anaemia.
PMID: 16679491
30. Ring chromosome 6 in three fetuses: Case reports, literature review, and implications
for prenatal diagnosis.
[Literature Review].
Am J Med Genet. 2002 Mar 1; 108 (2): 97-104.
Urban M, Bommer C, Tennstedt C, Lehmann K, Thiel G, Wegner RD, Bollmann R,
Becker R, Schulzke I, Körner H.
Institut für Medizinische Genetik, Universitätsklinikum Charité, Humboldt-Universität
zu, Berlin, Germany.
Prenatal and postnatal findings in three fetuses with a ring chromosome 6 are presented,
and the literature of this rare cytogenetic disorder is reviewed. The described fetuses
illustrate the broad spectrum of the clinical manifestation of ring chromosome 6. In one
fetus, the disorder was diagnosed incidentally by a routine amniocentesis due to advanced
maternal age. The other two fetuses were hydrocephalic and had other congenital
anomalies. Remarkably, the ring chromosome 6 tends to disappear in cultured amniotic
fluid cells; karyotyping revealed complete or nearly complete monosomy 6. In contrast,
the ring was preserved in high proportions of fetal leukocytes. Postnatal growth
retardation is the only consistent finding of this chromosomal disorder. Maternal age is
not significantly above average. An additional review of 20 literature cases revealed a
striking tendency to hydrocephalus, either due to deficient brain growth or secondary to
an aqueductal stenosis. Children with hydrocephalus and ring chromosme 6 tend to
display facial dysmorphism and may have additional malformations, growth failure, eye
anomalies, and seizures. In contrast, there are two reports on children with a ring
chromosome 6 who had short stature, normal appearance, and a normal or almost-normal
psychomotor development. In such patients at the mild end of the clinical spectrum, the
phenotype is basically restricted to what Kosztolányi. [1987: Hum Genet 75:174-179]
delineated as ring syndrome, comprising severe growth failure without major
malformations, without a specific deletion syndrome, with only a few or no minor
anomalies, and mild to moderate mental retardation. This ring syndrome is considered to
occur independently of the autosome involved in the ring formation. The overall
impression from our cases and from the literature review of cases with ring chromosome
6 is that the karyotype-genotype correlation is poor. This makes prognostic counseling of
parents difficult and unsatisfactory. Serial targeted ultrasound examinations, especially of
the brain, are decisive factors in elucidating the prognosis.
PMID: 1185755
31. Diagnosis and management of unilateral third-trimester hydrocephalus: A
multidisciplinary approach.
Am J Perinatol. 2008 Sep; 25 (8): 499-502. Epub 2008 Aug 21.
Mastrobattista JM, Pschirrer ER, Kelley-Martinez M, Ross PJ.
Department of Obstetrics, Gynecology and Reproductive Sciences, University of Texas
Houston Medical School, Houston, Texas 77030-1501, USA. (Email:
joan.m.mastrobattista@uth.tmc.edu).
Hydrocephalus is a pathological increase in cerebrospinal fluid. This condition may occur
when production exceeds absorption. Prior reports describe prenatally diagnosed
unilateral hydrocephalus with varying outcomes depending on underlying brain
abnormalities, karyotypic abnormalities, and infection. Prenatal ultrasound is a valuable
diagnostic tool in the identification of hydrocephalus. Obstacles such as near-field
artifact, additional intracranial abnormalities, fetal positioning, and maternal habitus often
make the diagnosis difficult. Antenatal diagnosis is important for emotional preparation
and for transfer to a tertiary center where appropriate facilities and subspecialists are
available. We present a case of right-sided hydrocephalus and mild left-sided
ventriculomegaly diagnosed in the third trimester. Fetal brain magnetic resonance
imaging confirmed the sonographic diagnosis, which allowed the multidisciplinary fetal
team to meet with the patient and formulate a management plan prior to delivery.
PMID: 18720324
32. The role of ultrasonography in recognizing the cause of fetal cerebral
ventriculomegaly.
