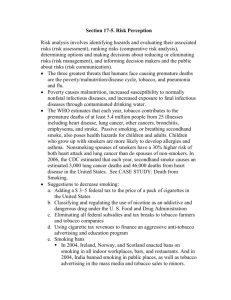
Quit Victoria and Cancer Council Victoria Submission: Draft for
advertisement

Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 – 2018 25th June 2012 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Contents Introduction ................................................................................................................................ 3 Part One – Overarching Issues ................................................................................................... 3 Part Two – Response to Part 6: Priority Areas and Actions ...................................................... 8 6.1 Strengthen social marketing campaigns to motivate smokers to quit; discourage uptake of smoking; and reshape social norms about smoking ........................................................... 8 6.2 Continue to reduce the affordability of tobacco products .............................................. 15 6.3 Bolster and build on existing programs and partnerships to reduce smoking rates among Aboriginal and Torres Strait Islander (ATSI) people........................................................... 23 6.4 Strengthen efforts to reduce smoking among people in disadvantaged populations with high smoking prevalence ...................................................................................................... 32 6.5 Eliminate remaining advertising, promotion and sponsorship of tobacco products ...... 37 6.6 Consider further regulation of the contents, product disclosure and supply of tobacco products and non-therapeutic nicotine delivery systems...................................................... 46 6.7 Reduce exceptions to smokefree workplaces, public places and other settings............. 52 6.8 Provide access to a range of evidence based cessation services to support smokers to quit........................................................................................................................................ 63 Part Three – Monitoring Progress ............................................................................................ 70 2 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Introduction Cancer Council Victoria and Quit Victoria welcome the opportunity to comment on the Draft National Tobacco Strategy 2012-2018. We believe the document represents a comprehensive evidence based approach to tobacco control that will guide the work necessary to be undertaken by government and non-government organisations if Australia is to reach its target of reducing adult smoking rates to 10 per cent or less and halving the Indigenous smoking rate by 2018. Part 1 of our submission outlines overarching issues that apply to the strategy as a whole. This includes areas which we believe either need to be elevated in the final version of the National Tobacco Strategy (the Strategy) or issues which, while they may not be documented in the Strategy, should be considered when adopting and implementing the Strategy. Part 2 are our comments on the eight priority areas outlined in the draft Strategy and the activities under each of these areas. Included in this section are references, some of which are more recent than those cited in the draft Strategy. Part 3 includes our comments on monitoring progress. Part One – Overarching Issues a. Greater recognition of Australia’s obligations under the World Health Organisation Framework Convention on Tobacco Control (WHO FCTC) The WHO FCTC is the first treaty negotiated under the auspices of the World Health Organization and is one of the most widely embraced treaties in UN history. The WHO FCTC is an evidence-based treaty that was developed in response to the globalisation of the tobacco epidemic. Its stated objective is to ‘protect present and future generations from the devastating health, social, environmental and economic consequences of tobacco consumption and exposure to tobacco smoke by providing a framework for tobacco control measures to be implemented by the Parties at the national, regional and international levels in order to reduce continually and substantially the prevalence of tobacco use and exposure to tobacco smoke.’ 3 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Australia signed the WHO FCTC on 5 December 2003, and became a full Party on 27 February 2005, the date on which it came into force. Australia is legally bound to perform, in good faith all of its obligations under the treaty including demand reduction provisions contained in articles 6-14, and supply reduction provisions contained in articles 15-17. We do not believe that the significance of the FCTC or the importance of Australia’s obligations under the FCTC is sufficiently addressed in the current draft of the Strategy. Cancer Council Victoria and Quit Victoria suggest that an additional Objective be added to the Strategy which reads: “to give effect to obligations that Australia has as a party to the WHO Framework Convention on Tobacco Control” We note that the last paragraph on page 14 of the draft Strategy does not provide a full list of policies as outlined in the FCTC and if this section of the draft is to remain in the final Strategy it should be changed along the lines of the first two paragraphs above. The introduction to the Priority Areas (5.4) in the draft Strategy should also highlight that the comprehensive approach to tobacco control taken in the Strategy is also consistent with the requirements of the WHO FCTC. Lastly it is unclear whether Part Four ‘Progress and Future Challenges’ will remain in the final Strategy. If so, then Australia’s important role in negotiation of the FCTC and its ratification in 2005 should be included as significant achievements during the period of the last strategy 2004-2009. b. Protecting the National Tobacco Strategy 2012–8 from tobacco industry interference in public health measures Article 5.3 of the WHO FCTC requires Parties to act to protect their tobacco control policies from commercial and other vested interests of the tobacco industry. In the draft Strategy there is simply a description of Article 5.3 on page 21 under section 5.7 with no comment on how the Strategy will address Australia’s obligations in relation to Article 5.3. The only other place Article 5.3 is mentioned is under Priority 6.5, action 6.5.10. Given that Article 5.3 applies to all tobacco control policies, we do not believe that the 4 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 specific priority area regarding advertising, promotion and sponsorship is an appropriate place for actions under Article 5.3 to be located. We believe that a description of Australia’s obligations under Article 5.3 and an explanation that these obligations apply to all tobacco control policies, and all levels of government, should form part of overarching principles of the Strategy (along with things such as working in partnership). In addition, reference should be made to the Guidelines for Article 5.3 that were adopted by the WHO FCTC Conference of the Parties and actions and responsibilities should be identified based on these guidelines. For example Principle 1 of the guidelines recognises that ‘there is a fundamental and irreconcilable conflict between the tobacco industry’s interests and public health policy interests’. Principle 2 of the guidelines recognises that ‘parties, when dealing with the tobacco industry or those working to further its interests, should be accountable and transparent’. If the current reference to Article 5.3 is to remain under the heading ‘The Framework’ then this would be the appropriate place for further detail on this issue to be contained in the Strategy. c. Countering illicit trade claims made by the tobacco industry Cancer Council Victoria and Quit Victoria are concerned about studies commissioned by the tobacco industry that report highly misleading and inflated levels of illicit trade activity in tobacco in Australia and have undertaken critiques of these reports which can be found at: Cancer Council Victoria website . The tobacco industry claims that increasing tobacco excise has already increased the use of illicit tobacco in Australia and measures such as the introduction of plain packaging of tobacco products will further increase this use. In sharp contrast to the claims made by the tobacco industry of 13.4% of the tobacco market in Australia being illicit tobacco, a more realistic estimate of the total use of illicit tobacco products in Australia based on analysis of figures from the National Drug Strategy Household Survey 2010 would be more like 2 to 3% of the total market. We believe that the tobacco industry, both in Australia and internationally, is attempting to use the spectre of illicit trade to discourage governments from introducing proven tobacco control measures, to divert attention and resources away from proven tobacco control measures into costly anti-illicit trade activity and to re-position itself as ‘legitimate’ and ‘responsible’ . 5 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 We are concerned by claims from the tobacco industry that the Australian Government should be doing more to detect counterfeit tobacco products. Counterfeiting is an intellectual property issue (trade mark protection) that is primarily the responsibility of trade mark owners, in this case the tobacco industry. Government tobacco control resources should not be used in protection of the tobacco industry’s intellectual property. d. Securing funding for the Strategy from all levels of government While many of the activities outlined in the draft Strategy are low cost to implement, others require allocation of funding to make implementation possible. Cancer Council Victoria and Quit Victoria believe it is essential that both the Australian government and State and Territory governments commit to providing funding for implementation of the strategy. Some activities will require federal funding, some will require state and territory funding and others will require both levels of government to commit funding in order to achieve the Strategy’s aims. For example it is very important that State governments continue to provide social marketing support to complement Commonwealth Government commitments to social marketing in the area of tobacco control. Without this support there is a danger the optimal levels of exposure to anti-smoking campaign messages amongst the public will not be achieved. The National Partnership Agreement for Closing the Gap and other funding initiatives by both Commonwealth and State and Territory governments has represented a significant level of investment towards activity in reducing smoking rates among Aboriginal and Torres Strait Islander people. This funding has enabled a significant amount of work to be started such as supporting the development of Aboriginal health workforce, tailoring and promotion of mainstream cessation services to Aboriginal and Torres Strait Islander people to reduce smoking disparities and federally funded dedicated mass media advertising campaigns. However this funding currently expires in 2013 and this work cannot be continued or further developed without further Commonwealth, State and Territory government funding. Cancer Council Victoria is pleased to see that the free on-line resource Tobacco In Australia: Facts and Issues has been acknowledged as a comprehensive and up to date resource on tobacco control evidence and policies. 6 The website is incredibly well accessed and used Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 (nearly 80,000 hits between January and May 2012), indicating it is invaluable in assisting all those working in tobacco control (policy makers, researchers, academics, health professionals, media). Funding for updating of this resource has now expired and we strongly urge an appropriate level of funding be allocated to ensure this resource remains up to date and its accuracy and utility maintained. e. The importance of existing and new partnerships Cancer Council Victoria and Quit Victoria are pleased to see the important role of partnerships in achieving past successes in Australia acknowledged and a commitment to continuing existing and building new partnerships emphasised in the draft Strategy. A comprehensive Strategy such as that proposed can only be successfully implemented with all levels of government, non-government organisations and increasingly the health and community sector working together. Each of these groups have different jurisdictional responsibilities, skills, expertise and differing capacity to impact on populations identified in the Strategy. 7 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Part Two – Response to Part 6: Priority Areas and Actions 6.1 Strengthen social marketing campaigns to motivate smokers to quit; discourage uptake of smoking; and reshape social norms about smoking Quit Victoria recommends that the Strategy determine a clear definition of the term “social marketing” which Quit Victoria considers to refer to mass media advertising campaigns delivered through broadcast television, radio and digital media; print and press media, and outdoor and transit media mediums. Within this range of advertising vehicles, Quit Victoria recommends that television campaigns targeted to smokers aged 18-49 years in low socio economic and blue collar occupations be prioritised within the National Tobacco Strategy over other advertising mediums. Anti-smoking television campaigns remain one of three main interventions (with tobacco taxation and legislative reform) to reduce population smoking rates both in Australia and internationally. In order to be effective an anti-smoking social marketing program should take a whole - of population approach where campaigns are created and run to appeal to the widest possible group of smokers to ensure maximum return on investment. A general-audience strategy where campaigns are produced to convey key messages likely to resonate with all, but not specific to any, population groups provides significantly more value than tailoring advertising message, settings and talent to multiple specific population subgroups. The latter strategy would not be cost-effective, as it requires funding multiple campaigns to convey a variety of tailored messages or tailored versions of one message A recent review summarised the impact of mass media campaigns on promoting quitting among adult smokers overall and for subgroups, the influence of campaign intensity and different channels; the effects of different message types. The review1 concluded that mass media campaigns to promote quitting are important investments as part of comprehensive tobacco control programmes to educate the broader public on the harms of smoking, set the agenda for discussion, change smoking attitudes and beliefs, increase quitting intentions and quit attempts, and reduce adult smoking prevalence. 8 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Jurisdictions should aim for high reach and consistent exposure over time with preference towards negative health effects messages. It is very important that State governments continue to support social marketing to complement Commonwealth Government commitments to social marketing in the area of tobacco control. Without this support there is a danger the optimal levels of exposure to antismoking campaign messages amongst the public will not be achieved. Actions 6.1.1 Run effective mass media campaigns at levels of reach and frequency demonstrated to reduce smoking. Responsibility: Australian Government, State and Territory governments (as applicable), non-government organisations. Recent research has also reinforced the need for repeated cycles of advertising to produce continuous, sustained exposure to anti-smoking messages. A study of Australian smokers found that although anti-smoking media campaigns increase the proportion of smokers who make a quit attempt (both for those who had an interest in quitting in the previous year and those who did not), this impact does not last beyond a few months following the conclusion of the campaign. 2 This highlights the need for sustained and consistent television campaign exposure if we are to continue to motivate smokers to prioritise making a quit attempt now. It also raises considerable concerns over potential negative effects of any prolonged period of being ‘offair.’ 6.1.2 Continue mass media campaigns targeted to Aboriginal and Torres Strait Islander people including robust evaluation to inform future campaign strategies. Responsibility: Australian Government, State and Territory governments, nongovernment organisations. Please see comments made in relation 6.3.10 6.1.3 Continue to monitor the appropriateness and effectiveness of recommended media weights and mediums/channels. 9 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Responsibility: Australian Government, State and Territory governments; nongovernment organisations. A review of mass media campaigns internationally recently completed by the Centre for Behavioural Research in Cancer (CBRC) at the Cancer Council Victoria and published in the British Medical Journal’s Tobacco Control has concluded that a mean of 2,560 Gross Rating Points (GRPs) per quarter (850/mth) was significantly associated with quitting and could be expected to reap proportionally larger returns than 4,800 GRPs per year (400/mth) and that higher levels of exposure could be required to influence adult rather than youth smoking since adults are more hampered by addiction. 3 Quit Victoria has recently sought advice from its media buying agency, Mitchell and Partners and the CBRC on how Quit’s target audience (low socio-economic smokers, 18-49 years) consume media but also respond to anti-smoking messages. Information received from both sources confirms television remains the most effective medium to both reach the most smokers and provide an avenue to deliver impactful antismoking message most directly. There is substantial evidence that TV campaigns contribute to increased numbers of quit attempts and decreased smoking prevalence. 6.1.4 Continue to implement national tobacco campaigns and state and territory campaigns, including a balance of existing material with proven effectiveness and a suite of new materials. Responsibility: Australian Government, State and Territory governments; nongovernment organisations Cancer Council Victoria and Quit Victoria support the action with the inclusion of nongovernment organisations within responsibility. Quit Victoria has worked collaboratively with the Department of Health and Ageing and Australian National Preventive Health Agency to ensure that scheduling of Victorian funded media campaigns complement the Commonwealth campaigns in both TARP levels of exposure and message content. 