RLF-Spinoreticulotha#9J5H#
advertisement

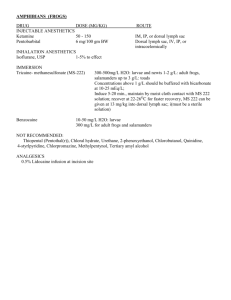
Spinoreticulothalamic Pathway – relays in the reticular formation of the brainstem Substantia gelatinosa - contacted by sensory afferents & reticulospinal fibers, especially raphe nucleus of medulla It synapses on tract cells of the spinothalamic tract. Spinothalamic fibers also synapse in posterior thalamus – to insula & parietal cortex sensory association area intralaminar – diffusely to frontal & parietal lobes, limbic areas & basal ganglia – consciousness, autonomic responses, movement mediodorsal – frontal lobe thought areas Pain – Dorsal column/medial lemniscus central processes have collaterals that synapse with substantia gelatinosa, making it inhibit the tract cells for pain This inhibition can be overcome with a strong nociceptive input Transection of the ventral lateral area of the spinal cord results in almost complete loss of pain sensations on the opposite side of the body below the lesion, but sensibility gradually returns, because of alternative pathways. Section of the ventral white commissure also causes prolonged analgesia Pain sensations after destruction of the postcentral gyrus is from spinothalamic & reticulothalamic afferents to intralaminar & mediodorsal thalamic nuclei that connect with the neocortex, as above. Raphe nuclei release serotonin into the substantia gelatinosa. The periaqueductal gray area stimulates the raphe nucleus Opioid receptors are on the dorsal horn, raphe nucleus, periaqueductal gray nuclei ALS - A-delta fast pain pathwy 1st order - in dorsal root ganglion, central process in lateral bundle synapses in lamina I, II, or V (nucleus proprius) of the dorsal horn of gray matter in the spinal cord http://cda.mrs.umn.edu/~meeklesr/p19.jpg 2nd order dorsal horn axons cross the midline in the spinal cord in the ventral white commissure, ascend in the ALS tract, and synapse at the VPL nucleus of the thalamus like the dorsal column pathway 3rd order - VPL axons travel to the postcentral gyrus From the face: 1st order - trigeminal ganglion In the central process, V1 fibers are dorsal, V3 are ventral, V2 are inbetween; they rotate as they enter so that in the spinal trigeminal tract, it’s the opposite. The most dorsal part of the tract has fibers from VII, IX, and X. 2nd order - spinal trigeminal nucleus: three different parts: pars caudalis - from pyramidal decussation to C3 - pain & temperature pars interpolaris - to inferior olivary nucleus - pain from teeth pars oralis - to chief sensory - mostly coarse touch; most superior part by chief sensory nucleus has discriminitive touch Included with all the pars is the adjacent reticular formation that functions like the dorsal root. processes from the 2nd order neuron cross the midline & travel through the ventral & dorsal trigeminothalamic tracts to the ventral posterior medial nucleus of the thalamus. VPM axons synapse in the post central gyrus slow pain - divergent pathway sensitized C fibers Pathway: Axons from the dorsal root ganglion (1st order neuron) in the lateral bundle of the dorsal root, a.k.a. dorsolateral fasciculus or Lissaur’s tract, synapses on many neurons (see gate theory below) in the dorsal horn of gray matter of the spinal cord, on the 2nd order neuron & interneurons: Lamina I - many pain fibers terminate here, contribute to ALS tract – Waldeyer cells Lamina II-III - substantia gelatinosa - interneurons that are stimulated by Adelta and C fibers and work in pain modulation Laminae IV-VI - nucleus proprius - ALS tract nucleus for light touch & pain, whose axon will cross the midline in the anterior white commissure, ascending 1-2 levels as it crosses, ascend on the opposite (contralateral) side in the anterolateral tract (aka spinal lemniscus) to synapse ...... in many places: - VPL of the thalamus (historically the 3rd order) to go to the post central gyrus of the cortex like the DCML pathway - reticular formation (where pain modulating pathways are stimulated) - interneurons in lamina I & II, transmitter is substance P, that synapse on nucleus proprius whose axons joint the tract and exit at: - midbrain - Spinomesencephalic tract - for eye, head & neck reflexes involving pain, tract cell synapses in superior colliculus for head & eye turning toward pain stimulus, and periaqueductal gray for pain modulation - reticular formation - Spinoreticulothalamic tract - slow pain, primarily from C fibers, tract cell collaterals synapse in the reticular formation of the brainstem, can also be involved in pain modulation, and eventually will synapse on the in the intralaminar nuclei of the thalamus to frontal & parietal lobes & striatum, mediodorsal to frontal lobe thought areas – evoke emotion and attention, sensory integration, affect personality, movementfrom the face - trigeminoreticulothalamic - to reticular formation and then intralaminar