J Perinat Med. 2004; 32 (1): 5-12.
D'Addario V.
Fetal Medicine Unit, Department of Obstetrics and Gynecology, University of Bari, Italy.
(Email: v.daddario@gynecology4.uniba.it).
Dilatation of the fetal cerebral ventricles (ventriculomegaly) is a generic sonographic sign
common to several pathological entities carrying different prognoses. The main causes of
fetal ventriculomegaly are aqueductal stenosis, Chiari II malformation, Dandy-Walker
complex, and agenesis of the corpus callosum. Ventriculomegaly is easily recognized by
ultrasound by measuring the atrial width.T his simple measure allows the recognition of
mild forms of ventricular dilatation and is used as a screening method for
ventriculomegaly. However, although the diagnosis of ventriculomegaly is easy, the
prenatal identification of the cause of ventricular dilatation is a more difficult task.To this
end, the evaluation of the posterior fossa in association with the visualization of the
corpus callosum is a useful landmark. Research into the cause of ventriculomegaly is
clinically useful, since the prognosis mainly depends on the etiology and on the presence
of associated anomalies.In this article, the role of prenatal sonography in recognizing the
cause of ventriculomegaly and the prognostic value of the prenatal sonographic findings
are discussed.
PMID: 15008380
33. Sonographic diagnosis of fetal cerebral ventriculomegaly: An update.
[Literature Review].
J Matern Fetal Neonatal Med. 2007 Jan; 20 (1): 7-14.
D'Addario V, Pinto V, Di Cagno L, Pintucci A.
Fetal Medicine Unit, Department of Obstetrics and Gynecology, University Medical
School, Bari, Italy. (Email: v.daddario@gynecology4.uniba.it).
Dilatation of the fetal cerebral ventricles (ventriculomegaly) is a generic sonographic sign
that is common to several pathological entities carrying different prognoses. The main
causes of fetal ventriculomegaly are aqueductal stenosis, Chiari II malformation, DandyWalker complex, and agenesis of the corpus callosum. Ventriculomegaly is easily
recognized by ultrasound by measuring the atrial width. This simple measure allows the
recognition of mild forms of ventricular dilatation and is used in screening for
ventriculomegaly. However, although the diagnosis of ventriculomegaly is easy, the
prenatal identification of the cause of ventricular dilatation is a more difficult task. For
this purpose the evaluation of the posterior fossa in association with the visualization of
the corpus callosum is useful. Research into the causes of ventriculomegaly is clinically
useful, since the prognosis mainly depends on the etiology and on the presence of
associated abnormalities.I n this article, the role of prenatal sonography in determining
the cause of the ventriculomegaly is reviewed, as well as the prognostic value of the
prenatal sonographic findings.
PMID: 17437193
34. Ultrasound of the fetal brain. Ultrasound Clinics. 2007 April; 2 (2): 217-244.
A, Timor-Tritsch IE.
Department of Obstetrics and Gynecology, NYU School of Medicine, 530 First Avenue,
NB9N26, New York, NY 10016, USA. (Email: ana.monteagudo@med.nyu.edu).
Ultrasound examination of the fetal central nervous system (CNS) distinguishes itself
from the sonographic evaluation of all other organs or organ systems because during the
course of pregnancy, the CNS (mainly the fetal brain) undergoes significant changes, in
size and in the shape of its different anatomic regions, which follow a well-defined
timeline and can be recognized sonographically. The developmental milestones of the
CNS from the time of its first sonographic detection to term can, and should, be taken
into consideration when a fetal neurosonogram is performed. This article describes a
systematic approach to the evaluation of the fetal brain by discussing the differential
diagnosis of two important sonographic findings, namely ventriculomegaly and an
enlarged posterior fossa, and by touching on other important brain abnormalities.
PMID: N/A
Link: http://www.jvir.org/article/S1556-858X(07)00065-5/abstract
35. The midsagittal view of the fetal brain:A useful landmark in recognizing the cause of
fetal cerebral ventriculomegaly.