10 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Quit Victoria remains in regular contact both Commonwealth and State government departments and agencies to ensure the messages communicated in social marketing campaigns are supportive of overarching strategies to reduce smoking rates. Quit Victoria is also in regular contact with other jurisdictions creating new anti-smoking social marketing campaigns to avoid duplication of, and create access to, new creative messages. This ensures all organisations conducting anti-smoking campaigns are working together to result in a broader variety of anti-smoking messages are reaching the public. The choice of creative executions for Quit Victoria’s advertising program is a mix of graphic health effects, emotional campaigns and more recently positive campaigns, either produced in Victoria or sourced from other Australian and/or international jurisdictions. Annual advertising plans include new creative executions and regular rotation of older messages to avoid wear out and fatigue of the anti-smoking message. 6.1.5 Enhance collaborative action between the Australian Government, State and Territory governments and non-government organisations to maximise the effectiveness of mass media campaigns. Responsibility: Australian Government, State and Territory governments and nongovernment organisations. In order to maximise the effectiveness of mass media campaigns it is essential that Australian Government, State and Territory governments and non-government organisations work together to ensure smokers are exposed to a roster of sustained anti-smoking television campaigns at requisite exposure levels to drive a reduction in smoking rates and an increase in quitting behaviour. There is a risk of substantially reduced exposure to anti-smoking television campaigns in Victoria due to the non-continuation of tobacco social marketing funding by the Victorian government for the next four years. In the period 2008-2012, state funded campaigns have achieved an average 400 TARPS per month over 34 weeks. From July 2012, this will be reduced to an average 200 TARPS per month over 17 weeks. 11 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 6.1.6 Complement the implementation of tobacco control policies (e.g. new health warnings on packs and plain packaging) with mass media campaigns to enhance cessation efforts by smokers. Responsibility: Australian Government, State and Territory governments, nongovernment organisations. In Australia the introduction of pictorial health warnings on cigarette packets was supported by a televised media campaign highlighting illnesses featured in two of the warning labelsgangrene and mouth cancer. Research into the effectiveness of this strategy concluded that television advertisements and pictorial health warnings on cigarette packets may operate in a complementary manner to positively influence awareness of the health consequences of smoking and motivation to quit.4 Cancer Council Victoria and Quit Victoria believes the implementation of tobacco control policies, including revised pictorial warnings would benefit from supportive mass media campaigns to increase the depth, meaning and personal relevance of the warnings. 6.1.7 Continue to build the evidence base on effectiveness of mass media to inform and refine future campaign development. Responsibility: Australian Government, State and Territory governments, nongovernment organisations. Cancer Council Victoria and Quit Victoria strongly agree that the Australian Government, State and Territory governments, non-government organisations should work together to continue to build the evidence base on the effectiveness of mass media as a tool to reduce smoking rates and refine future campaign development. Quit Victoria benefits from the social marketing research expertise of the Centre for Behavioural Research in Cancer (CBRC) at the Cancer Council Victoria, whose work not only influences campaign development but also provides effective direction on optimal media weights to achieve the biggest impact on smoking behaviour. As part of the Cancer Council Victoria, Quit Victoria is continuously evaluating efficacy of 12 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 social marketing campaigns and analysing the resonance of individual creative executions to ensure communications objectives are being met, and the best possible combination of campaigns is being employed to reach smokers and motivate them to quit. Quit Victoria measures the effectiveness of social marketing campaigns by a range of methods, including; Newly created Victorian Tobacco Social Marketing Monthly Tracking survey will assess recall of the ad, emotional, cognitive, and behavioural impact of the campaign and the efficiency of Quit’s media buying strategies; Social research focus groups which are conducted for every new campaign developed. These take the form of exploratory research groups at the start of the campaign development process and concept testing groups prior to production. Further groups may also be held post production to clarify and validate any remaining questions. These groups are an essential component of the campaign development process. Smoker contacts with support services and information including Quitline, Quit Coach, quit.org.au and social media sites. 6.1.8 Continue to share campaigns as well as evidence on effective mass media campaigns with the global tobacco control community. Responsibility: Australian Government, research organisations; State and Territory governments, non-government organisations. Agree Quit Victoria has a long history of sharing campaigns and evidence with the global tobacco control community and will continue to do so. For more information on how we measure the effectiveness of our social marketing program please see response to 6.1.7 1 Durkin S, Brennan E and Wakefield M. Mass media campaigns to promote smoking cessation among adults: an integrative review. Tobacco Control 2012;21(2):12738. Available from: Tobacco Control website 2 Wakefield M, Spittal M, Yong H-H, Durkin S and Borland R. Effects of mass media campaign exposure intensity and durability on quit attempts in a population-based cohort 13 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 study. Health Education Research 2011;36(6):98897. Available from: Oxford Journals website 3 Durkin S, Brennan E and Wakefield M. Mass media campaigns to promote smoking cessation among adults: an integrative review. Tobacco Control 2012;21(2):12738. Available from: Tobacco Control website 4 Brennan E, Durkin S, Cotter T, Harper T and Wakefield M. Mass media campaigns designed to support new pictorial health warnings on cigarette packets: evidence of a complementary relationship. Tobacco Control 2011;20(6):4128. Available from: National Center for Biotechnology Information website 14 6.2 Continue to reduce the affordability of tobacco products As stated in the draft strategy ‘There is strong evidence of the influence of price on the prevalence of tobacco smoking.1 Price increases encourage existing smokers to quit and raise the barrier for people considering taking up smoking, especially young people. 2 The greater the increase in price, the greater the fall in demand.3 Actions 6.2.1 Analyse the impact of the 2010 tobacco excise increases, including the impact on young people and smokers from low socioeconomic groups. Responsibility: Australian Government; research organisations; non-government organisations. In addition to the study cited in the consultation paper, the Centre for Behavioural Research in Cancer at the Cancer Council Victoria has undertaken two studies of the impact of the April 2010 tobacco excise increases. The first study was a cohort study which examined quitting and changes in the prevalence of tobacco use, consumption, and price minimising behaviours between November and December 2009 and July and August 2010.4 The second study presents data relating to smokers’ predicted and actual responses tobacco price increases using data from 2009 (pre price increase) and 2010 (post price increase). 5 Findings from both reports indicate that the 2010 excise increases was a success and a highly effective measure to reduce smoking. In the cohort study, 15.1% of smokers had quit smoking at follow up, some of these prior to the price increase but one-third to one-half as a direct result of the price increase. In addition, almost a quarter of respondents (23.8%) had tried to quit smoking and 35.8% reported that they had cut down consumption in response to the tax increase. Young people and those from low socioeconomic groups were as likely as others to have quit or cut down consumption. The second study investigated continuing smokers only and doesn’t include those that did successfully quit between 2009 and 2010. Of continuing smokers, 28% indicated that they had made a quit attempt following the price increase and 34% indicated smoking fewer cigarettes. In this study younger smokers were significantly more likely than older smokers to report that they had tried to quit. There was also a trend towards low SES smokers being more likely to report they had tried to quit when compared to high SES smokers. Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 In addition the 2010 price increase did not appear to have negatively impacted on continuing smokers’ ability to pay for essentials such as food with no change in the proportion of smokers who reported this problem between 2009 and 2010. 6.2.2 Continue to implement regular staged increases in tobacco excise as appropriate, to reduce demand for tobacco. Responsibility: Australian Government. Increasing the price of tobacco products is the most reliable way that governments can accelerate declines in smoking: indeed based on historical trends, without a further increase in excise/customs duty of a similar magnitude to the April 2010 increase, it is unlikely that such targets can be achieved.6 There is little evidence internationally about whether a number of smaller increases in price have the same or a greater impact than a single increase of the same magnitude, but it is psychologically and economically plausible that each price ‘shock’ would provide smokers with another prompt to quit. It seems that regular increases in excise/customs duty in line with the previous six-months CPI have prevented tobacco products from becoming more affordable, but may not have been sufficiently large to prompt quitting among smokers additional to the background level of cessation occurring across the population across time.7 Health groups would be pleased to see moderate increases in duty at least once each year over the first few years of this strategy. These might be combined with one of the indexation increases for greater (combined) impact. The impact of these increases on consumption and quitting could usefully be compared to that of the April 2010 increase to help guide future tax policy on tobacco products. 6.2.3 Complement tobacco excise increases with additional supports for low income smokers to quit. Responsibility: State and Territory governments, Australian Government, non-government organisations, social service organisations. 6.2.4 Encourage low income smokers to access subsidised medications to assist them to quit. Responsibility: Australian Government, State and Territory governments, non-government organisations, social service organisations. 16 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 We believe that Action items 6.2.3 and 6.2.4 are more appropriately and already adequately addressed under action items for Priority 6.8 Provide access to a range of evidence based cessation services to support smokers to quit. 6.2.5 Identify practices that may be undermining the effectiveness of the tobacco excise increases in reducing smoking prevalence (e.g. price discounting) and develop strategies to minimise these practices. Responsibility: Australian Government; State and Territory governments and non-government organisations. Overseas studies examining industry and consumer responses 8 9 10 have found that the availability of tobacco products from cheaper sources reduced the percentages of smokers quitting and cutting down in response to tax-related price increases but in no case studied completely undermined the effectiveness of tax increases.. Assessment of the impact of increases in excise/customs duty in Australia in 1999–200111 12 and in April 201013 similarly detected increases in price-minimising behaviours by smokers such as purchasing in bulk, switching to RYO,[10] shifting to purchase from convenience to discount outlets, looking out for ‘specials’ and switching to cheaper brands. However these were less common that smoking-related changes such as attempting to quit or cut down.14 The company marketing practices that reduce the effectiveness of tax increases in reducing the use of tobacco products include: providing stock at lower costs to supermarkets, tobacconists and other discount outlets (discounting)15 manufacturing RYO under the same name as well known cigarette brands (facilitating shifts to cheaper product types)16 (In 2001, RYO brands included Marlboro and Winfield.17 In 2012 they also include Choice, Davidoff, Escort, Holiday, Horizon, Longbeach and Peter Stuyvesant18 ... i.e. many of the most popular cigarette brands in Australia.19 providing stock at lower prices for short periods (‘specialling’)20 packaging in large pack sizes which are cheaper per stick21 22 packaging in smaller pack sizes to reduce the up-front purchase costs. packaging small packs in multi-packs which are cheaper per stick than single packs but require less of an outlay than cartons. 17 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Prices boards at retail outlets (still allowed in most jurisdictions in Australia) and on-line catalogues published by supermarkets and other retailers allow companies to promote products on the basis of price relative to that of other brands. Governments should assess whether the effects of price-related marketing could be minimised through amendments to national and state legislation. 6.2.6 Continue to participate in negotiations to finalise the Protocol to Eliminate the Illicit Trade in Tobacco Products under the WHO FCTC. Responsibility: Australian Government. 6.2.8 Continue enforcement efforts to prevent the illegal importation and illegal supply and cultivation of tobacco. and enhance technology and support systems to identify and respond to illicit trade in tobacco. 6.2.9 Continue to monitor the supply and use of illicit tobacco in Australia and effective approaches to reduce the illicit trade in tobacco. Responsibility: Australian Government; non-government organisations. The Australian Government showed leadership during the final negotiating session of the Draft FCTC Protocol to Eliminate the Illicit Trade in Tobacco Products in Geneva in March – April 2012. The Draft Protocol will be presented to the Conference of the Parties in November 2012 for adoption by Parties. Cancer Council Victoria and Quit Victoria are concerned about studies commissioned by the tobacco industry that report highly misleading and inflated levels of illicit trade in tobacco in Australia and has undertaken critiques of these reports which can be found at: Cancer Council Victoria website . The tobacco industry claims that increasing tobacco excise has already increased the use of illicit tobacco in Australia and measures such as the introduction of plain packaging of tobacco products will further increase this use.23 In sharp contrast to the claims made by the tobacco industry of 13.4% of the tobacco market in Australia being illicit tobacco24, a more realistic estimate of the total use of illicit tobacco products in Australia 18 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 based on analysis of figures from the National Drug Strategy Household Survey 2010 would be more like 2 to 3% of the total market.25 We also support the Australian Government’s work to date in monitoring illicit trade in tobacco in Australia and implementing prevention and law enforcement measures, and believe it is important this work continues. However given the very low levels of use of illicit tobacco by Australian smokers we do not believe there is evidence that existing technology and support systems are inadequate and need enhancement. Specifically we do not support health funding for tobacco control measures being diverted to increase funding for illicit trade monitoring and enforcement. In addition we are concerned by claims from the tobacco industry that the Australian Government should be doing more to detect counterfeit tobacco products. Counterfeiting is an intellectual property issue that is primarily the responsibility of the trade mark owners, in this case the tobacco industry. Government tobacco control resources should not be used in protection of the tobacco industry’s intellectual property. Tobacco control resources allocated to illicit trade should be concerned only with public health – through the effect of the evasion of taxes and duties on tobacco use. 6.2.7 Support and participate in the development of Guidelines for Implementation of Article 6 of the WHO FCTC. Responsibility: Australian Government; The Australian Government provided $400,000 to support the development of guidelines under Article 6 of the FCTC and we applaud this extra-budgetary contribution. The draft Article 6 Guidelines will be presented to the Conference of the Parties in November 2012 for adoption. Cancer Council Victoria and Quit Victoria encourages the Australian Government to continue to play a leading role in the development and finalization of the guidelines to ensure that the guidelines adopted by the COP contain recommendations for effective tobacco tax policy that are globally useful. 19 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 6.2.10 Keep under review the possibility of reducing duty-free sales of tobacco, subject to consideration of international obligations. Responsibility: Australian Government. As part of the 2012-2013 budget measures the Australian Government announced that it would decrease the duty-free tobacco allowance for in-bound travellers. At present travellers can bring into Australia 250 cigarettes or 250 grams of cigars or tobacco products tax free. From 1 September 2012, this will be reduced to 50 cigarettes or 50 grams of cigars or tobacco products.26 We support this measure and would also encourage the Australian Government to completely remove the duty free allowance for tobacco products in the near future. We recognise that this may require negotiations with other countries in relation to international obligations and would encourage the Australian Government to play a lead role in amending these obligations. Removing international obligations for duty-free allowances for tobacco products would be beneficial for all countries wanting to implement comprehensive tobacco control programs and assist parties to the FCTC in compliance with obligations under Article 6. 