Comparison of Success and Morbidity (Draft Correction) 14.08.12
advertisement
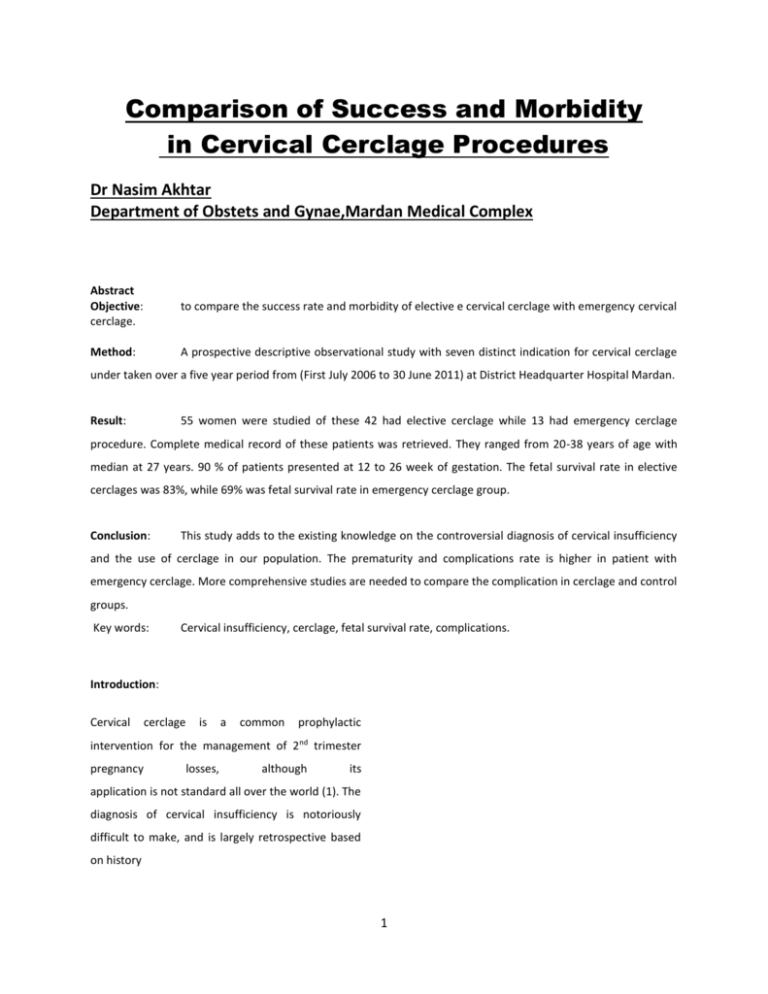
Comparison of Success and Morbidity in Cervical Cerclage Procedures Dr Nasim Akhtar Department of Obstets and Gynae,Mardan Medical Complex Abstract Objective: cerclage. to compare the success rate and morbidity of elective e cervical cerclage with emergency cervical Method: A prospective descriptive observational study with seven distinct indication for cervical cerclage under taken over a five year period from (First July 2006 to 30 June 2011) at District Headquarter Hospital Mardan. Result: 55 women were studied of these 42 had elective cerclage while 13 had emergency cerclage procedure. Complete medical record of these patients was retrieved. They ranged from 20-38 years of age with median at 27 years. 90 % of patients presented at 12 to 26 week of gestation. The fetal survival rate in elective cerclages was 83%, while 69% was fetal survival rate in emergency cerclage group. Conclusion: This study adds to the existing knowledge on the controversial diagnosis of cervical insufficiency and the use of cerclage in our population. The prematurity and complications rate is higher in patient with emergency cerclage. More comprehensive studies are needed to compare the complication in cerclage and control groups. Key words: Cervical insufficiency, cerclage, fetal survival rate, complications. Introduction: Cervical cerclage is a common prophylactic intervention for the management of 2nd trimester pregnancy losses, although its application is not standard all over the world (1). The diagnosis of cervical insufficiency is notoriously difficult to make, and is largely retrospective based on history 1 (2). Cervical surveillance by use of transvaginal This was a descriptive prospective study based on ultrasonography has been recommended. The record files of 55 patients at DHQ hospital Mardan efficacy of cervical cerclage and its need has been from first July 2006 to 30 June 2011. Historical data discounted, an about previous pregnancies, the course of the unnecessary intervention in 50% of the cases. pregnancies, operation and delivery records, post However there is some evidence of positive role of operative care record and subsequent pregnancy cerclage in women at high risk with more than one record were all maintained. Approval was granted by second trimester losses (28-protocol). Strong risk the hospital ethics committee. Clinical indication for factor for preterm birth is a prior history of cervical cervical cerclage were divided into seven categories insufficiency, based on a history of repeated, in an effort to determine which historical feature painless midtrimester losses or preterm delivery. would predict the success rate of the procedure. Previous studies has indicated that ascending Patients with contraction and vaginal bleeding were infection from the vagina leads to preterm delivery considered to have premature labour rather than as well as cerebral palsy (4,5). In recent years the cervical insufficiency. These different indication importance of the cervical mucus plug as gatekeeper were; protecting the feto placental unit against ascending 1. History of single second trimester loss. infection from vagina has been demonstrated 2. History of >2 second trimester losses. (6,7,8). There is convincing data showing that 3. History of single second trimester loss with with Althusis (1) calling it increased intrauterine cytokine production in the prior cervical trauma. amniotic fluid contributes to the mechanism of 4. History of premature labour. cervical incompetence (9). Premature dilatation can 5. History of previous successful cerclage. be followed by infection but it can also be visa-versa. 