J Perinat Med.2005; 33 (5): 423-7.
D'Addario V, Pinto V, Di Cagno L, Pintucci A.
Fetal Medicine Unit, Department of Obstetrics and Gynecology, University Medical
School, Bari, Italy. (Email: vdaddario@gynecology4.uniba.it).
Aim:To evaluate the positive predictive value of the midsagittal view of the fetal brain in
recognizing the cause of ventriculomegaly diagnosed with traditional axial scan.
Methods:Fifty-eight pregnant women, referred to our Center following a generic
diagnosis of ventriculomegaly have been evaluated: 38 had marked and 20 had borderline
ventriculomegaly. The fetal brain was scanned by the midsagittal view using a
transabdominal probe in fetuses in breech presentation or transverse lie and a transvaginal
probe in fetuses in cephalic presentation. The possible cause of ventriculomegaly was
postulated by combining the findings of the corpus callosum/cavum septi pellucidi
complex with those of the posterior fossa.The prenatal diagnoses were compared with the
anatomical specimens of aborted fetuses or with postnatal neuroimaging. Results: The
prenatal diagnoses were confirmed in 54/58 cases (PPV 93.1%).In the marked
ventriculomegaly group, one case of partial agenesis of the corpus callosum was
mistaken for a complete agenesis.In the group of borderline ventriculomegaly, two cases
of partial agenesis of the corpus callosum were confused with a complete agenesis, while
one case of suspected isolated ventriculomegaly was diagnosed after birth as partial
agenesis of the corpus callosum. Conclusions:The sagittal scan of the fetal brain is a
useful source of information and allows the contemporary view of both corpus callosum
and posterior fossa, where various typical sonographic findings are present in
ventriculomegaly.
PMID: 16238537
36. Differential diagnosis in fetuses with absent septum pellucidum.
Ultrasound Obstet Gynecol. 2005 Jan; 25 (1): 42-9.
Malinger G, Lev D, Kidron D, Heredia F, Hershkovitz R, Lerman-Sagie T.
Fetal Neurology Unit, Department of Obstetrics and Gynecology, Edith Wolfson Medical
Center, Holon 58100, Israel. (Email: malinger@inter.net.il).
Objective: To elucidate the characteristic morphological features that may help in the
prenatal differential diagnosis of absent septum pellucidum as demonstrated by
ultrasound. Methods: Twenty-six fetuses were referred to the fetal neurology clinic due to
mild to severe ventriculomegaly and a connection between the lateral ventricles. The
following ultrasonographic features were evaluated: place and extent of the ventricular
communication, non-cleavage of the hemispheres and deep gray nuclei, callosal
anomalies, position of the choroid plexus, and other central nervous system and facial or
body anomalies. A flowchart was created in order to facilitate the final diagnosis.
Results: The presence of non-cleavage and/or characteristic facial anomalies prompted
the diagnosis of holoprosencephaly (HPE) in 14 fetuses, including two fetuses with the
middle interhemispheric variant. Ten fetuses were diagnosed as having hydrocephalus
based on the lack of the same features and the observation that the communication
between the lateral ventricles was at the level of the third ventricle with almost normal
anterior and posterior segments. In two fetuses the diagnosis of septo-optic dysplasia vs.
isolated agenesis of the cavum septi pellucidi was contemplated. Conclusions: The use of
the proposed flowchart enabled differentiation between hydrocephalus and HPE. The
communication between the ventricles in hydrocephalic fetuses may be due to a
disruption of the septum pellucidum or to a pathological enlargement of the foramen of
Monro. Published by John Wiley & Sons, Ltd. Copyright (c) 2004 ISUOG.
PMID: 15593321
37. Frequency and cause of disagreements in diagnoses for fetuses referred for
ventriculomegaly.
Radiology.2008 May; 247 (2): 516-27.