1 Commonwealth of Australia Taking Preventative Action- A response to Australia: the Healthiest country by 2020 - the report of the National Preventative Health Taskforce 2 Commonwealth of Australia Taking Preventative Action- A response to Australia: the Healthiest country by 2020 - the report of the National Preventative Health Taskforce 3 International Agency for Research on Cancer. Chapter 4. Tax, price and aggregate demand for tobacco products. Effectiveness of tax and price policies for tobacco control. Lyon, France: IARC, 2011. Available from: International Agency for Research on Cancer website 4 Scollo M, Zacher M, Warne C, Hayes L, Durkin S and Wakefield M. Impact in Victoria of the April 2010 25% increase in excise on tobacco products in Australia. Short-term effects on prevalence, reported quitting and, reported consumption, real cost, and price-minimising strategies in Victoria. Melbourne, Australia: Centre for Behavioural Research in Cancer, The Cancer Council Victoria, April 2012 5 Hayes L. Smoker's responses to the 2010 increase to tobacco excise: Findings from the 2009 and 2010 Victorian Smoking and Health Surveys. CBRC Topline Research Report. Melbourne, Australia: Centre for Behavioural Research in Cancer, The Cancer Council Victoria. Prepared for Quit Victoria, November 2011. 6 Hurley S, Spittal M, Scollo M, Durkin S and Wakefield M. Predicted impact of proposed tobacco control strategies. Melbourne, Australia: Cancer Council Victoria, 2009. Available from: Department of Health and Ageing website 7 Scollo M. Chapter 2. Trends in tobacco consumption. In: Scollo, M, and Winstanley, M, ed. Tobacco in Australia: facts and issues. Melbourne, Australia: Cancer Council Victoria, 2012 In press. Available from: Tobacco in Australia website 20 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 8 White V, Gilpin E, White M and Pierce J. How do smokers control their cigarette expenditures? Nicotine & Tobacco Research 2005;7(4):625–35. Available from: Taylor and Francis website 9 Hyland A, Laux FL, Higbee C, Hastings G, Ross H, Chaloupka FJ, et al. Cigarette purchase patterns in four countries and the relationship with cessation: findings from the International Tobacco Control (ITC) Four Country Survey. Tobacco Control 2006;15(suppl. 3):iii59–64. Available from: Tobacco Control website 10 Ross H, Blecher E, Yan L and Hyland A. Do cigarette prices motivate smokers to quit? New evidence from the ITC survey. Addiction 2011;106(3):609–19. Available from: Wiley Online Library website 11 Scollo M, Owen T and Boulter J. Price discounting of cigarettes during the National Tobacco Campaign. In: Hassard, K, ed. Australia's National Tobacco Campaign: evaluation report vol. 2. Canberra: Commonwealth Department of Health and Aged Care, 2000. 155-200. Available from: http://www.quitnow.gov.au/internet/quitnow/publishing.nsf/Content/national-tobacco-campaign-lp (This website link was valid at the time of submission) 12 Scollo M, Younie S, Wakefield M, Freeman J and Icasiano F. Impact of tobacco tax reforms on tobacco prices and tobacco use in Australia. Tobacco Control 2003;12(suppl. 2):ii59–66. Available from: Tobacco Control website 13 Scollo M, Zacher M, Warne C, Hayes L, Durkin S and Wakefield M. Impact in Victoria of the April 2010 25% increase in excise on tobacco products in Australia. Short-term effects on prevalence, reported quitting and, reported consumption, real cost, and price-minimising strategies. Melbourne, Australia: Centre for Behavioural Research in Cancer, Cancer Council Victoria, 2012. 14 Scollo M, Zacher M, Warne C, Hayes L, Durkin S and Wakefield M. Impact in Victoria of the April 2010 25% increase in excise on tobacco products in Australia. Short-term effects on prevalence, reported quitting and, reported consumption, real cost, and price-minimising strategies. Melbourne, Australia: Centre for Behavioural Research in Cancer, Cancer Council Victoria, 2012. 15 Prices Surveillance Authority. Report no. 52: inquiry into cigarettes declaration. Matter no: PI/94/1. Melbourne, Australia: PSA, 1994. 16 Convenience & Impulse Retailing. RYO & cigar sales continue to defy the odds. Balmain, New South Wales: Berg Bennett, 2010 [viewed 15 July 2011]. Available from: http://www.cstore.com.au/magazine/article.php?id=544(This website link was valid at the time of submission) 17 NSW Retail Tobacco Traders' Association. Price lists--cigarettes. The Australian Retail Tobacconist 2001;61(no. 8 Aug-Sep):14-16. 18 NSW Retail Tobacco Traders' Association. Price listscigarettes. The Australian Retail Tobacconist 2012;84(no. 5 FebApr):12. 19 Annual report, Market sizes & shares Retail World 2011;64:50. 20 Prices Surveillance Authority. Report no. 52: inquiry into cigarettes declaration. Matter no: PI/94/1. Melbourne, Australia: PSA, 1994. 21 NSW Retail Tobacco Traders' Association. New Winfield 25s. The Australian Retail Tobacconist 1977;37(March):13. 22 Scollo M. Chapter 13. The pricing and taxation of tobacco products in Australia. In: Scollo, M, and Winstanley, M, ed. Tobacco in Australia: Facts and Issues. Melbourne, Australia: Cancer Council Victoria, 2008. Available from: Tobacco in Australia website 21 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 23 Deloitte. Illicit trade of tobacco in Australia: Report for 2011. Sydney: A report prepared for British American Tobacco Australia Limited, Philip Morris Limited and Imperial Tobacco Australia Limited, May 2012. Available from: British American Tobacco Australia website 24 Deloitte. Illicit trade of tobacco in Australia: Report for 2011. Sydney: A report prepared for British American Tobacco Australia Limited, Philip Morris Limited and Imperial Tobacco Australia Limited, May 2012. Available from: British American Tobacco Australia website 25 Quit Victoria. Illicit trade of tobacco in Australia: Report for 2011: a report prepared for British American Tobacco Australia Limited, Philip Morris Limited and Imperial Tobacco Australia Limited, May 2012. A critique by Quit Victoria, May 2012. Available from: Cancer Council Victoria website 26 Plibersek T. Minister Welcomes Move on Duty-Free Tobacco [Media Release]. Canberra: Minister for Health, 8 May 2012. Available from: Department of Health and Ageing website 22 6.3 Bolster and build on existing programs and partnerships to reduce smoking rates among Aboriginal and Torres Strait Islander (ATSI) people. Comments related to Action Items related to reaching Indigenous and disadvantaged populations. (Action items 6.3, 6.4 and 6.8). Quit Victoria acknowledges the clear intention within the draft strategy clearly outlines to consolidate efforts to date plus further advance efforts to reduce smoking rates and behaviours in the high smoking rate populations. We recommend that the objective specifically related to reducing smoking among Aboriginal and Torres Strait Islander people, groups at higher risk from smoking and other disadvantaged populations with high smoking prevalence be broadened to include reducing exposure to tobacco smoke (ETS) and harm from continuing to smoke. Reducing smoking in public places, community and recreational events and by individuals from less affluent areas in their homes and cars, will reduce consumption and reduce exposure to ETS among disadvantaged children who are currently exposed to ETS at a much higher rate. It will also help to de-normalise smoking among disadvantaged communities which should both drive down uptake and increase cessation. Action 6.3.1 Continue the investment in, and roll out of existing and planned national and State and Territory programs to reduce Aboriginal and Torres Strait Islander smoking. The National Partnership Agreement for Closing the Gap (CTG) and other funding initiatives by both Commonwealth and State/Territory governments there has represented significant level of investment towards activity in reducing smoking rates among Aboriginal and Torres Strait Islander (ATSI) people. This has been the first government funding allocated to tobacco control for Aboriginal people in Victoria. Activities include: The roll out of national programs to develop and test new initiatives to engage with ATSI communities The development of capacity within existing Aboriginal and mainstream health workforce to address tobacco use with clients and in Aboriginal communities. Enhancing existing mainstream cessation support services, such as the Quitline service, for ATSI people Development of both national and local social marketing tools and messages, to raise awareness and support ATSI people to access quitting services Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 The reinforcement of smokefree policies in all Aboriginal Health services and other services supporting ASTI people. This work cannot be continued or further developed without further Commonwealth, State and Territory government funding, to support the Aboriginal health workforce, and to appropriately tailor and promote mainstream services to ATSI people to reduce smoking disparities between the ATSI and non-ATSI population 6.3.2 Monitor and evaluate the impact of these initiatives and use this data to inform and refine future programs to reduce Indigenous smoking. Responsibility: Australian Government; State and Territory governments and Aboriginal community controlled organisations and non-government organisations. Quit Victoria recommends the development and support for a National (or State and Territory) system through which evaluation data from initiatives to reduce ATSI smoking can be collected, analysed and disseminated. A system of this kind could support the shared learnings from current programs; the development of evidence based interventions and efficiencies in rolling out those interventions found to be most effective in reducing smoking among ATSI people. For example, the Quitline Enhancement project was rolled out in 2011, an initiative to enhance Quitline services for Aboriginal and Torres Strait Islander people. This Commonwealth and State/Territory funded program is being evaluated and results shared at local and national levels. An initial Face-to-face meeting is currently being held between Government, NGO and Quitline services to discuss local evaluation strategies and to share initial findings as programs are rolled out. However a strategy for dissemination of these findings is yet to be finalised. 6.3.3 Continue to build tobacco control capacity within Aboriginal community controlled organisations. Responsibility: Australian Government; Aboriginal community controlled organisations and State and Territory governments and non-government organisations. Quit Victoria has conducted Aboriginal Health Worker Training in Victoria and other jurisdiction for over a decade and recognises the importance of building capacity within Aboriginal health and community controlled organisations as an effective way of 24 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 encouraging and supporting Aboriginal smokers to address their smoking. However it should also be recognised that many Aboriginal people also access mainstream services for health care, so this capacity building in culturally sensitive and appropriate smoking cessation support should also occur within these services. In all states and territories, non-government organisations have fostered positive partnerships with Aboriginal community controlled organisations. In Victoria, there have been many collaborative efforts between Quit Victoria and Aboriginal community controlled organisations to build their organisational capability through training, information sharing and smoke free policy advice, as well as research projects. An example of this is the VACCHO smoking in pregnancy project, funded by the Victorian government, which aims to build capacity in three Victorian Koorie Maternity Services to trial interventions to better support women who smoke (including pregnant women) to reduce consumption or quit smoking. 6.3.4 Support Aboriginal and Torres Strait Islander organisations to move towards smoke free workplaces and events. Responsibility: Aboriginal community controlled organisations; Australian Government; State and Territory governments and non-government organisations. Quit Victoria recommends consideration of a funded program for the implementation of smokefree workplaces. Funding would provide for organisational smoke free policy development, planning and staged implementation, monitoring and evaluation. Furthermore Quit believes it is important that additional support be provided to staff of ATSI organisations, including skill development in policy document writing, implementation planning and monitoring. This should be complemented by cessation support through access to NRT for staff who smoke and for clients accessing these services. Studies among Aboriginal health workers have found that the majority of health workers want to quit and have made at least one quit attempt in the past.1234 A requirement for establishment and compliance of organisational smokefree workplace policy could form part of funding agreements for these organisations to reinforce this initiative. 25 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Quit recommends that non-government organisations have an important role in this process. Quit Victoria has supported the implementation of smokefree policy within the Victorian Aboriginal Health Service and provides policy support and advice for a range of organisations moving toward and creating smokefree environments. 6.3.5 Strengthen partnerships and collaboration between Aboriginal and Torres Strait Islander organisations, governments and non-government organisations. Responsibility: Australian Government; State and Territory governments, Indigenous organisations; and non-government organisations. Agree. Strengthening partnerships and collaboration can provide for consistent practises to de-normalise smoking among the ATSI population and can help reduce exposure to secondhand smoke, and by extension, its impact on the community. 6.3.6 Continue to provide training to Aboriginal Torres Strait Islander health workers and other relevant health workers in effective tobacco control interventions. Responsibility: Australian Government; State and Territory governments and nongovernment organisations. Early indications show that developing cessation support skills, including brief intervention training and establishing protocols for referrals into effective cessation services, such as Quitline, have been shown to be an effective mechanism in supporting smokers to reduce their tobacco use and quit successfully. This as a model operating in the general population has been shown to be highly efficacious. In a recent study, patients who were provided with in-practice cessation support plus Quitline referral were three times more likely to have sustained abstinence at 12 months than those who received in practice advice alone5. Quit recommends this training continue to be competency based. Training should be comparable across jurisdictions to ensure capacity building in the existing and new workforce is comparable across jurisdictions. Quit recommends that in addition to this action item, training is continually evaluated and reviewed for effectiveness in embedding practise change, as well as supporting behaviour change among smokers. 26 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Responsibility should be extended to non-government organisations. Quit Victoria has a long history of providing evidence based training and support into Aboriginal health services to support skills development and delivery of cessation support. Post training evaluation of Quit Victoria’s training shows increased levels of skill and confidence in the workforce to provide brief intervention. In 2009, Quit Victoria evaluated its Aboriginal training program by surveying Aboriginal health and community training participants. Ninety percent of respondents gave positive feedback and as a result of training, confidence to raise the issue of smoking was 93% and confidence to use and refer clients to Quitline was 98%. Overall, the evaluation indicates that the Aboriginal smoking cessation training program had achieved its primary aim to improve understanding of effective smoking cessation interventions, increase confidence to deliver brief intervention and encourage/advocate for implementation of such interventions6. As per comments made at 6.3.4, health workers who smoke should also be provided with additional support to quit, as a component of this Action. 6.3.7 Deliver best practice screening and smoking cessation as part of routine health service delivery to Aboriginal and Torres Strait Islander clients. Responsibility: Australian Government; State and Territory governments; Aboriginal community controlled organisations and mainstream health services. Agree. As noted in 6.3.6 it is vital that all enhancement of workforce capacity be evidence based (best practise) and competency based, ensuring that workers delivering smoking cessation as part of routine service delivery are equipped with appropriate skills and resources to effectively support behaviour change in their clients. As above, Quit Victoria and other NGO’s are currently supporting this Action through the skill development of health workers to effectively deliver smoking cessation— particularly brief interventions—as a part of routine healthcare. In addition, routine screening and brief intervention in smoking cessation should also be integrated with routine referral to those Quitline services with specific Indigenous counsellors and protocols for all clients who smoke, along with routine recording of smoking status of all clients. Quitline, along with health worker support and brief interventions, has been demonstrated to enhance quit attempt success 7. 27 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 6.3.8 Encourage Aboriginal and Torres Strait Islander people to access subsidised NRT, identify any barriers to access, and develop strategies to overcome these barriers. Responsibility: Australian and State and Territory Governments and non-government organisations. Agree. However ‘non-government organisations’ as well as ‘state and territory governments’ should be included under ‘Responsibility’. Some of the barriers that have been identified among Aboriginal and Torres Strait Islander people with regard to accessing subsidised NRT include the requirement for a GP script for subsidised NRT. In addition some communities may have limited access to GPs (particularly remote communities) and medications. Removing these barriers would help many more Aboriginal and Torres Strait Islander people access NRT. Quit Victoria recommends that further Nurse Practitioners be authorised to issue prescriptions for NRT in addition to GPs 8. Some Aboriginal Medical Services stock their own medications including NRT, and can dispense NRT to their clients at any time. This may be a good mechanism for many other Aboriginal medical services9. 