nuclei (temperature also goes to the reticular formation, thalamus, hypothalamus) Reticular formation pain modulation sites: Periaqueductal gray in midbrain - activates raphe nucleus Raphe Magnus nucleus in medulla - neurotransmitter is serotonin - axons go to spinal cord and synapse on the substantia gelatinosa that releases enkephalins Lateral tegmental nucleus in brainstem also is activated by PAG, which also stimulates substantia gelatinosa to release enkephalins Locus ceruleus in pons - also activated by PAG, releases norepinephrine to suppress the release of substance P at the primary pain afferent endings, collaterals inhibit raphe magnus Enkephalins (opioids) produce analgesia - block pain transmission: 1. by hyperpolarizing both presynaptic ending & post-synaptic neuron 2. block transmission -bind to receptors on presynaptic primary afferent fibers to block neurotransmitter release 3. receptors on PAG, raphe, dorsal horn nuclei Pain Modulation: Gate theory - developed by Melzack & Wall - edits painful sensations http://pirate.shu.edu/~vigorimi/Motivation_and_Emotion/Chapter%208.html (just the top diagram) the 1st order neuron synapses on in the dorsal horn many places: 1. tract cell - laminas I & nucleus proprius - axon crosses the midline at the ventral white commissure and continues on the opposite side of the spinal cord to the brain 2. excites interneuron to inhibit the gate neuron in the substantia gelatinosa (SG) (that inhibits pain - gate theory is below ) 3. interneurons to the tract 4. interneurons to ventral horn motor area neurons (reflex withdrawl) 5. interneurons to lateral horn (autonomic) neurons Collaterals from mechanoreceptors (i.e. dorsal column/medial lemniscus pathway 1st order neuron) excite gate interneurons of the SG whose axons release enkephalins (opioid) on the ALS tract cell &/or interneuron to the tract cell that is directly stimulated by the 1st order ALS neuron. (Substantia Gelatinosa also gets afferents from reticular formation) - at least 1/2 of lamina I & nucleus proprius tract cells get input from SG opioid interneurons - opioids reduce Ca+2 influx, hyperpolarize presynaptic endings to block pain transmission & hyperpolarize postsynaptic terminals to make pain transmission more difficult Levels of pain inhibition: 1 - non-narcotic analgesics decrease synthesis of prostaglandins 2 - dorsal horn local inhibition from non-nociceptive afferents 3 - periaqueductal gray descending pathways 4 - stress hormones released thru the H-P-A pathway 5 - cortex 6 - Exogenous opioids bind to periaqueductal gray, raphe, and dorsal horn neurons, inducing analgesia chronic pain - burning, throbbing, chronic - pain that lasts beyond the period of healing, relative absence of tissue destruction, excess nociceptor activity that outlasts the healing period - prostaglandins increase nociceptor excitability pain produces autonomic and motor reflexes – withdrawl reflex – crossed extensor reflex – a collateral of the central pain fiber synapses on an interneuron that synapses on interneurons that cause flexion (withdrawl) with inhibition of the antagonist on the ipsilateral side & extension (excitation of antagonist, inhibition of the flexor) on the contralateral side visceral pain - transmitted with sympathetic nerve fibers, poorly localized because of convergence, which can involve 2nd order anterolateral system neurons; injury can cause sympathetic axons to sprout & activate dorsal root ganglion cells referred pain - perceived in one area but initiated in a different area - due to convergence at the dermatome (diaphragm --> C3,4; heart -->left T1-4; stomach --> left T6-9; gall bladder R T7-8; appendix --> right T10; kidney --> Lumbar1-2); or brain interpretation The cortex perceives the sensation, and projects that sensation to an area of the body that may differ from the location of the stimulation, that has already perceived pain from a different modality. radicular pain - pain caused by activation of sensory fibers at the dorsal root - herniated disks are a good example phantom pain - pain from an amputated structure other definitions: hyperalgesia - increased sensitivity, lower threshold, of pain receptors, primary (? increased # of Na+ channels), or secondary (surrounding tissues become supersensitive), can be caused by lower pH analgesia - absence of pain in response to pain stimulation allodynia - pain from a stimulation that normally is not painful, also can be caused by lower pH neuralgia - pain in the distribution of a nerve threshold - stimulus necessary to initiate pathway tolerance - amount of pain one can tolerate pain also incorporates visceral and emotional responses - ’emotional, affective & arousal aspects of nociception (sensation of pain)’ Reflexes: 1,2 – S = calcaneous tendon & Babinski 3,4 – L = quadriceps 5,6 – C = biceps 6,7 – C= triceps 7,8 – C = brachioradialis