Levine D, Feldman HA, Tannus JF, Estroff JA, Magnino M, Robson CD, Poussaint TY,
Barnewolt CE, Mehta TS, Robertson RL.
Department of Radiology, Beth Israel Deaconess Medical Center, 330 Brookline Ave,
Boston, MA 02215, USA. (Email: dlevine@caregroup.harvard.edu).
Purpose:To prospectively assess the frequency and cause of disagreements in diagnoses
at ultrasonography (US) and magnetic resonance (MR) imaging for fetuses referred for
ventriculomegaly (VM).Materials and Methods: One hundred ninety-five women, aged
18-44 years, with 200 fetal referrals for VM, were recruited in a prospective IRB-
approved, HIPAA-compliant study.Written informed consent was obtained.US scans
were prospectively interpreted by three obstetric radiologists and MR examinations were
read by one obstetric radiologist and three pediatric neuroradiologists. Final diagnosis
was reached by consensus (198 US, 198 MR, and 196 US-MR comparisons).Gestational
age, ventricular size, types of disagreements, and reasons for disagreements were
recorded. Interreader agreement was assessed with kappa statistics. Ventricular diameter,
gestational age, and confidence scores were analyzed by using mixed-model analysis of
variance, accounting for correlation within reader and fetus. Results:There was
prospective agreement on 118 (60%) of 198 US and 104 (53%) of 198 MR readings.
Consensus was more likely when the final diagnosis was isolated VM (83 of 104, 80% at
US; 82 of 109, 75% at MR) than when the final diagnosis included other anomalies as
well (14 of 63, 22% at US; seven of 68, 10% at MR; P < .001).There was disagreement
on 19 (10%) of 196 and 31 (16%) of 196 fetuses about the presence of VM at US and
MR, respectively, and on 29 (15%) of 198 and 39 (20%) of 198 fetuses regarding the
presence of major findings at US and MR, respectively.Reasons for discrepancies in
reporting major findings included errors of observation, lack of real-time US scanning,
lack of neuroradiology experience, as well as modality differences in helping depict
abnormalities. Conclusion:Of radiologists who read high-risk obstetric US and fetal MR
images for VM, there is considerable variability in central nervous system diagnosis. (c)
RSNA, 2008.
PMID: 18430880
Link for Full Text:
http://radiology.rsna.com/content/247/2/516.full
38. Craniospinal malformations in a twelve-year fetopathological study: The efficiency of
ultrasonography in view of fetopathological investigations.
Early Hum Dev. 2008 Feb; 84 (2): 115-9. Epub 2007 May 7.
Joó JG, Beke A, Szigeti Z, Csaba A, Mezei G, Tóth-Pál E, Papp C.
1st Department of Obstetrics and Gynecology, Semmelweis University Medical School,
Budapest, Hungary. (Email: joogabor@hotmail.com).
Background: Craniospinal malformations represent a heterogeneous group of congenital
malformations by their morphology and etiology alike. Certain craniospinal
malformations could be diagnosed as early as the dawn of ultrasonography and this group
of malformations has been the focus of attention ever since. Aims: The aim of the authors
was to review the main characteristics of craniospinal malformations, as well as to
evaluate the efficiency of ultrasonography based on autopsy examinations during twelve
years. Study Design: The current study comprises the details of 339 pregnancies
terminated by induced abortion for craniospinal malformation between 1995 and 2006.
Results: Maternal median age was 27+/-5.8 years, ranging from 15 to 47 years. In 24.5%
of the cases, there was a positive obsterical-gynecological or genetic history. In 68.1% of
the cases, ultrasonographic and autopsy findings were completely identical; in 24.2% a
partial coincidence was found, but autopsy allowed for further diagnoses, while in 26
cases (7.7%) different findings were obtained by prenatal ultrasonography and
fetopathological investigations. In half of the latter 26 cases, induced abortion was
suggested due to hydrocephalus confirmed by ultrasonography but not justified by
autopsy or the autopsy revealed the presence of other craniospinal malformation(s).