6.3.9 Encourage and support Aboriginal and Torres Strait Islander pregnant women and their families to quit and provide messages about the harm associated with ETS exposure. Responsibility: Australian Government; State and Territory governments and Aboriginal community controlled organisations and non-government organisations. Agree. Responsibility should be broadened to include non-government organisations. The effects of smoking on infant health are well known leading to lower birth weight, pre term birth and prenatal death. 10 11 12 Smoking rates among Aboriginal and Torres Strait Islander women during pregnancy remains higher than pregnant smokers of non-Aboriginal and Torres Strait Islander background13. . Similarly, rates of smoking in the home are higher among the Aboriginal and Torres Strait Islander population than among the non-Aboriginal and Torres Strait Islander population.14 15 However, two studies of pregnant women in Townsville found that the women may have been more motivated, and able to quit smoking during their pregnancy1617. This supports 28 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 other studies that show pregnancy represents a critical point in time of high motivation to quit or change smoking behaviours (reduce consumption, make a quit attempt) and contribute to successful quit attempts Additional competency based training must be provided to health workers to ensure they are well-equipped to provide cessation support to pregnant Aboriginal and Torres Strait Islander women. 6.3.10 Enhance social marketing campaigns for Aboriginal and Torres Strait Islander people using effective mainstream campaigns and complemented by Indigenous-specific campaign elements and local community-specific campaigns. Responsibility: Australian Government; State and Territory governments; Aboriginal community controlled organisations and non-government organisations Agree. Quit Victoria recommends inclusion of non-government organisations within ‘responsibility’. Quit Victoria has extensive experience in developing effective social marketing campaigns as well as strong relationships with a number of Aboriginal Health Services. Quit recommends leveraging this experience and existing relationships and partnerships to both promote smoke-free and quitting activity by creating locally appropriate messages. All activity would complement any existing Commonwealth social marketing activity and/or other local grass roots community efforts. We believe the main elements of an Aboriginal special social marketing campaign should include where possible: Promotion of the enhanced Aboriginal Quitline service to Aboriginal smokers in identified communities through local media (potentially regional TV, radio, print and outdoor) and printed collateral disseminated in Aboriginal Health Services and communities. The identification of local champions within the community to use their stories/testimonials within the communications materials. These stories could be also used in a DVD for local Aboriginal health services. 29 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Work within health services, local alcohol and drug services and youth services to provide training to staff, to complement social marketing activities. Provide appropriate sponsorship opportunities for local sports or community activity (including signage at grounds or venues). Develop digital media activity within Aboriginal health websites. The aim of these activities would be to provide information about the harmful effects of smoking and details about quit supports. 6.3.11 Improve understanding of barriers to successful smoking cessation in Aboriginal and Torres Strait Islander populations and any areas in which they differ from those in the general population. Responsibility: Australian Government; State and Territory governments and Aboriginal community controlled. Agree. However Quit Victoria recommends extending this Action to include ‘improving understanding of the barriers to uptake of cessation services’. There are opportunities for nongovernment organisations to engage with state and territory governments and other agencies, in the collection and dissemination of evidence relating to barriers in smoking cessation and the uptake of cessation services among the Aboriginal and Torres Strait Islander populations. For example, data collected on the uptake of the Quitline service among the Aboriginal and Torres Strait Islander population could contribute to this evidence base. 1 Lindorff KJ. Tobacco time for action: National Aboriginal and Torres Strait IslanderTobacco Control Project final report. Canberra: National Aboriginal Community Controlled Organisations, 2002. Available from: http://www.naccho.org.au/Files/Documents/NACCHO_Tobacco_report.pdf (This website link was valid at the time of submission) 2 Andrews B, Oates F and Naden P. Smoking among Aboriginal health workers: findings of a 1995 survey in western New South Wales. Australian and New Zealand Journal of Public Health 1997;21:789–90. Available from: National Center for Biotechnology Information website 3 West L, Young D and Lloyd J. A Report on Far North Queensland Aboriginal and Torres StraitIslander health workers. Knowledge, attitudes and beliefs about smoking cessation and prevention. Cairns: Queensland Health, 1998. 4 Mark A, McLeod I, Booker J and Ardler C. Aboriginal health worker smoking: a barrier to lower community smoking rates? Aboriginal and Islander Health Worker Journal 2005;29(5):22–6. Available from: Informit website 30 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 5 Borland, R., Balmford, J., Bishop, N., Segan, C., Piterman, L., McKay-Brown, L., Kirby, C., Tasker, C. (2008) In-practice management vs. quitline referral for enhancing smoking cessation in general practice: A cluster randomised trial. Family Practice, 25: 382-389 6 Abott, J. Centre for Behavioural Research in Cancer (July 2009) - unpublished. Internal Memo to Fiona Sharkie, Luke Atkin, Toni Mason, Edwina Pearce and Kylie Lindorff, Quit Victoria, Cancer Council Victoria. 7 Zwar N, Richmond R, Borland R, Peters M, Litt J, Bell J, Caldwell B, Ferretter I. Supporting Smoking Cessation: A guide for health professionals. Melbourne: The Royal Australian College of General Practitioners, 2011. 8 Australian Government: Department of Health and Aging. Nurse Practitioner PBS prescribing. www.pbs.gov.au/browse/nurse 9 Stoneman J, Taylor SJ. Improving access to Medicines in urban, regional and rural Aboriginal communities- is expansion of Sction 100 the answer? Rural and Remote Health 7:738. 2007 10 Fleming P, and Blair P. Sudden Infant Death Syndrome and parental smoking. Early Human Development. 2007;83(11):721−5. Available from: National Center for Biotechnology Information website 11 Salihu HM, and Wilson RE. Epidemiology of prenatal smoking and perinatal outcomes. Early Human Development. 2007;83(11):713-20. Available from: National Center for Biotechnology Information website 12 Aliyu MH, Salihu HM, Wilson RE, and Kirby RS. Prenatal smoking and risk of intrapartum stillbirth. Archives of environmental & occupational health. 2007;62(2):87-92. Available from: National Center for Biotechnology Information website 13 Australian Institute of Health and Welfare. Substance Use among Aboriginal and Torres Strait Islander people. Canberra: AIHW, 2011. Available from: Australian Institute of Health and Welfare website 14 Johnston V, Thomas DP, McDonnell J, et al. Maternal smoking and smoking in the household during pregnancy and postpartum: findings from an Indigenous cohort in the Northern Territory. Med J Aust 2011;194:556–9. 15 Australian Bureau of Statistics. 4704.0-The Health and Welfare of Australia's Aboriginal and Torres Strait Islander Peoples. Canberra, ACT: ABS, 2010 16 Heath D, Panaretto K, Manessis V, Larkins S, Malouf P, Reilly E, et al. Factors to consider in smoking interventions for Indigenous women. Australian Journal of Primary Health 2006;12(2):131–5. Available from: CSIRO Publishing website 17 Panaretto K, Mitchell M, Anderson L, Gilligan C, Buettner P, Larkins S, et al. Tobacco use and measuring nicotine dependence among urban Indigenous pregnant women. Medical Journal of Australia 2009;191(10):554–7. Available from: The Medical Journal of Australia website 31 6.4 Strengthen efforts to reduce smoking among people in disadvantaged populations with high smoking prevalence 6.4.1 Identify and form new partnerships between governments, NGOs with tobacco control expertise, social service organisations and mental health care providers to reduce smoking among disadvantaged groups. Responsibility: Non-government organisations; social service organisations (both government and non-government); mental health care organisations; Australian government; State and Territory governments. Agree. This will support a whole of population approach to smoking prevalence among disadvantaged populations. There is a more recent reference to the one cited related to smoking among people with psychotic illness which we bring to your attention. There are a number of examples that demonstrate the effectiveness of partnering tobacco control expertise with social service and mental health organisations. On example from the United States is that of Break Free Alliance. The Break Free Alliance is a program of the Health Education Council (a non-government organisation) and has been funded by various United State government departments since 2001. The mission of Break Free Alliance is to reduce tobacco use among populations of low socioeconomic status across the United States. Break Free Alliance collaborate with partner organisations who serve low SES populations to: • Build their institutional capacity in tobacco control • Assist with tobacco control education, activities and policy development • Work with state tobacco programs, committees and regions to collaborate with other networks The Break Free Alliance website houses a repository of organisational tools and research re: promising approaches at Health Education Council website. In addition the work in NSW through the CCNSW Tackling Tobacco program. The program aims to reduce the harm that smoking causes amongst disadvantaged groups with the highest smoking rates. The target groups for phase 1 of the program included: people with mental Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 illness; people with drug and alcohol problems; homeless people; lone mothers; vulnerable young people and Aboriginal people. The Tackling Tobacco Program partners with social and community service organisations to raise awareness of higher smoking rates among disadvantaged groups as a social justice issue. The program aims to: Increase the capacity of the social and community service sector to address tobacco issues; Create quit-friendly service environments Increase support to clients of social and community service organisations interested in quitting. Tackling Tobacco has been picked up and rolled out on a smaller scale into South Australia under the Tobacco and Mental Health Project1. 6.4.2 Expand effective programs and frameworks to reduce smoking among disadvantaged groups. Responsibility: Non-government organisations; social service organisations; Australian Government; State and Territory governments. Agree. In addition, Cancer Council Victoria and Quit Victoria recommend that “effective programs” be given greater explanation in Action area 6.4.2. To foster this expansion of programs and frameworks, a system/s of disseminating evidence on these programs and frameworks should be employed. But as highlighted above there are a number of programs that have been developed in both international and local settings. Cancer Council Victoria and Quit Victoria suggests and has been involved in conversations and a Smoking and Disadvantage roundtable workshop hosted by Cancer Council Western Australia to discuss further expansion and collaboration on reducing smoking among disadvantaged groups. Quit Victoria suggests that there is a role for ANPHA in this work. 6.4.3 Build the capacity of social service organisations and mental health care providers to include tobacco control interventions as part of case management approaches. Responsibility: Non-government organisations; social service organisations; Australian Government; State and Territory governments. Agree, with the expansion of this statement to include the community as well as social service sector. As part of the Cancer Council NSW Tackling Tobacco program the delivery 33 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 of free Tackling Tobacco-smoking care training was identified as a crucial element to increase the sectors’ capacity to address tobacco issues and support clients to quit. Again in the Tobacco and Mental Health project (QuitSA) the focus was on three areas : 1) raising awareness of tobacco and support available to quit/ reduce smoking; 2) supporting smoke free policy and practice in mental health services (acute and community based); and 3) delivering best practice smoking cessation/reduction programs. This capacity building in both cases was found to the crucial in integrating and embedding tobacco control into existing programs. 6.4.4 Increase collaboration and referral between mental health care services, social service organisations and Quitline services. Responsibility: Australian Government; State and Territory governments; Quitline services; health services; social service organisations. Agree, although this should also include the NGO sector. Quit Victoria with Beyond Blue ran a pilot study looking at the effectiveness of the Victorian Quitline service in supporting people with mental health issues in a co-managed arrangement with their primary care provider. The Quitline was shown to be a well received and appropriate service for people with mental health issues and improved cessation outcomes2. Enhancement and reinforcement of referral pathways from mental health care services is shown to be an effective mechanism to support smokers to stop smoking3. Further we suggest promoting the adoption or development of strategies of the efficacy of Quitline referral to mental health and social service organisations, as a further means of supporting the integration of smoking cessation advice and the management of nicotine dependence as part of routine care. 6.4.6 Ensure that mental health services and drug treatment agencies are smokefree. Responsibility: State and Territory governments; Australian Government. Agree, however Cancer Council Victoria and Quit Victoria suggest this should be extended to community and social service sector organisations as well. This should be a component of comprehensive response to tobacco smoking. Many government funded services now have funding agreements that are conditional on being smokefree and the Cancer Council of Victoria and Quit Victoria is supportive of this. However this must be combined with 34 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 cessation support for staff, enhanced access to NRT for staff and clients and supported by management and clinical/support staff. 6.4.7 Enhance partnerships and collaboration between State and Territory custodial authorities, health agencies and non-government organisations with expertise in tobacco control. Responsibility: State and Territory governments; non-government organisations. Agree. Smoking in prison populations remains a significant problem and must be addressed with a supportive approach. Quit Victoria recently developed a DVD for prisoners on quitting on the inside and this is currently being rolled out nationally by DOHA. In addition there are already examples of partnership and collaboration. A National Summit on Tobacco smoking in Prisons was convened in 2010 with a report released in 2011 summarising principles and priority areas for action. The report also drew on the approaches of New Zealand and Canada in their implementation of totally smoke free prisons. Quit Victoria also suggests monitoring the outcomes of the New Zealand smoke free prisons approach (commenced July 2011) and using the principles in the Summit Report (2011) to inform future action. 6.4.8 Develop implement and evaluate policies and programs to reduce exposure to ETS and encourage smokers to quit in correctional facilities. Responsibility: State and Territory governments. Agree. As in 6.4.7 there are examples of successful approaches to encouraging prisoners to quit smoking such as the Quit Victoria “Quitters are Winners” and the more recent DVD project. Quit strongly endorses an evidence based approach to supporting prisoners to quit smoking and in developing and implementing policies to reduce exposure to ETS. As above Quit Victoria suggests reviewing the evidence available locally and internationally to support effective policy changes to reducing exposure to ETS and smoking in correctional facilities. Quit Victoria recommends this action area extend to include developing options for smokefree correctional facility rollout. 6.4.9 Establish a state and territory working group to provide leadership on smoking in prisons and oversee and facilitate progress in this area. Responsibility: State and Territory governments. 35 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Agreed noting the comments at 6.4.8 and 6.4.9 6.4.10 Provide greater smoking cessation support for prisoners including access to NRT and other pharmacotherapies. Responsibility: State and Territory governments. Agree. There are evidence based programs currently available such as the Quitters are Winners program 4. However Quit Victoria notes that access to cessation supports differs from facility to facility. The Cancer Council of Victoria and Quit Victoria endorses an approach that would involve correctional facility management, jurisdictional Justice Departments and a national working group to collaboratively develop solutions to enhance access to cessation support. 6.4.11 Continue to build the evidence base to identify effective approaches to reducing smoking among disadvantaged populations. Responsibility: State and Territory governments; Australian Government; research organisations. Agree. NGO’s should share this responsibility, particularly the contribution to the evidence base a number of local NGOs (CCNSW, CCSA) are already making. Current population level surveys do not capture the broad range of behaviour change that may result from tobacco control interventions. Smoking rates are measured by number of regular smokers (daily and weekly) and number of people who have made successful quit attempts. Working in partnership, a national framework of indicators could be developed to measure organisational change and impact of approaches as well as a broad range of client outcomes reduction in tobacco smoked, change in home environments (e.g. not smoking inside, around children), number of quit attempts made, and client learning from relapses. 1 Scoping Paper - Tobacco Related Disparities and Social Disadvantage in Victoria, M. Chiller for Quit Victoria, June 2012, unpublished. 2 Segan C, Borland R, Wilhelm K, et al Helping Smokers with depressions to quit smoking: collaborative care with Quitline. Medical Journal of Australia 2011: 195 (3): 7. 