6. Second trimester cervical dilatation without Measuring cervical length by ultrasound has been contractions. directly correlated with the duration of pregnancy 7. (10). The trans abdominal cerclage in cases of failed Second trimester cervical dilatation with contractions. previous transvaginal cerclages (11), and cervical Category 6 and 07 were called emergency cerclages occlusion in combination with cervical cerclage in while 1-5 were called elective cerclage. Differences order to retain the mucus plug has been proposed to in the fetal survival rate and complications were improve the take- home baby rate. The incidence of analysed. In all the patients McDonald procedure cervical between was performed with purse-string suture of No.2 silk. departments and countries. Part of this variation in General anaesthesia was used in all the patients. incidence rates is due to difficulties in diagnosis. Post operative bed rest for 24 to 72 hours was given insufficiency varies widely in emergency procedures while elective cerclage was Material and Method: done on day care basis with patients staying upto 12-18 hours at Hospital. Parentral antibiotics were 2 given in all the patients for first 24 hours. 06 patients i.e. 83% than it had been in the pregnancies prior to had history of previous cervical cerclages. In one cerclage in those women (25%). Fetal survival rate patient both the cerclage procedure failed due to after 13 emergency cerclages was not significantly badly damaged cervix in previous term pregnancy. greater than it had been in the pregnancies prior to 13 procedures were emergency cerclages. cerclage i.e,60%. The results and their significance remained un-changed when the first cerclage Results: The 55 patients had 222 pregnancies before treated pregnancy was analysed in each women. the cerclage was performed and the fetal survival When the cerclage procedures are categorized rate was 25%. In patient having elective cerclage the according to indications the improvement in fetal survival rate in 192 prior pregnancies was 20% pregnancy outcome is not significant in any category where as the previous fetal survival rate in 30 prior that includes cervical dilatation as the reason for the pregnancies of women with emergency cerclage was cerclage. The greatest increase in pregnancy 57%. The difference between these rates is outcome i.e. more than 6-fold increase occurs in the significant (p<.001) suggesting that two population operation performed for 2 or more second trimester were not similar. The population having emergency pregnancy losses. cerclage had better previous record of reproductive success but the fetal survival rate after 13 Post-op Morbidity emergency cerclage procedures was only 69% Estimated blood loss averaged 20ml in compared to 83% after 42 elective cerclages. The elective McDonald procedure. No Major post cerclage does not reduce the number of first operative complication occurred within two weeks trimester losses. These were omitted from the two of the 42 elective procedures. The risk of pregnancy population for the purpose of comparison with loss apparently cause by elective procedures was survival rate after cerclages. In patients having 1%. One of the elective cerclage suture was found elective cerclage the fetal survival rate in 150 prior displaced from pregnancies beyond twelve weeks was 27% where as procedure which was reapplied and pregnancy it was 60% in the 25 prior pregnancies beyond reached to term. One patient delivered one