Conclusion: It can be concluded that - in view of the diagnostic efficiency of
fetopathological investigations - the ultrasonographic diagnosis of hydrocephalus should
be interpreted independently from other craniospinal malformations on the basis of
principles of ultrasonographic methodology and at different times.
PMID: 17482389
39. Correlation between ultrasound and autopsy findings after 2nd trimester terminations
of pregnancy.
J Perinat Med. 2008; 36 (1): 59-69.
Antonsson P, Sundberg A, Kublickas M, Pilo C, Ghazi S, Westgren M, Papadogiannakis
N.
Center for Perinatal Pathology, Karolinska University Hospital, Stockholm, Sweden.
Objective: To compare ultrasound (US) and fetal autopsy findings in 2(nd) trimester
termination of pregnancy because of structural fetal anomalies. Methods: A total of 112
terminations of pregnancy (TOP) between 1999-2003 were reviewed retrospectively. The
cases originated from a secondary and a tertiary Fetal Medicine unit in the south
Stockholm area, using a common specialized perinatal pathology service. Karyotype was
not known at the time of US examination. The findings were compared and classified
into four groups according to the degree of agreement between US and autopsy. Results:
In 45% of cases there was total agreement between US and autopsy. In 40%, autopsy
confirmed all US findings but provided additional information of clinical importance.
Partial or total lack of agreement was noted in 11% and 4% of the cases, respectively.
Areas of discrepancy involved mainly CNS- and cardiovascular abnormalities and, to a
lesser extent, renal anomalies, abdominal wall defects and hydrops/hygroma. Regarding
CNS abnormalities the overall rate of agreement was 62%; it was highest in
acrania/anencephaly (92%) and lowest in hydrocephaly (39%). Conclusion: We find an
overall high degree of agreement between US and autopsy findings. Autopsy often
provided additional information of clinical value and it should always follow US
examination and TOP. Fixation of CNS is crucial for optimal results. Specific limitations
of autopsy, i.e., detection of CNS abnormalities, may be reduced by complementary
imaging techniques, such as MRI. The ability of US to detect cardiac anomalies is
enhanced with the close contact to specialized fetal cardiology.
PMID: 18184098
40. Potential pitfalls in fetal neurosonography.
[Literature Review].
Prenat Diagn. 2006 Jan; 26 (1): 52-6.
Correa FF, Lara C, Bellver J, Remohí J, Pellicer A, Serra V.
Unidad de Pediatría, Instituto Universitario Valenciano de Infertilidad, Universidad de
Valencia, Valencia, Spain. (Email: ummf@ivi.es ).
Objective:To present anatomic variants of the fetal brain and artifacts related to scanning
techniques that could be misinterpreted as abnormalities on prenatal neurosonographic
studies.Methods:The findings were derived from fetal neurosonographic studies
performed routinely from 16 to 36 weeks' gestation during the last 3 years, supervised by
a sonologist specialized in neonatal cranial sonography. Results:The pitfalls were divided
into three groups:brain parenchyma, ventricular system, and choroid plexus.We provide
images of these pseudolesions and clues to their differentiation from true brain
pathology.Conclusions:Knowledge of misleading images seen on fetal neurosonographic
studies that could be misinterpreted as lesions is essential for the proper interpretation of
these studies and will help avoid the use of more invasive diagnostic tests.To the best of
our knowledge, the majority of the pitfalls presented here have only been described in
neonates.
PMID: 16378322
41. Fetal intracranial hemorrhage (fetal stroke): Report of four antenatally diagnosed
cases and review of the literature.
[Literature Review].
Taiwan J Obstet Gynecol. 2006 Jun; 45 (2): 135-41.
Huang YF, Chen WC, Tseng JJ, Ho ES, Chou MM.
Department of Obstetrics and Gynecology, Taichung Veterans General Hospital,
Taichung, Taiwan.