3 Segan C, Borland R, Wilhelm K, et al Helping Smokers with depressions to quit smoking: collaborative care with Quitline. Medical Journal of Australia 2011: 195 (3): 7. 4 McCarthy M, Brewster J, Evaluation of the Quitters are Winners course a prison based cessation program: CBRC Research Paper Series No.38 36 6.5 Eliminate remaining advertising, promotion and sponsorship of tobacco products Actions 6.5.1 Fully implement plain packaging laws by 1 December 2012. Cancer Council Victoria and Quit Victoria acknowledges that, subject to a successful defence in the tobacco industry High Court of Australia challenge, plain packaging laws will commence on 1 December 2012. Following implementation, this action point will be redundant. Action 6.5.3 reflects the challenges facing plain packaging laws post implementation. In the lead up to the legislated implementation of the laws, we recommend that the highest priority be given to defending the laws and ensuring that they are implemented on 1 December 2012. 6.5.2 Fully implement updated and larger health warnings on tobacco packaging by 1 December 2012 and monitor the need for further updating of health warnings. Cancer Council Victoria and Quit Victoria strongly supports the updated and larger health warnings provided in the Competition and Consumer (Tobacco) Information Standard 2011 and awaits their full implementation on 1 December 2012. In particular, Quit supports the increased size of the health warning on the front surface of packs to 75%. To ensure that the health warnings have maximum impact, we recommend the establishment of a designated authority (such as the Chief Medical Officer) to: implement a new system for providing consumer product information to smokers which ensures that package health warnings are reviewed more regularly and amended where necessary to maintain their effectiveness; and prepare a bulletin that provides more frequent and rapid warnings to consumers through news media and at the point of sale. 6.5.3 Monitor and enforce legislation relating to the plain packaging of cigarettes and non-cigarette tobacco products and the new graphic health warnings as specified in the Competition and Consumer (Tobacco) Information Standard 2011 Cancer Council Victoria and Quit Victoria supports the full enforcement of the plain packaging laws and the new graphic health warnings from 1 December 2012. Given the long consultation period, and long lead time provided to tobacco manufacturers to prepare for Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 plain packaging, we believe that plain packaging laws and the new regulations involving graphic health warnings be enforced from commencement. We further recommend that the penalties available in the legislation for non-compliance be strictly applied and ‘warnings’ for any breaches only be used in the first month for minor breaches by small scale individual retailers. As part of the government’s enforcement measures, we also recommend that an online system be established where breaches can be reported, and subsequently investigated. 6.5.4 Investigate the possible benefits of Require tobacco companies to report regularly on expenditure on any form of tobacco promotion and marketing activity. Cancer Council Victoria and Quit Victoria supports the federal government’s ongoing efforts, through the introduction of plain packaging laws and the prohibition on online tobacco advertising, to ensure Australia meets its obligations under Article 13 of the FCTC. The guidelines for the implementation of Article 13 adopted by the Conference of the Parties to the FCTC (COP) includes the following recommendation: “each party shalI…require…the disclosure to relevant governmental authorities of expenditures by the tobacco industry on advertising promotion and sponsorship not yet prohibited. Those authorities may decide to make those figures available, subject to national law, to the public…”1 To ensure continued compliance with the FCTC, Cancer Council Victoria and Quit Victoria recommends the immediate implementation of regulations to monitor tobacco industry expenditure on marketing and advertising. Identifying and acting to remove all remaining forms of advertising, promotion and sponsorship is critical to ensure smoking continues to decrease in Australia. Reporting should include expenditure on price-relation promotion such as stock discounts to retailers. In the US where companies have been required for many years to report on promotional expenditure to the Federal Trade Commission, expenditure on pricerelated promotions has been the most important category of expenditure in recent years. 38 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 We recommend that the Australian government urgently: Amend the Tobacco Advertising Prohibition Act 1992 to compel the tobacco companies to report regularly on expenditure on all the forms of advertising, promotion and sponsorship as defined in the Appendix to the FCTC Guidelines for implementation for Article 132. 6.5.5 Explore regulatory options to eliminate any remaining forms of tobacco promotion including use of advertising of price specials, public relations activities, payments and incentives programs between tobacco manufacturers, wholesalers, and retailers and proprietors of hospitality venues. Cancer Council Victoria and Quit Victoria supports the elimination of any residual opportunities available to the tobacco industry to use price specials, public relations activities, payments and incentives to retailers and proprietors of hospitality venues. As a signatory party to the FCTC, Australia has an obligation to ban all forms of tobacco advertising, promotion and sponsorship. Accordingly, we strongly support the immediate implementation of amendments to the TAP Act to ban: 39 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Incentive payments to wholesalers, retailers and proprietors of hospitality venues Public relations activities, including promotion of corporate images and ‘corporate responsibility’ donations. Retailers from encouraging consumers to purchase, one or more brands or products; Tobacco manufacturers or retailers offering discounts on certain products lines; A licensee giving tobacco companies the right to promote or exclusively sell a tobacco product or brand at pubs, clubs or other venues or events; Tobacco manufacturers providing funds for building renovations to accommodate smokers; and The tobacco industry promoting the sale of tobacco products and tobacco use as a means to achieve retailer reward programs (eg rewards for achieving certain sales volumes), loyalty programs, incentives to staff and rebates and price supports. This includes encouraging third parties, such as retailers, venue occupiers or event managers, to promote tobacco products or smoking. Tobacco companies often enter into arrangements with licensed premises and other public venues that confer on tobacco companies the right to sell certain products exclusively, or to promote smoking or tobacco products in other ways. The guidelines on implementation of Article 13 of the FCTC recommend that the following types of tobacco sponsorship be banned: “payment or other consideration in exchange for the exclusive sale of a particular product or particular manufacturer’s product in a retail outlet, at a venues or at any event, or prominent display of a product”. “provision of financial or other support by the tobacco industry to venue operators, such as pubs, clubs or other recreational venues, in exchange for building or renovating premises to promote tobacco products or use or provision of awnings and sunshades”.3 40 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Persons or organisations who have a direct or indirect commercial interest in promoting the sale or use of tobacco products should be banned from making contributions to events, activities or individuals, with the aim, effect or likely effect of promoting a tobacco product or tobacco use. Prohibited acts should include the provision of funding by the tobacco industry for the creation, fitting out and furnishing of smoking areas and the funding of third parties (such as the Australian Hotel’s Association or the Australian Retailers’ Association) by tobacco companies to sponsor events and venues. Quit Victoria is concerned that public acknowledgements of tobacco industry assistance or support (ie sponsorship) are excluded from the definition of “publish a tobacco advertisement” if they comply with regulations made under the Act.4 This exception creates avenues for tobacco companies, through sponsorship to build associations in the public consciousness between the tobacco industry and sporting and cultural events, community projects and the like. The guidelines for implementation of Article 13 of the FCTC recommend that: “The Parties should ban contributions from tobacco companies to any other entity for ‘socially responsible causes’, as this is a form of sponsorship. Publicity given to ‘socially responsible’ business practices of the tobacco industry should be banned, as it constitutes advertising and promotion”.5 We recommend that section 10(5) of the TAP Act should be repealed in favour of an express ban on all forms of sponsorship and commercial promotions of tobacco products at all public events and social venues. This should include a ban on publicity in relation to tobacco industry sponsorship of events or causes.6 6.5.6 Consider and develop regulatory options to prohibit the remaining display of tobacco products at point of sale. 41 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Quit Victoria recommends immediate law reforms to ban point of sale tobacco displays. Tobacco displays normalise smoking (particularly in the eyes of children), promote brand awareness and can act as a visual cue that contributes to smoking initiation, making it harder for smokers to quit and causes recent quitters to relapse.7 The guidelines for the implementation of Article 13 of the FCTC state: “Display and visibility of tobacco products at points of sale constitutes advertising and promotion and should therefore be banned.”8 Presently, point of sale bans are the responsibility of State and Territory governments with varying implementation dates and exemptions. For example in New South Wales the government has given specialist tobacconists’ an exemption from complying with display bans until 1 July 2013.9 A date for the removal of tobacco displays for specialist tobacconists’ in Victoria has not been set. We propose that point of sale bans should be standardised across the country. To satisfy its obligations as a party to the FCTC, we recommend that the Australian government provide the states and territories with a timeframe of 1 July 2014 in which to remove all point of sale tobacco displays, including those of ‘specialist tobacconists’. If the timeframe is not satisfied, the Commonwealth should revoke section 16 of the TAP Act and substitute this section with a requirement that tobacco products be stored out of sight of members of the public at any place where tobacco products are offered for sale to the public. The ban should apply to all tobacco retailers including: specialist tobacconists’ and duty free outlets. Price boards or paper lists of available product lines should be the only information provided for consumers to make their purchase decisions. The size of these boards, the font and format used and the information included on a price board should be standardised to ensure that they are visible only to the customer making the purchase and any branding, tobacco industry trade marks or discount tickets should be prohibited from appearing on price boards. It should also be mandatory for products to be placed in alphabetical order on a price board to ensure tobacco manufacturers do not collude with retailers to obtain or demand priority placement. 42 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 6.5.7 Restrict the advertising of tobacco products on the internet by passing the Tobacco Advertising Prohibition Amendment Bill 2010. Cancer Council Victoria and Quit Victoria recognise that as of 6 September 2012, this action item is out of date. We applaud the passing of the Tobacco Advertising Prohibition Amendment Bill 2010 restricting online advertising of tobacco products. We recommend that the action item be updated to require the immediate implementation of enforcement mechanisms to ensure the government can adequately respond to breaches of the Act. 6.5.8 Explore the possible benefits of regulatory restrictions on incentive programs between tobacco manufacturers, wholesalers and retailers. We believe that this action item is repetitive of action item 6.5.5 and as such should be deleted and action item 6.5.5 amended as per the suggestion above. 6.5.9 Consider and develop regulatory options to remove tobacco from retailer shopper and reward schemes. Many retailers currently include tobacco as a product that can be purchased to amass points as part of “Fly Buys”, “Everyday Rewards” and other similar schemes. The guidelines on the implementation of Article 13 recommends that the following be banned: “incentive promotions or loyalty schemes, e.g. redeemable coupons provided with purchase of tobacco products.” 10 We recommend that the TAP Act be immediately amended to ban tobacco from being included in manufacturers’ and/or retailers’ use of consumer reward schemes which are used to induce consumers into purchasing products for the purposes of accruing points that can be offset against future purchases or other rewards. 6.5.10 Consider and develop policies and regulatory options consistent with Article 5.3 of the FCTC to prevent tobacco company interference in public health policies. 43 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Article 5.3 applies to all tobacco control policies and does not belong as an action item under one particular priority. It is our view that Article 5.3 should be an overarching principle of the entire National Tobacco Strategy with associated actions adopted by all levels of government. Please see our comments in Part 1 – Overarching Issues. 6.5.11 Continue to monitor the portrayal of smoking in movies and the adequacy of the current classification guidelines. Cancer Council Victoria and Quit Victoria recognise the authority of cinema to cast certain behaviours and images in ways that normalise the conduct. To ensure that tobacco use is not misused in films, we support the recommendations of the National Preventative Health Taskforce that tobacco use in cinema be immediately made a ‘classifiable element’ the result of which would see that films exhibiting tobacco use with particularly seductive portrayals of smoking be categorised with a restrictive classification.11 We also support the Taskforces recommendations to: Produce a set of guidance notes to the Board based on findings of the literature on the impact of portrayals of smoking on young people. Fund a project to raise awareness among people working in the Australian film and entertainment industries of the damaging effects of seductive portrayals of smoking in popular entertainment viewed by children. Include training to decode depictions of smoking in movies in drug education in schools. To assess the effectiveness of this policy, commission a suitable agency to commence ongoing monitoring of the exposure of Australian teenagers (concentrating on those aged 14–15 years) to portrayals of smoking in movies (both at the cinema and on DVD) and computer games. At present, we are not aware of any government or non-government organisation monitoring the prevalence of portrayals of smoking in television, cinema or in computer games. 1 Framework Convention on Tobacco Control, opened for signature on 16 June to 22 June 2003, art 13.4(d) (entered into force on 27 February 2005) 44 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 2 Guidelines for implementation of Article 13 (Tobacco advertising, promotion and sponsorship) of the WHO FCTC, adopted by the third session of the FCTC Conference of the Parties, Durban, South Africa, 17-22 November 2008, Appendix. 3 Guidelines for implementation of Article 13 (Tobacco advertising, promotion and sponsorship) of the WHO FCTC, adopted by the third session of the FCTC Conference of the Parties, Durban, South Africa, 17-22 November 2008, Appendix. 4 TAP Act 1992 (Cth), section 10(5) Available from: Com Law website 5 Guidelines for implementation of Article 13 (Tobacco advertising, promotion and sponsorship) of the WHO FCTC, adopted by the third session of the FCTC Conference of the Parties, Durban, South Africa, 17-22 November 2008, Appendix. 6 TAP Act 1992 (Cth), section 10(5) Available from: Com Law website ; Tobacco Act 1987 (Vic), section 10(1). Available from: Victoria Parliament website 7 Wakefield M, Germain D, Henriksen L. The effect of retail cigarettes pack displays on impulse purchase. Addiction. 2007; 103(2):322 – 328; Wakefield M, Germain D, Durkin S, Henriksen L. An experimental study of effects on schoolchildren of exposure to point of sale cigarette advertising and pack displays. Health Education Research 2006; 21(3): 338 8 Guidelines for implementation of Article 13 (Tobacco advertising, promotion and sponsorship) of the WHO FCTC, adopted by the third session of the FCTC Conference of the Parties, Durban, South Africa, 17-22 November 2008, Appendix. paragraph 14 9 Public Health (Tobacco) Act. 2008 (NSW). Schedule 1, Part 2, section 5(3)(a): Available from: NSW Legislation website; Retailer Factsheet 6 NSW Health website<http://www.health.nsw.gov.au/resources/publichealth/healthpromotion/tobacco/pdf/specialist_tobaccon ist_factsheet_6_final.pdf(This website link was valid at the time of submission)> at 20 June 2012 10 Guidelines for implementation of Article 13 (Tobacco advertising, promotion and sponsorship) of the WHO FCTC, adopted by the third session of the FCTC Conference of the Parties, Durban, South Africa, 17-22 November 2008, Appendix. 