week twelve weeks in women with emergency cerclage. after the procedure. Among the 13 emergency When elective cerclage procedures were sub divided cerclages by gestational age at the time of operation, no charioamnionitis within one week postoperatively. significant differences in the fetal survival rate, The fetus didn’t survive. Among the entire series of premature delivery and small for gestational age 55 cases there were two cases of post op infants were found. There were no significant charioamnionitis forcing immediate suture removal differences in these parameters among the 13- and delivery (3.6%). In two cases membranes were women with emergency McDonald procedure. The bulging with cervical dilatation upto 2cm, in non of fetal survival rate was higher after elective cerclages these sac ruptured during surgery but both 3 there the cervix, two weeks after the was one case of acute developed PROM after surgery and delivered within section after cerclage. During the study time there 3 weeks of application of suture. At parturition one were 597 Cesarean-sections among the six thousand women had irregular cervical tear which needed deliveries. An overall rate of 9.95%. The McDonald repair. She had elective cervical cerclage. No cervical procedure might increase the cesarean section rate lacerations were reported in 13 of the emergency for obstetric indications only. Since maternal cervical cerclages. In the 6000 deliveries performed morbidity is five time greater after cesarean section at DHQ Mardan, 120 cervical lacerations at than after vaginal delivery, the cerclage procedures parturition required surgical repair or about 1 in thereby increase maternal morbidity and potential every 50 deliveries (2 %). After cerclage cervical mortality. Among 55 patients, in this study, only 6 laceration occurred 1 in 55 cases which is the same. patients (10.9%) needed cesarean section and that There was no case of bladder damage or Laparotomy too for obstetric reasons only. for repair or control of bleeding. Progestin’s: Cesarean Section: Additional No greater fetal cervical rate in 35 morbidity patients treated with progestin’s post operatively occurs in women with cerclage procedure because )80%) compared to 20 patients receiving no post op some physicians prefer to electively deliver by C- progestin (78%). Progestin’s: Tocolysis: No greater fetal cervical rate in 35 There was no significant difference patients treated with progestin’s post operatively in preterm birth rate before 35 weeks in 25 patients )80%) compared to 20 patients receiving no post op using tocolysis i.e. progestin (78%). (B-Mimetics) and 30 patients not using tocolysis, 18% vs 16%. Indication for cerclage No Term Preterm & SGA Total History of single second trimester loss History of >2 second trimester losses History of singe second trimester loss and prior cervical trauma History of premature labour History of prior successful 11 7 (64%) 1 (9%) 8 (73%) 8 /32 (25%) 12 8 (67%) 2 (17%) 10 (84%) 12/80 (15%) 6 2 (33%) 2 (33%) 4 (66%) 4/27 (15%) 7 6 5 (71%) 4 (67%) 1 (14%) 1 (16%) 6 (86%) 5 (83%) 10/29 (34%) 4/24 (17%) 4 Prior pregnancy fetal survival cerclage Second trimester cervical dilatation without contractions Second trimester dilatation with contractions Discussion: Establishing 5 (56%) 2 (22%) 7 (78%) 11/20 (55%) 4 1 (25%) 1 (25%) 2 (50%) 6/10(60%) of infection. Elective Transvaginal cerclages can be midtrimester loss actually caused by cervical safely performed as day case procedures (12). Most insufficiency accepted studies in the literature indicate a low major indications for cervical cerclage vary widely. There