Objective: Neonatal intracranial hemorrhage (ICH) has been estimated to be high in
premature infants, occurring in approximately 40% of infants of less than 32 weeks'
gestation. However, the true incidence of ICH in utero has not been determined. We
present our experience with four cases of fetal ICH (fetal stroke), which was detected
prenatally by ultrasonography (US). Materials and Methods: Four cases of fetal ICH were
identified over a 2-year period at the prenatal unit of Taichung Veterans General
Hospital, Taiwan. Prenatal and neonatal sonograms, computed tomography (CT) scan or
magnetic resonance imaging (MRI), medical records, and the clinical course were
assessed retrospectively. In each case, a series of initial and follow-up obstetric
sonograms were available. Fetal stroke was recognized by several sonographic features:
irregular echogenic brain mass, intraventricular echogenic foci or periventricular
echodensities; ventriculomegaly; and posthemorrhagic hydrocephalus (PHH). A detailed
investigation for possible etiology of fetal ICH was performed in all cases. Results:
Transabdominal US showed hyperechoic lesions in the lateral ventricle and
ventriculomegaly in three of the four fetuses, and a massive intraparenchymal
hemorrhage in the remaining one. Three fetuses were born vaginally and one by cesarean
section due to an enlarged head circumference. Abnormal nonstress tests and abnormal
flow velocity waveforms in the umbilical and middle cerebral arteries were present in
two cases. Intrapartum fetal death and neonatal death occurred in the first two cases
associated with maternal preeclampsia at 31 and 27 weeks, respectively. In the remaining
two infants, the one in case 3 underwent ventriculoperitoneal shunting, which developed
normally at the age of 18 months. The other infant in case 4 had PHH after suspicious
choroids plexus hemorrhage, and the detailed information regarding the cause of neonatal
death was not available. Conclusion: This small series demonstrate that an antenatal
diagnosis of fetal stroke with intraventricular hemorrhage Grades III and IV or with brain
parenchymal involvement appears to be associated with poor neurologic outcome. Due to
the significant neonatal neurologic impairment and potential medicolegal implications of
antepartum fetal ICH, it follows that obstetricians and sonographers should be familiar
with predisposing factors and typical diagnostic imaging findings of rare in utero ICH
events.
PMID: 17197354
42. Sonographic findings in fetal viral infections: A systematic review.
Obstet Gynecol Surv. 2006 May; 61 (5): 329-36.
Degani S.
Department of Obstetrics and Gynecology, Bnei-Zion Medical Center, Ruth and Baruch
Rappaport Faculty of Medicine, Technion-Institute of Technology, Haifa, Israel. (Email:
sdegani@tx.technion.ac.il).
Viral infections are a major cause of fetal morbidity and mortality. Transplacental
transmission of the virus, even in subclinical maternal infection, may result in a severe
congenital syndrome. Prenatal detection of viral infection is based on fetal sonographic
findings and polymerase chain reaction to identify the specific infectious agent. Most
affected fetuses appear sonographically normal, but serial scanning may reveal evolving
findings. Common sonographic abnormalities, although nonspecific, may be indicative of
fetal viral infections. These include growth restriction, ascites, hydrops,
ventriculomegaly, intracranial calcifications, hydrocephaly, microcephaly, cardiac
anomalies, hepatosplenomegaly, echogenic bowel, placentomegaly, and abnormal
amniotic fluid volume. Some of the pathognomonic sonographic findings enable
diagnosis of a specific congenital syndrome (eg, ventriculomegaly and intracranial and
hepatic calcifications in cytomegalovirus, eye and cardiac anomalies in congenital rubella
syndrome, limb contractures and cerebral anomalies in varicella zoster virus). When
abnormalities are detected on ultrasound, a thorough fetal evaluation is recommended
because of multiorgan involvement. Target Audience: Obstetricians & Gynecologists,
Family Physicians. Learning Objectives: After completion of this article, the reader
should be able to recall that both clinical and subclinical maternal viral infections can
cross the placenta, explain that there are specific sonographic findings along with
laboratory findings to detect infectious agents, and state that when sonographic
abnormalities are detected fetal viral infections need to be considered.