11 Australia: the healthiest country by 2020. Technical Report No 2 Tobacco control in Australia: making smoking history, Including addendum for October 2008 to June 2009, page 21. Tobacco Control Directorate Health Canada. Canadian Tobacco Use Monitoring Survey (CTUMS). Ottawa: 2008. Available from: http://www.hc-sc.gc.ca/hl-vs/tobac-tabac/research-recherche/ stat/_ctums-esutc_prevalence/prevalence-eng.php 45 6.6 Consider further regulation of the contents, product disclosure and supply of tobacco products and non-therapeutic nicotine delivery systems 6.6.1 Commission research to inform the development of any further regulatory policies on the disclosure of tobacco product ingredients, and emissions data to government authorities and to the public. Partial guidelines for implementation of Articles 9 and 10 of the WHO Framework Convention on Tobacco Control recommend that: “Parties should require that manufacturers and importers of tobacco products disclose to governmental authorities information on the ingredients used in the manufacture of their tobacco products at specified intervals, by product type and for each brand within a brand family.”1 Cancer Council Victoria and Quit Victoria understand that a consultancy has already taken place to investigate development of regulatory policies in this area. We would support public release of the report in order for the broader tobacco control community to take account of the findings. We believe that disclosure of tobacco product ingredients and emissions data is important for government, scientists and the tobacco control community in order to further inform policy regarding potential regulation of these ingredients. The pros and cons of making this information available more broadly to the general public, in what format and who would communicate this should be given consideration with an improvement in public health being the desired outcome, not simply the public having access to a long list of technical ingredients as is currently the case with the voluntary disclosure agreement. 2 6.6.2 Commission research to examine the effects of flavourings and masking agents in increasing palatability of tobacco products and the impact of these substances on smoking behaviours (particularly smoking initiation and uptake) and identify best practice approaches to regulation. 6.6.3 Regulate options to enhance controls on tobacco product ingredients, emissions and product disclosure in line with agreed partial or full guidelines for implementation of Articles 9 and 10 of the FCTC as these are adopted by the Conference of the Parties. Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 6.6.4 Continue to participate in the development of international guidelines for implementation of Articles 9 and 10 of the FCTC. Cancer Council Victoria and Quit Victoria understand that consultancies are either underway or completed in relation to action items 6.6.2 and 6.6.3 and we strongly support the Australian Government’s participation in further development of Guidelines for FCTC Articles 9 and 10. We have recommended a change to the wording of action item 6.6.3 which is slightly confusing. At present the Conference of the Parties (COP) has only adopted partial guidelines for Articles 9 and 10 and work is continuing to complete these guidelines. For example one aspect of the guidelines still to be completed is recommendations around constituents and emissions. Implementation of regulation should be consistent with adoption by the COP of partial or full guidelines as this work progresses. We strongly support state and territory law reforms to ban overtly ‘fruit or lolly’ flavoured cigarettes. Conversely, we are concerned that the ban does not extend to menthol cigarettes or a long list of other flavours that tobacco companies now report as being included in cigarettes. Implementing regulation around palatability is consistent with the FCTC Partial guidelines for implementation of Articles 9 and 10 that recommend: “Parties should regulate, by prohibiting or restricting, ingredients that may be used to increase palatability in tobacco products.”3 New products launched by tobacco companies contain added sugars, sweeteners and other flavours reminiscent of cocktails or liquors. In order to increase their appeal to emerging markets, which are largely youth oriented, the flavoured varieties have often been seasonal or themed based.4 The high sugar content is used to improve the palatability of tobacco products, while the smoke harshness of tobacco is masked with flavours that contribute to promoting and sustaining tobacco use.5 Studies from the US also indicate that flavoured brands are primarily used by younger people.6 47 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 6.6.5 Commission research on electronic cigarettes to examine the risks and/or benefits of these products; determine whether there is a need to increase restrictions on their availability and use; and, identify the most appropriate policy approach for Australia. We are aware that a consultancy on electronic nicotine delivery systems and smokeless tobacco products is underway. We support this consultancy and look forward to the release of the report and the opportunity to consider its findings. We further recognise that federal laws prohibit the sale, possession and use of e-cigarettes that contain nicotine.7 In Victoria, nicotine is a controlled substance which means that a person must not manufacture, sell, supply, purchase, possess or use nicotine without a licence.8 Part of any policy approach to electronic cigarettes should be regulation to ensure that electronic cigarettes cannot be branded, marketed or promoted in any way that would link them to existing tobacco brands, products or companies. 6.6.6 Continue to monitor and enforce legislation prohibiting the sale of tobacco to minors. Cancer Council Victoria and Quit Victoria recommend strengthening laws to ensure tobacco products are not available to minors. As discussed in 6.6.7, we recommend that the best approach to controlling the supply of tobacco products is through a licensing scheme. Research shows that reducing the availability of tobacco products has been associated with lower levels of smoking.9 We recommend that a licensing scheme be structured to enable a designated authority to obtain information about patterns of tobacco supply to youth specific areas; in particular, around schools, dedicated youth events, sporting events, university grounds and university related events. This information could be used to restrict new licenses being issued in these youth specific areas. We also recommend that a graduated penalty structure be implemented as part of reforms to tobacco licensing schemes to penalise retailers who supply tobacco products to minors. This system would mean that tobacco retailers found guilty of 2 or more offences could have their 48 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 license to sell tobacco products removed. We also recommend that a strict liability test apply to infringements. 6.6.7 Consider and explore options to implement tobacco licensing schemes for retailers and wholesalers. Cancer Council Victoria and Quit Victoria recognise the effectiveness of licensing schemes to facilitate the provision of information needed by authorities to adequately enforce tobacco control laws, the provision of information to tobacco retailers and wholesalers regarding their legal obligations and the application of efficient and effective sanctions against retailers who contravene tobacco control laws.10 We also consider licensing schemes as a way of reminding retailers and wholesalers that selling tobacco is an activity that carries significant responsibilities. Licensing schemes enhance the authority of governments to monitor the stages of tobacco production from commencement all the way through to point of sale. This provides governments with considerable data to regularly adjust policy to respond to tobacco industry activities. Cancer Council Victoria and Quit Victoria recommend as a matter of urgency that Victoria and Queensland, the only states in Australia without any form of tobacco licensing, implement laws initiating tobacco licensing at a wholesale and retail level. In order to ensure tobacco laws are adequately enforced, we recommend state and territory governments enact law reforms to strengthen licensing schemes. In strengthening licensing schemes, Quit recommends that: Licensing be extended from tobacco retailers to tobacco wholesalers, where this does not already exist; Licensing fees be set at a level high enough to provide funds for health education, compliance and monitoring Licensing requires provision of data for sales of tobacco at a wholesale and retail level which should be entered into a government initiated information system, and subject to privacy restrictions, be publicly available; Data collected from this government controlled system be used to limit the number and location of tobacco retailer outlets near schools, or in low socio economic areas; 49 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 A process for applying and renewing tobacco licenses be implemented to place the onus on retailers to prove why a license should be granted or renewed; instead of a process where licenses are automatically granted, or depending on the situation, renewed; The granting and renewal of tobacco retail and wholesale licences be based on a “fit and proper person test”; and Licenses be restricted to persons 18 years or older. An expansive licensing scheme that provides governments with data on retail and wholesale transactional activity would strengthen attempts to limit the availability of tobacco in low socio economic areas. Further, placing the onus on wholesalers and retailers to meet a “fit and proper person” test provides licensees with a greater incentive to comply with tobacco control laws, thus buttressing an overarching National Tobacco Strategy. 1 FCTC/COP4(10). Partial guidelines for implementation of Articles 9 and 10 of the WHO Framework Convention on Tobacco Control (Regulation of the contents of tobacco products and Regulation of tobacco product disclosures). Adopted at its fourth session in November 2010, Geneva: World Health Organization, 2010. Available from: http://www.who.int/fctc/guidelines/Decisions9and10.pdf 2 Commonwealth Department of Health and Ageing. Voluntary agreement for the disclosure of the ingredients of cigarettes. Commonwealth Department of Health and Ageing, 2000. Available from: Department of Health and Ageing website 3 FCTC/COP4(10). Partial guidelines for implementation of Articles 9 and 10 of the WHO Framework Convention on Tobacco Control (Regulation of the contents of tobacco products and Regulation of tobacco product disclosures). Adopted at its fourth session in November 2010, Geneva: World Health Organization, 2010. Available from: World Health Organisation website 4 Lewis MJ and Wackowski O. Dealing with an innovative industry: a look at flavored cigarettes promoted by mainstream brands. American Journal of Public Health 2006;96(2):244-51. Available from: American Public Health Association website 5 FCTC/COP4(10). Partial guidelines for implementation of Articles 9 and 10 of the WHO Framework Convention on Tobacco Control (Regulation of the contents of tobacco products and Regulation of tobacco product disclosures). Adopted at its fourth session in November 2010, Geneva: World Health Organization, 2010. Available from: World Health Organisation website 6 Lewis MJ and Wackowski O. Dealing with an innovative industry: a look at flavored cigarettes promoted by mainstream brands. American Journal of Public Health 2006;96(2):244-51. Available from: American Public Health Association website 7 Section 52D(2)(b) of the Therapeutic Goods Act 1989 (Cth) provides the Secretary of Department of Health and Ageing with the authority to prepare or revise the Poisons Standard 2011. Nicotine is Schedule 7 poison. Unless nicotine is prepared and packed for smoking or used by licensed or authorised person it is a controlled substance. 8 Nicotine is a controlled poison according to the 12 (2) of the Drugs Poisons and Controlled Substances Act 1981 (Vic). Section 65 of the Drugs, Poisons and Controlled Substances Regulations 2006 (Vic) provides that a person must not manufacture, sell, supply, purchase or otherwise obtain, possess or use a controlled poison unless the person is licensed or permitted to do so. 9 Hyland A, Travers MJ, Cummings M, et al. Tobacco outlet density and demographics in Erie County, New York. American Journal of Public Health 2000:92:937-40 50 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 10 Licensing of Tobacco Retailers and Wholesalers. Report to the Commonwealth Department of Health and Ageing, endorsed by the Intergovernmental Committee on Drugs. The Allen Consulting Group, December 2002. 51 6.7 Reduce exceptions to smokefree workplaces, public places and other settings The Actions under section 6.7 reflect Australia’s commitment as a party to the World Health Organization Framework Convention on Tobacco Control (FCTC), in relation to Article 8 of the FCTC, under which Australia has an obligation to protect the public from exposure to tobacco smoke. Smokefree legislation is one of the critical population interventions available to the Australian Government and respective states and territories, to reduce smoking rates among the Australian population. Smokefree legislation in public places and other settings ensures protection from secondhand smoke exposure1 and can help to denormalise smoking behaviour, through reshaping public opinion and perceptions of social acceptability of smoking.2 3 Australian research reported that teenagers significantly overestimated the prevalence of smoking among adults as well as among other teenagers. The teens were also more likely to overestimate smoking prevalence if they were from a lower socio-economic status (SES) or Indigenous background.4 Limiting tobacco use in public, reducing areas for opportunities to smoke and changing public attitudes to smoking can all help to prevent smoking experimentation and smoking uptake among youth. 5 6 7 8 Section 6.7 provides appropriate and feasible actions in relation to smokefree legislation, as part of a comprehensive strategy to achieve the aim of the National Partnership Agreement on Preventative Health to reduce smoking prevalence in the population to less than 10% by 2018, and to reduce the health, social, economic costs and health inequality associated with smoking. However further detailed comments and recommendations specific to Actions under 6.7 have been provided below for consideration. In addition, marked in tracked changes below are suggested additional references and edits for inclusion in the opening statement of Section 6.7. Exposure to environmental tobacco smoke (ETS) causes a range of serious adverse health effects in both adults and children. The International Agency for Research on Cancer (IARC) reported on a scientific review of the effectiveness of smoke free policies in reducing population exposure to second-hand Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 smoke.9 It determined that there is sufficient evidence to accept that laws restricting smoking in workplaces and other public places reduce population exposure to second-hand smoke and consumption of cigarettes, and respiratory symptoms in workers. In line with two earlier reviews 10 11 it also found that such policies provide net benefits to business, with no adverse affects on overall sales in the hospitality industry. Article 8 of the FCTC requires Parties to recognise that scientific evidence has unequivocally established that exposure to tobacco smoke causes death, disease and disability and to adopt and implement effective legislative, executive, administrative and/or other measures, providing for protection from exposure to tobacco smoke in indoor workplaces, public transport, indoor public places and, as appropriate, other public places. Evaluation studies of the implementation of smoke free legislation overwhelmingly report that the legislation is popular, compliance is high and the laws are effective in improving air quality and reducing exposure to ETS. A growing body of evidence suggests that these laws can have a broader impact on smoker behaviour particularly among young people. There is increasing evidence that smoke free legislation has an impact on initiation of smoking among young people and that the strength of smoke free restrictions in the legislation is a key factor influencing the uptake of smoking. Smoke free legislation can also influence exposure to ETS in domestic environments. Following the implementation of smoke free legislation in Scotland, there was an increase in the proportion of children reporting a complete ban on smoking in their household. A similar pattern was reported in Queensland following implementation of new smoke free laws in 2006. Smoke free policies at home can increase adults’ chances of quitting. Smoke free legislation is largely the responsibility of States and Territories. Under the previous National Tobacco Strategy there was a significant regulatory reform as State and Territory governments progressively introduced legislation to protect workers and the community from exposure to ETS. Every State and Territory bans smoking in enclosed public places including restaurants and cafes and liquor licensed premises. Indoor environments such as public transit, office buildings, shopping malls, schools and cinemas are also smoke free. All States and Territories except the Northern Territory have also 53 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 prohibited smoking in cars when children are present. There is, however, variability between jurisdictions in terms of exemptions from indoor smoking bans. Non smokers can be exposed to high levels of ETS in outdoor settings when close to or downwind of smokers. As restrictions on smoking in enclosed public places have become more common, smokers are increasingly required to smoke outdoors. Problems arise when smokers cluster around entrances and exits and near air conditioning intake vents to smoke. People who enter and exit the building are exposed to ETS and there may be problems with smoke drift into indoor smoke free areas. States and Territories have different approaches for managing smoking in outdoor areas. Five jurisdictions1 (Western Australia, Queensland, Northern Territory, Tasmania and the Australian Capital Territory) have implemented bans on smoking in outdoor dining areas in cafes, restaurants and licensed premises. In NSW and Victoria, some local council have prohibited smoking in outdoor areas. A number of jurisdictions have also prohibited smoking in a range of outdoor spaces such as sporting stadia, children’s playgrounds, patrolled beaches and bus stops. As public awareness of the risks of ETS has increased and the introduction of smoke free public spaces has become the norm, the number of smoke free homes has increased. However, among disadvantaged groups, exposure to ETS remains high, particularly for children from low socioeconomic groups12 and Aboriginal and Torres Strait Islander children. Actions 6.7.1 Continue to monitor and enforce existing smokefree legislation. Responsibility: State and Territory Governments Cancer Council Victoria and Quit Victoria support the proposed measure 6.7.1. We urge state and territory governments to ensure adequate, ongoing support is provided to the relevant enforcement agencies to improve educational, monitoring and enforcement activities under smokefree legislation, particularly given the increase in the number of smokefree laws in South Australian government has announced an intention to ‘phase-in’ smoking bans in any outdoor area provided for the consumption of food/and or drink purchased onsite by 2016 NSW government has announced an intention to implement smoking prohibitions in commercial outdoor dining areas by 2015. 