is complications rate (18) i.e,in less than 10% of no satisfactory objective test that can identify procedures (19) charioamnionitis is 2-3 times higher women with cervical weakness in the non pregnant in elective cerclages (20). The complication rate state (12). Most physician offer history indicated increase with increasing gestational age and cervical cerclage to women with three or more previous dilatation. PROM after elective cerclage occurs in 2% preterm births or second trimester losses. (13) and up to 58% in non elective procedures. Cervical Elective cerclage is either history indicated or dystocia and cervical trauma in labour have been ultrasound indicated while rescue cerclage is an reported in fewer than 5% of patients. Excessive emergency bleeding, maternal sepsis and fistula formation are is very procedure the 9 difficult. for diagnosis The premature cervical dilatation with exposed fetal membranes. 2-3 cm rare. cervical dilatation without effacement does not In a comprehensive review on cervical cerclage dictate imminent vaginal delivery (14,15). The Drakely (21) has noted an increase in cesarean substantial variation in fetal survival rate depends on delivery in cervical suture group, thought not the type of indication used for the operation, and statistically significant. This increased risk of the difference in population. Overall fetal survival cesarean section has probably due to Scar tissue rates before and after cerclage in this study are preventing cervical dilatation (22). Recent report comparable to those of the other large series. indicate that fetal rather than maternal indications (16,17,18). On analyzing the fetal survival rates, influence the rate of cesarean delivery (23,24). which vary considerably, the prognosis is worse in Some report in are in discordance with the general cases of emergency cerclage when cervical dilatation trend that cesarean section rate increase with has begun compared to elective procedure same is cerclage (25,26). in this study(69%vs83%). Patients undergoing rescue pregnancies are medicalised once a stitch is inserted, cerclage do benefit from at least 24-hours post hence increased anxiety to expedite delivery so operative period observation in hospital owing to many women may be treated unnecessarily due to the PP poor prediction and indications(21) .In this study ROM, early preterm delivery, miscarriage and cesarean section rate in the cerclage group was higher risk of 5 One of the postulates is than similar to the rest of the population 6. Hein M. The immunology of the cervical (10.9%vs9.95%).. mucus plug. PhD thesis faculty of Health To improve the accuracy of diagnosis and the sciences, University of Aarhus, 2002. pregnancy prognosis with the cerclage procedure 7. Hein M, Helmig RB, Schonheyder HC, Ganz prior exclusion of chorio amnionitis and fetal T, Uldbjerg N. An in vitro study of compromise, lethal fetal defects, fetal death, and antibacterial properties of the cervical PPROM is essential. It is essential to exclude genetic mucus plug. Am J Obstet Gynecol 2001; disorders, mullerian defects, thyroid disorders, and 185:586-92. collagen vascular disease before proceeding with a 8. Hein M, Valore EV, Helmig RB, Uldbjerg N, cerclage (27). There is absence of data to support Ganz T. Antimicrobial factors in the cervical routine genital tract screening for infections before mucus cerclage insertion (12). 2002;187:137-44. 9. plug. Am J Obstet Gynecol Lee KY, Jun HA, Kum HB, Kang SW. References: Interleukin-6, but not relaxin, predicts 1. Althuisius SM, Dekker GA, Controversies outcome of rescue cerclage in women with regarding cervical incompetence, short cervical incompetence. Am J Obstet Gynecol cervix, and the need, and the need for 2004;191:784-9. cerclage. Clinics in Perinatology, 2004; 2. 