PMID: 16635273
43. Three-dimensional sonographic evaluations of embryonic brain development.
J Ultrasound Med.2008 Jan; 27 (1): 119-24.
Kim MS, Jeanty P, Turner C, Benoit B.
Inner Vision Women's Ultrasound, Nashville, TN 37203, USA. (Email:
misuksmile@gmail.com).
Objective:The purpose of this presentation is to show 3-dimensional development of the
ventricles of the brain in early pregnancy, from 6 to 13 weeks, and to provide a reference
for early diagnosis of central nervous system anomalies such as hydrocephalus and
holoprosencephaly.Methods:From March 2007 to August 2007, 46 patients were
included.All patients had routine first-trimester 2- and 3-dimensional sonographic
examinations at the same time. All cases were examined with a Voluson 730 Expert or
Voluson E8 ultrasound scanner (GE Healthcare, Milwaukee, WI) using a 4- to 8- or 6- to
12-MHz transvaginal probe.Volumes were reviewed and analyzed with GE 4DView
release 6 software.After the inversion-rendering mode was selected, volumes were
dissected by the MagicCut function to show the ventricles. Results:A total of 34 volumes
from 7 to 12 complete gestational weeks were successfully dissected. Those before 7 and
after 12 weeks could not be dissected properly. The crown-rump length ranged from 12.7
to 68 mm. Twelve representative images of the rendered volumes in chronologic order
are shown. The brain volume dissections of 2 fetuses with ventriculomegaly and alobar
holoprosencephaly are shown for comparison. Conclusions:Early human brain ventricular
structures could be evaluated in vivo with 3-dimensional sonography.T his presentation
shows the timeline of brain development and provides reference images to compare
possible anomalies of development.
PMID: 18096737
44.Examination of the fetal brain by transabdominal three-dimensional ultrasound:
Potential for routine neurosonographic studies.
Ultrasound Obstet Gynecol.2006 May; 27 (5): 503-8.
Correa FF, Lara C, Bellver J, Remohí J, Pellicer A, Serra V.
Unidad de Pediatría, Instituto Valenciano de Infertilidad (IVI), Universidad de Valencia,
Valencia, Spain. (Email: ummf@ivi.es).
Objective:To evaluate the role of transabdominal three-dimensional (3D) ultrasound in
the assessment of the fetal brain and its potential for routine neurosonographic
studies.Methods:We studied prospectively 202 consecutive fetuses between 16 and 24
weeks' gestation.A 3D ultrasound volume of the fetal head was acquired
transabdominally. The entire brain anatomy was later analyzed using the multiplanar
images by a sonologist who was expert in neonatal cranial sonography. The quality of the
conventional planes obtained (coronal, sagittal and axial, at different levels) and the
ability of the 3D multiplanar neuroscan to visualize properly the major anatomical
structures of the brain were evaluated. Results:Acceptable cerebral multiplanar images
were obtained in 92% of the cases.The corpus callosum could be seen in 84% of the
patients, the fourth ventricle in 78%, the lateral sulcus (Sylvian fissure) in 86%, the
cingulate sulcus in 75%, the cerebellar hemispheres in 98%, the cerebellar vermis in
92%, the medulla oblongata in 97% and the cavum vergae in 9% of them.The thalami
and the cerebellopontine cistern (cisterna magna) were identified in all cases.At or
beyond 20 weeks, superior visualization (in > 90% of cases) was achieved of the cerebral
fissures, the corpus callosum (97%), the supracerebellar cisterns (92%) and the third
ventricle (93%).Some cerebral fissures were seen initially at 16-17
weeks.Conclusion:Multiplanar images obtained by transabdominal 3D ultrasound provide
a simple and effective approach for detailed evaluation of the fetal brain anatomy.This
technique has the potential to be used in the routine fetal anomaly scan.
PMID: 16586474