1 54 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Australian states and territories in more recent times and under the previous National Tobacco Strategy 2004-09. Some enforcement agencies are not well resourced to carry out robust educational, monitoring and enforcement programs, thus ongoing support to these agencies (e.g. though service agreements) will provide for adequate enforcement officers, and will support appropriate prosecutions under smokefree law, for which in Victoria for example, there have been very few. 6.7.2 Strengthen partnerships between – state and territory and local governments to enhance the promotion, monitoring and enforcement of smokefree laws. Responsibility: State and Territory Governments; Local Governments. Cancer Council Victoria and Quit Victoria support the proposed measure 6.7.2 and refer to comments made in Action area 6.7.1 above, whereby enforcement agencies’ educational, monitoring and enforcement activity would be enhanced through ongoing partnership and support through state and territory governments. In Victoria and NSW, health groups have established projects that engage with local governments to promote and encourage implementation of smokefree local laws in public outdoor areas in the absence of state and territory legislation. These projects have seen an increase in the number of local governments implementing smokefree outdoor area local laws. 13 14 However state and territory legislation banning smoking in outdoor areas* would ultimately ensure a consistent approach across each jurisdiction. *Refer to Action area 6.7.7 for further detail on ‘outdoor areas’. 6.7.3 Ensure all publicly funded health services, community and social sector services and drug treatment agencies have comprehensive smokefree policies in place. Responsibility: State and Territory Governments; Australian Government; Local governments Cancer Council Victoria and Quit Victoria support the proposed measure 6.7.3. We have made suggested edits to the wording of the Action (as marked above) and refer to comments below, and in Action area 6.4.6. 55 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Smokefree environments afford protection from secondhand smoke exposure 15 16 and provide an environment conducive to reducing consumption and/or making a quit attempt.17 18 19 20 21 22 Funding agreements between health service/s, community/social sector and drug treatment agencies and the respective government should stipulate the establishment of a smokefree policy for the service/s. The funding agreement should include provisions for the service/s to implement, maintain, enforce and evaluate the smokefree policy. Quit Victoria would recommend the National Tobacco Strategy nominate a date for Action area 6.7.3, by which all publicly funded health services, community/social sector and drug treatment agencies should be required to have a smokefree policy in place. 6.7.4 Consider and develop approaches* that reduce children’s exposure to environmental tobacco smoke in their homes and develop policy that reduces children’s exposure to environmental tobacco smoke when travelling as passengers in cars. Responsibility: State and Territory governments; Australian Government Cancer Council Victoria and Quit Victoria proposed measure 6.7.4 and makes suggested edits to the wording of Action 6.7.4 as marked above. We recommend the immediate development of legislation to reduce children’s exposure to tobacco smoke when travelling in cars, in jurisdictions where legislation does not currently exist. In Australia, smoking inside the home has declined over time, as more households have become smokefree and as a greater proportion of smokers opt to smoke outdoors at home.23 However children, particularly those living in the most disadvantaged households are still exposed to secondhand smoke in the home.24 We support consideration and exploration of appropriate approaches to reduce smoking in homes. In addition to this, it is important for governments to continue to promote and implement smokefree policy in public areas, so as to reduce the number of environments where children may be exposed to secondhand smoke. Furthermore, a greater number of smokefree public places and workplaces has been associated with an increasing number of smokefree homes; a beneficial ‘flow-on effect’ of these policies. 25 26 *NB. Given the complexity of developing ‘policy’ in relation to reducing children’s exposure to tobacco smoke in the home, we would recommend the consideration/exploration and development of ‘approaches’, that reduce children’s exposure to tobacco smoke in the home, as a more feasible and appropriate action. 56 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 6.7.5 Enforce existing smokefree legislation and work towards all workplaces being smokefree (including outdoor areas in restaurants and hotels, near the entrances to buildings and air conditioning intake points, and in workplace vehicles). Responsibility: State and Territory Governments. Cancer Council Victoria and Quit Victoria supports the recommendation 6.7.5 to enforce existing smokefree legislation and refer to comments made in above Actions 6.7.1 and 6.7.2. The Preventative Health Taskforce technical report on tobacco proposes action to “review and if necessary amend state and territory legislation to cover the loose ends and address loopholes” in order to eliminate exposure to environmental tobacco smoke indoors and at other public areas.27 We recommend that Action 6.7.5 of the National Tobacco Strategy stipulates the removal of exemptions under state and territory smokefree law, which currently allow for smoking in certain workplaces. The removal of exemptions should capture in particular, but not necessarily be limited to, casino high roller rooms and gaming rooms, for which exemptions exist in some states and territories. It is unacceptable that staff in high roller rooms continue to be exposed to secondhand tobacco smoke. Workers in these settings should be afforded the same protection as staff of smokefree workplaces. We urge Action area 6.7.5 to call for an agreed date by which all states and territories must remove exemptions for high roller rooms. Alternatively, the Australian Government can act under Commonwealth law to prohibit smoking in these workplaces. Setting a date by which to enact/amend legislation would ensure a uniform approach across the country and would negate any argument of advantage of one state/territory over another. Cancer Council Victoria and Quit Victoria would recommend under Action 6.7.5, the development and adoption of smokefree legislation by states and territories as a matter of priority, for workplace vehicles, as an extension of existing smokefree workplace laws. Given the potential for smoke to accumulate in an outdoor area, particularly so where overhead coverings are in place and as the number of ignited cigarettes in the area increases,28 29 30 31 smokefree outdoor areas in restaurants and hotels, entrances to public buildings and near air conditioning intake points should also be nominated as a policy priority in order to prevent smoke accumulating at these areas and/or potentially drifting in to enclosed smokefree areas. 57 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Cancer Council Victoria and Quit Victoria recommend the National Tobacco Strategy nominate a date of ‘end-2014’ by which Australian states and territories should implement smokefree outdoor areas in restaurants and hotels. To date, Victoria remains the only jurisdiction yet to either legislate (QLD, ACT, WA, TAS, NT) or announce an intention to legislate (NSW, SA) smokefree outdoor areas in dining and drinking premises. 6.7.6 Complement legislative approaches to remaining smokefree workplaces with efforts to support employees and employers to quit smoking. Responsibility: State and Territory Governments Cancer Council Victoria and Quit Victoria support the proposed measure 6.7.6. and recommend the Action area also seeks the participation of non-government organisations to achieve this Action. Complementary workplace programs should include provision of: a) Training of staff to deliver one-to-one/brief interventions (e.g. training an OHS representative), b) Cessation support for employees/ers in the form of referral to Quitline and other cessation services, and; c) Communication to raise awareness among staff of the availability of subsidised NRT and other pharmacotherapies as effective mechanisms to manage cravings whilst quitting. 6.7.7 Encourage adoption of policies that restrict smoking outdoors where people gather or move in close proximity. For example, commercial outdoor eating areas; public playgrounds; public swimming pools and public recreation centres; sporting stadia, at public sports grounds; enclosed or covered bus stops and taxi ranks; near entrances to public buildings etc. Responsibility: State and Territory governments Cancer Council Victoria and Quit Victoria supports action 6.7.7 and urges the adoption of these policies by State and Territory Governments as a matter of priority. We recommend that the adoption of smoking restrictions in ‘commercial outdoor eating areas’ should be moved to Action area 6.7.5 to be consistent with proposed extensions to workplace smoking restrictions. 58 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Further to the comments made in Section 6.7.5, the adoption of smokefree policies help to further protect the public from secondhand smoke exposure and to denormalise smoking, which is particularly relevant for young people and children.32 We recommend that Action area 6.7.7 also articulate that relevant states and territories encourage the adoption of smokefree policy in the following areas (where these are yet to be implemented by relevant states and territories): on school grounds/premises at public/pedestrian malls at public outdoor events, including outdoor ‘youth events’ (i.e. events predominantly organised, intended for and attended by persons less than 18 years of age) between the flags at patrolled beaches 6.7.8 Consider and develop options to reduce exposure of residents to smoke drift in multi-unit developments. Responsibility: State and Territory Governments Cancer Council Victoria and Quit Victoria support the proposed Action 6.7.8. We recognise the absence of specific legislation protecting residents in multi-unit developments from exposure to smoke drift. However in NSW, a tribunal held that owners’ corporations can establish by-laws to prohibit smoking33. We recommend action from state and territory governments to: a) increase community awareness about the options available to residents in multi-unit developments that are owners’ corporations to prohibit smoking within the complex; and b) to provide prospective owners of lots in planned multi dwelling developments with information about achieving a smokefree development. The information would detail how an owners’ corporation committee could incorporate a bylaw prohibiting smoking within the private and common areas of a complex. This information would include: c) template by-laws with information about the procedures for incorporating new bylaws; 59 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 d) the processes for managing non-compliance; and e) in the event of continued non-compliance, enforcing the by-law through the legal system. Owners’ corporations are regulated by State and Territory government laws. Accordingly, State and Territory governments would be responsible for preparing and disseminating this information. 1 IARC Working Group on the Evaluation of the Effectiveness of Smoke-free Policies. Evaluating the effectiveness of smoke-free policies. IARC Handbooks of Cancer Prevention, Tobacco Control. Lyon, France: International Agency for Research on Cancer, 2009. Available from: International Agency for Research on Cancer website 2 Eureka Strategic Research. Youth tobacco prevention research project. Canberra: 2005. June 2005. [viewed 22 June 2012]. Available from: Department of Health and Ageing website 3 Smart R and Stoduto G. Interventions by students in friends' alcohol, tobacco, and drug use. Journal of Drug Education 1997;27:213-22. Available from: National Center for Biotechnology Information website 4 Wood L, Lang A and Coase P. Smarter than Smoking Qualitative Research. A research report. West Perth, Australia: TNS Social Research, 2005. 5 IARC Working Group on the Evaluation of the Effectiveness of Smoke-free Policies. Evaluating the effectiveness of smoke-free policies. IARC Handbooks of Cancer Prevention, Tobacco Control. Lyon, France: International Agency for Research on Cancer, 2009. Available from International Agency for Research on Cancer 6 Smart R and Stoduto G. Interventions by students in friends' alcohol, tobacco, and drug use. Journal of Drug Education 1997;27:213-22. Available from: National Center for Biotechnology Information website 7 Wakefield MA, Chaloupka FJ, Kaufman NJ, Orleans CT, Barker DC, and Ruel EE. Effect of restrictions on smoking at home, at school, and in public places on teenage smoking: cross sectional study. BMJ. 2000;321(7257):333-7. Available from: National Center for Biotechnology Information website 8 Winstanley M, and Wood L. Chapter 5. Factors influencing the uptake and prevention of smoking. Tobacco in Australia: Facts and Issues. Third Edition. Melbourne: Cancer Council Victoria; 2008 [cited 20 June 2012]. Available from: Tobacco in Australia website 9 Pierce JP, and Leon M. Effectiveness of smoke-free policies. Lancet Oncol. 2008;9(7):614-5. Available from: National Center for Biotechnology Information website 10 Scollo M, Lal A, Hyland A, and Glantz S. Review of the quality of studies on the economic effects of smokefree policies on the hospitality industry. Tob Control. 2003;12(1):13-20. Available from: National Center for Biotechnology Information website 11 Eriksen M and Chaloupka F. The economic impact of clean indoor air laws. CA: A Cancer Journal for Clinicians 2007;57(6):367–78. Available from: http://caonline.amcancersoc.org/cgi/content/abstract/57/6/367(This website link was valid at the time of submission) 60 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 12 Gartner CE, and Hall WD. Is the socioeconomic gap in childhood exposure to secondhand smoke widening or narrowing? Tobacco Control. 2012; [Epub ahead of print]. Available from: National Center for Biotechnology Information website 13 Heart Foundation, and Quit Victoria. Smoke-free policies in outdoor areas: a resource kit for Victorian local governments. Melbourne, Australia: Heart Foundation and Quit Victoria, 2010. Available from: Quit Victoria website 14 Heart Foundation. Smoke-free policy in outdoor areas. Sydney, Australia: National Heart Foundation of Australia, 2011. Available from: Heart Foundation website 15 IARC Working Group on the Evaluation of the Effectiveness of Smoke-free Policies. Evaluating the effectiveness of smoke-free policies. IARC Handbooks of Cancer Prevention, Tobacco Control. Lyon, France: International Agency for Research on Cancer, 2009. Available from: International Agency for Research on Cancer website 16 Pickett MS, Schober SE, Brody DJ, Curtin LR and Giovino GA. Smoke-free laws and secondhand smoke exposure in US non-smoking adults, 1999-2002. Tob Control, 2006. 15(4):302-307. Available from: Tobacco Control website 17 Albers AB, Siegel M, Cheng DM, Biener L, and Rigotti NA. Effect of smoking regulations in local restaurants on smokers' anti-smoking attitudes and quitting behaviours. Tobacco control. 2007;16(2):101-6. Available from: National Center for Biotechnology Information website 18 Farkas AJ, Gilpin EA, Distefan JM and Pierce JP. The effects of household and workplace smoking restrictions on quitting behaviours. Tob Control, 1999. 8(3):261-265. Available from: Tobacco Control website 19 Fong GT, Hyland A, Borland R, Hammond D, Hastings G, McNeill A et al. Reductions in tobacco smoke pollution and increases in support for smoke-free public places following the implementation of comprehensive smoke-free workplace legislation in the Republic of Ireland: findings from the ITC Ireland/UK Survey. Tob Control, 2006. 15(suppl_3):iii51-58. Available from: Tobacco Control website 20 Siahpush M, Borland R and Scollo M. Factors associated with smoking cessation in a national sample of Australians. Nicotine Tob Res, 2003. 5(4):597-602. Available from: Nicotine and Tobacco Research, Oxford Journals 21 Chapman S, Borland R, Scollo M, Brownson RC, Dominello A and Woodward S. The impact of smoke-free workplaces on declining cigarette consumption in Australia and the United States. Am J Public Health, 1999. 89(7):1018-23. Available from: American Journal of Public Health website 22 Fichtenberg CM and Glantz SA. Effect of smoke-free workplaces on smoking behaviour: systematic review.[see comment]. BMJ, 2002. 325(7357):188. Available from: BMJ website 23 Gartner CE, and Hall WD. Is the socioeconomic gap in childhood exposure to secondhand smoke widening or narrowing? Tobacco Control. 2012; [Epub ahead of print]. Available from: National Center for Biotechnology Information website 24 Gartner CE, and Hall WD. Is the socioeconomic gap in childhood exposure to secondhand smoke widening or narrowing? Tobacco Control. 2012; [Epub ahead of print]. Available from: National Center for Biotechnology Information website 25 IARC Handbooks of Cancer Prevention Tobacco Control. Chapter 4. Impact of smoke-free policies on businesses, the hospitality sector, and other incidental outcomes. In: Evaluating the effectiveness of smoke-free policies. Lyon, France: International Agency for Research on Cancer, 2009. Available from: http://com.iarc.fr/en/publications/pdfs-online/prev/handbook13/(This website link was valid at the time of submission) 61 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 26 Borland R, Yong HH, Cummings KM, Hyland A, Anderson S and Fong GT. Determinants and consequences of smoke-free homes: findings from the International Tobacco Control (ITC) Four Country Survey. Tobacco Tobacco Control website 27 Australian Government, Preventative Health Taskforce. Australia: the healthiest country by 2020. Technical Report 2. Tobacco control in Australia: making smoking history. Canberra: Commonwealth of Australia, 2009. Available from: Department of Health and Ageing website 28 Brennan E, Cameron M, Warne C, Durkin S, Borland R, Travers MJ, et al. Secondhand smoke drift: examining the influence of indoor smoking bans on indoor and outdoor air quality at pubs and bars. Nicotine Tob Res. 2010;12(3):271-7. Available from: National Center for Biotechnology Information website 29 Klepeis N, Ott W, and Switzer P. Real-time measurement of outdoor tobacco smoke particles. J Air Waste Manag Assoc. 2007;57(5):522–34. Available from: Action on Smoking and Health website 30 Cameron M, Brennan E, Durkin S, Borland R, Travers MJ, Hyland A, et al. Secondhand smoke exposure (PM2.5) in outdoor dining areas and its correlates. Tob Control. 