3. 31(4)695-720. Nicolaides KH. Cervical length at 23 weeks Simcox R, Shenanan A, Cervical Cerclage in of gestation: prediction of spontaneous the Gynae 2007; 21(5); 831-42. preterm ACOG Practice insufficiency. 4. 10. Heath VC, Southall TR, Souka AP, Elisseou A, Int Bulletin. J Gynaecol Cervical Ultrasound Obstet Gynecol 1998;12:312-17. Obstet 11. Zaveri V, Aghajafari F, Amankwah K, Hannah 2004;85:81-9. M. Abdominal Versus vaginal cerclage after Petrous S, Mehta Z, Hockley C, Cook- a failed transvaginal cerclage: a systematic Mozaffari P,Henderson J, Goldacre M. The review. Am J Obstet Gynecol 2002;187:868- impact of preterm birth on hospital 72. inpatient admissions and costs during the 5. delivery. 12. Royal college of Obstetricians and first 5 years of life. Pediatrics 2003;112(6pt Gynaecologists.Cervical Cerclage.Green-top 1):1290-7 Guideline Jacobsson B, Hagberg G, Hagberg B, Ladfors at:www.rcog.org.uk/files/rcog- L, Niklasson A. Cerebral palsy in preterm corp/uploaded-files. infants: a population-based case study of No.60 May2011.Available 13. Delboy A, et al. Multicenter randomized antenatal and intrapartal risk factors. Acta trial Paediatr 2002;91.946-51. prevention 6 of cerclage in for high-risk preterm birth women with shortened midtrimester cervical length. Am Obst.Gynecol: Dec 15. 1981; 141(8):1065-71 J Obstet Gynecol 2009;201:375.el-8. (Medline). 21. Drakeley AJ, Roberts D, Alfirevic Z.Cervical 14. Final report of the Medical Research stitch (cerclage) for preventing pregnancy Council/Royal College of Obstetricians and loss in women. Cochrane Database Syst Gynaecologists Rey. 2003;(1):CD003253. trial of multicentre cervical randomized cerclage. MRC/RCOG 22. Abdelhak YE, Aronov R, Roque H, Young BK. Working party on Cervical Cerclage Br J Management Obstet Gynaecol 1993:100:516-23. term:remove the suture in labor? J Perinat 15. To MS, Skentou C, Liao AW, Cacho A, Nicolaides KH. Cervical Length of cervical cerclage at Med. 2000;28(6):453-7. and 23. Fox NS>Rebarber A, Bender S, Saltzman DH. funneling at 23 weeks of gestation in the Labor outcomes after Shirodkar cerclage. J prediction of spontaneous early preterm Reported Med. 2009 jun;54(6):361-5. delivery. Ultrasound Obstet Gynecol 2001; 24. Schwartz RP, Chatwani A, Sullivan P.Cervical 18:200-3. cerclage. A review of 74 cases. J Report 16. To MS, Palaniappan V, Skentou C, Gibb D, Nicolaides KH. Elective Med. 1984;29(2):103-6. cerclage 25. Shamshad, Mustajab Y. Jehanzaib M. vs.ultrasound-indicated cerclage in high-risk Evaluation pregnancies. Ultrasound Obstet Gynecol sonographically incompetent cervix in at 2002;19:475-7. high risk patients. J Ayub Med Coll 17. Berghella V, Odibo AO, To MS, Rust OA. of trials 2009;8(3):234-237. 27. Glass RH, Golbus MS: Habitual abortion. 18. Owen J, Hankins G, Lams JD, Berghella V, Fertil Steril 29:257,1978. Sheffield JS, Perez- Herger JH. Comparison of success and morbidity in cervical cerclage procedures. Obstet Gynecol 1980;56:543-8. Cerclage and Cervical insufficiency: an evidence-based analysis. Obstet Gynecol. Dec 2002;100(6):131327(Medline). 20. Charles D, Edwards for cerclage in cervical incompetence. JLUMHS Gynecol 2005;106:181-9. JH. cerclage 26. Memon S, Shaikh F, Pushpa. Role of cervical using individual patient-level data. Obstet 19. Herger cervical Abbottabad 2008;20:31-4. Althuisius SM.Cerlage for short cervix on ultrasonography;meta-analysis of WR, Infectious complications of cervical cerclage. Am J 7