2010;19(1):19-23. Available from: National Center for Biotechnology Information website 31 Wilson N, Edwards R, and Parry R. A persisting secondhand smoke hazard in urban public places: results from fine particulate (PM2.5) air sampling. The New Zealand Medical Journal. 2011;124(1330):34-46. Available from: The New Zealand Medical Journal website 32 Wakefield MA, Chaloupka FJ, Kaufman NJ, Orleans CT, Barker DC, and Ruel EE. Effect of restrictions on smoking at home, at school, and in public places on teenage smoking: cross sectional study. BMJ. 2000;321(7257):333-7. Available from: National Center for Biotechnology Information website 33 Owners Corporation SP 49822 v May & Ors (Strata & Community Schemes) [2006] NSW Consumer, Trader and Tenancy Tribunal 739 62 6.8 Provide access to a range of evidence based cessation services to support smokers to quit 6.8.1 Increase the availability and range of Quitline and other cessation support, particularly for disadvantaged groups and people receiving specialist treatment for chronic health conditions. Responsibility: State and Territory governments; non-government organisations; Quitline services. As discussed in 6.4 there have been many recent developments in developing tailored cessation support for disadvantaged people, particularly through the CCNSW tackling tobacco program. Quit strongly advocates for national collaboration on the development of smoking cessation projects/programs for disadvantaged/vulnerable smokers in an effort to develop best practise, evidence based activity that is shared across jurisdictions. Quit Victoria identifies the need for a national coordination role for this activity. 6.8.2 Enhance Quitline services for pregnant women (in particular Aboriginal and Torres Strait Islander women) including call back services and feedback to obstetricians, GPs and midwives and Aboriginal health workers. Responsibility: State and Territory governments; non-government organisations; Quitline/Multilingual Quitline services. Agree. It is estimated that 16% of pregnant women in Australia currently smoke, and as stopping or reducing smoking is one of the few preventable risk factors associated with a range of poor birth outcomes for the baby1. Multifaceted smoking cessation interventions are effective at reducing the number of women who smoke while pregnant by approximately 6% overall 2. Repeated cessation support and advice via Quitline that is tailored to pregnant women has been shown to be effective in reducing smoking among this group3. Continuing to enhance Quitline services, promote and integrate brief intervention including routine referral to Quitline by GP’s, midwives and maternal and child health workers can lead to a reduction in the prevalence of smoking in pregnancy. To illustrate in Victoria, fax referrals to the Quitline made by midwives in 2009, increased by 430% from 2008 figures. While it is important to note that midwife fax referral figures were low in 2008, this dramatic increase highlights that this approach of training, support and engagement assists midwives to deliver smoking cessation intervention to their clients. In subsequent years fax referrals made by Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 midwives and maternal and child health nurses have continued to increase by an average of 65% per year. Quit Victoria recognises and reinforces the value of not only enhancing Quitline services but working with the maternity care sector is essential in providing optimal support to pregnant women who smoke. 6.8.3 Enhance Aboriginal-specific Quitline services including call back services and feedback to Aboriginal health workers. Responsibility: State and Territory governments; non-government organisations; Quitline/Multilingual Quitline and other cessation services Agree with expansion of responsibility to include other cessation support services. Currently all jurisdictions are funded to enhance Quitline services to support ATSI persons (funding for Quitline Victoria’s dedicated Aboriginal counsellors will cease in 2015. A scoping paper conducted by Cancer Institute NSW to review the appropriateness of Quitline service for ATSI people living in NSW found that there was a high level of awareness of the service, and recognition that the service could provide access for ATSI people, but very low levels of uptake. Further work need to be done to • Develop cultural competencies within existing Quitline workforce • Continue to develop skills in ATSI people working within or promoting Quitline services • Develop routine referral mechanisms for Aboriginal health services into Quitlines • Integrate Quitline referral into routine care for aboriginal health workers and workers within other services supporting ATSI people • Enhance feedback mechanisms for referrers to promote co-management • Raise awareness of Quitline services for ATSI people employing targeted social marketing approaches. 6.8.4 Continue to promote Quitline services to smokers and the community through mass media campaigns and other communication channels. Responsibility: Australian Government; State and Territory governments, nongovernment organisations and Quitline and other cessation support services. 64 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Agree with expansion of responsibility to include other cessation support services. Anti-smoking television campaigns remain one of three main interventions (with tobacco taxation and legislative reform) to reduce population smoking rates both in Australia and internationally. Currently the Quitline number appears at the end of all social marketing television campaigns in Victoria and is a primary referral source, with 27% of all callers becoming aware of, and contacting the service after seeing the television campaigns 4. 6.8.5 Increase the range of web based programs provided as part of Quitline services to provide greater opportunities to interact with smokers and encourage them to quit and ensure the information is regularly updated to reflect best practice. Responsibility: State and Territory governments; non-government organisations; Quitline services. Quit Victoria supports the development of digital based cessation support. There is emerging efficacy of cessation support delivered through web based programs. An example of which is the QuitCoach and onQ SMS tools developed in Victoria by Professor Ron Borland5. Since late 2010, Quit Victoria has greatly improved and expanded information and support tools for smokers through its website Quit Victoria website which has increased unique visitor traffic substantially. Average monthly usage for the visitors for the first quarter of 2012 was 30,567 unique visitors per month. This is compared with 17,242 unique visitors for the last quarter of 2010, prior to relaunching www.quit.org.au6. Quit Victoria endorses further development and recommends this action item be expanded to include the evaluation of these digital activity in both attracting and engaging smokers in ecessation as well as assessing the effectiveness to change smoking behaviours (eg delay to first cigarette, quit attempts, reduced consumption, successfully quit, etc). Quit Victoria recommends national coordination and collaboration on the development of new digital programs to maximise resources and avoid duplication. 6.8.6 Improve the integration of Quitline programs across the health system, primary care services and relevant non-government organisations with a priority focus on low socio-economic and disadvantaged groups. 65 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Responsibility: State and Territory governments; Australian Government; nongovernment organisations; Quitline services; health services. Quit Victoria agrees with proposed action 6.8.6. Noting the addition of “other cessation programs” to read “Improve the integration of Quitline and other cessation programs with other programs across the health system, primary care services and relevant non-government organisations with a priority focus on low socioeconomic and disadvantaged groups”. Responsibility should be broadened to include Australian Government and non-government organisations. Integration and routine referral to Quitline should be a component of all integrated approaches within other programs across the health and community services system. Opportunities for increased referral of vulnerable smokers by social service organisations should be explored. The National Drug and Alcohol Research Centre (NDARC) is currently involved in developing a study to assess the effectiveness of generating referrals to Quitline from Centrelink for smoking clients on financial assistance. 6.8.7 Develop systems that encourage health professionals to routinely ask patients about their smoking status and provide smokers with appropriate advice and support to quit, including appropriate referral to specialist cessation services. Responsibility: State and Territory government; Australian Government Agreed with the expansion of the Action to include further integration of cessation support and routine referrals into existing primary health care systems as follows: “Explore and develop systems that integrate brief intervention and routine referral into primary health care settings and the systems (i.e. Medical Director) that support them. Encourage health professionals to routinely ask (and record) patients about their smoking status and accordingly provide smokers with appropriate advice and support to quit, including appropriate referral to specialist cessation services.” 6.8.8 Improve management of smoking patients in healthcare facilities, particularly for patients on admission to hospital. Responsibility: State and Territory government health services. 66 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 Agree with expansion of responsibility to include Australian government and nongovernment organisations and modification of the Action to read as follows: “Improve management patients in health care facilities, particularly for patients on admission to hospital. Providing access to smoking cessation support, routine referral and NRT access”. The evidence suggests that for many people a health event is the time when they are motivated to attempt to address their smoking7. Providing routine brief intervention, access to NRT and cessation support and routine referral to Quitline for all patients admitted into healthcare facilities would provide many smokers with additional support to address smoking. 6.8.9 Provide policy guidelines and training in best practice smoking cessation (particularly brief interventions) to a range of health professionals, health, community and welfare workers and ensure these are regularly updated to reflect best practice. Responsibility: State and Territory governments; non-government organisations; Quitline services; health and community services; community controlled Aboriginal Medical Services; Australian Government. Agree with expansion of Action to include community services. Organisations and individual services may vary in the type and intensity of smoking cessation they provide and therefore it may be important to establish a recommended minimum care model. This would need to be created in consultation with sector representatives, but as a guide it should include: Routine assessment and recording of smoking status Provision of brief advice and encouragement to quit as part of usual casework Referral to other quit support services (including staff access to quit lines during working hours) Organisational smokefree policy development and implementation. Services with ongoing contact with vulnerable smokers provide the opportunity to provide regular support and multiple quit attempts over time. Quit Victoria also advocates for a 67 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 collaborative approach to smoking cessation to ensure a consistent approach across jurisdictions to enhance opportunities for knowledge sharing. Quit Victoria projects with a homeless persons program and an Aboriginal youth mentoring program has found that many support workers don’t feel empowered to discuss tobacco with their clients. In both of these instances brief intervention training and development of Quitline referral pathways has led to increased confidence in talking to clients about smoking. 6.8.10 Provide policy guidelines and training in brief interventions to social service organisations who are already working with highly disadvantaged groups to build their capacity to support quit attempts in these groups, including by appropriate referral and ensure these are regularly updated to reflect best practice. Responsibility: State and Territory governments; non-government organisations; social service organisations; Quitline services; Australian Government. Agree. With reference to 6.8.10 organisations working with these populations can be encouraged to integrate into their existing service provision model. A process of consultation and engagement could be adopted to enable smoking cessation expertise to support the adopting of localised solutions rather than imposing a model on services. 6.8.11 Increase awareness among relevant organisations and disadvantaged groups of the availability of subsidised nicotine replacement therapies. Responsibility: State and Territory governments; Australian Government; nongovernment organisations; Quitline services; health and community services; community controlled Aboriginal Medical Services; social service organisations. Agree with the expansion of the responsibility to include community services. Following the announcement of the PBS subsidy for nicotine patches from February 2011, Quit Victoria and Quitline Victoria received an abundance of calls from health care sector workers and smokers to find out how subsidised products could be accessed, and what products were subsidised. Quit Victoria believes a level of confusion and low awareness still exists, particularly among the social support sector. For example, as part of Quit’s homeless persons project, it has 68 Quit Victoria and Cancer Council Victoria Submission: Draft for Consultation of the National Tobacco Strategy 2012 - 2018 June 25, 2012 become apparent that barriers exist for disadvantaged populations, where some general practitioners either refused to prescribe NRT for smoking clients as part of the study, citing a disbelief in the efficacy of NRT supporting smoking cessation in this client group, or were unaware of it being available on the PBS. 6.8.12 Improve appropriate use of pharmacotherapies and services demonstrated to assist with smoking cessation especially among disadvantaged groups. Responsibility: Australian Government, State and Territory governments; non-government organisations; Quitline services. Agree. NRT and other pharmacotherapies have been proven to be effective in supporting successful quit attempts, and can be particularly useful for clients for whom there are additional barriers to quitting8. However this access should be combined with options for other effective cessation supports. NRT and other pharmacotherapies are useful in assisting clients to deal with nicotine withdrawal but the habitual and psychological aspects of addiction are able to be addressed though face to face or Quitline support. Quit would suggest that all disadvantaged and vulnerable clients accessing or being prescribed NRT or other pharmacotherapies also receive at a minimum routine referral to Quitline. 1 Scollo MM, Winstanley, MH (ed). Tobacco in Australia: Facts and Issues. Third ed. Melbourne: Cancer Council Victoria; 2008. Available from: http://www.tobaccoinaustralia.org.au/ 2 Lumley J, Chamberlain C, Dowsell T, Oliver S, Oakley L and Watson L. Interventions for promoting smoking cessation during pregnancy. Cochrane Database Systematic Review 2009(3):CD001055. Available from: National Center for Biotechnology Information website 3 Dennis C and Kingston D. A systematic review of telephone support for women during pregnancy and the early postpartum period. Journal of Obstetric, Gynecologic, and Neonatal Nursing 2008;37(3):301–14. Available from: Wiley Online Library website 4 Quitline Victoria – Monthly Reports – Source of Calls 2011 and 2012. 5 Borland R, Balmford J & Hunt D. The effectiveness of personally tailored computer-generated advice letters for smoking cessation. Addiction. 2004; 99: 369-377 6 Quit Victoria website Monthly Google Analytics Reports, 2012 7 Lindorff KJ. Tobacco time for action: National Aboriginal and Torres Strait Islander Tobacco Control Project final report. Canberra: National Aboriginal Community Controlled Organisations, 2002. Available from: http://www.naccho.org.au/Files/Documents/NACCHO_Tobacco_report.pdf (This website link was valid at the time of submission) 8 Scollo MM, Winstanley, MH (ed). Tobacco in Australia: Facts and Issues. Third ed. Melbourne: Cancer Council Victoria; 2008. Available from: Tobacco in Australia website 69 Part Three – Monitoring Progress Cancer Council Victoria and Quit Victoria endorse the position in the draft Strategy that monitoring the implementation of the strategy will require a co-ordinated national effort. Data collection and analysis, and policy and program monitoring and evaluation are currently undertaken across a range of jurisdictions and by both government and non-government organisations. We believe co-ordination of this activity requires the establishment of a specific monitoring sub-committee of the Standing Committee on Tobacco and this sub-committee should comprise members with research expertise from federal government, state and territory government and state and territory NGOs where these organisations play a lead role in monitoring tobacco control progress. These experts should be identified and consulted prior to the Strategy being finalised to ensure the feasibility and value of collecting data against the outcome indicators contained in the draft Strategy. These experts may not necessarily work in tobacco control, for example is important that staff of the Australian Institute of Health and Welfare who collect data for the National Drug Strategy Household Survey are involved. In Victoria, the Centre for Behavioural Research in Cancer and the International Tobacco Control Policy Evaluation Survey (ITC) at the Cancer Council Victoria both collect and analyse data that is relevant at the state and national level. Representatives of these agencies should be part of any sub-group established, as should agencies involved in similar work from each state and territory. Lastly we believe that with the heavy emphasis on supporting reduced smoking prevalence in priority/disadvantaged and Indigenous populations, greater attention must be given to developing data collection mechanisms and analysis of data to measure the impact of the Strategy within these populations. This may include developing data collection tools to be integrated into government services (for example Centrelink) and that can be used by funded health and social sector agencies.