Module # 3 – Pulmonary Embolus / Deep Vein Thrombosis
advertisement
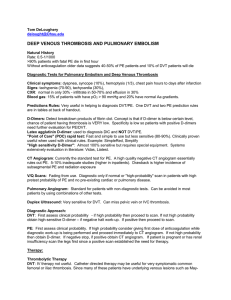
Facilitator Version Module # 3 – Pulmonary Embolus / Deep Vein Thrombosis Created by Taylor Goot, 2/14 Objectives: 1. 2. 3. 4. 5. Recognize the signs, symptoms, and risk factors of PE/DVT. Be familiar with scoring systems used in assessing pre-test probability (Wells). Identify appropriate diagnostic modality based on clinical scenario. Be familiar with different therapeutic options available and their use. Be able to recognize and appropriately treat cardiovascular collapse in the setting of APE. References: Ageno, W., Gallus, A. S., Wittkowsky, A., Crowther, M., Hylek, E. M., Palareti, G., et al. (2012). Oral anticoagulant therapy: Antithrombotic therapy and prevention of thrombosis, 9th ed: American college of chest physicians evidence-based clinical practice guidelines. Chest, 141(2 Suppl), e44S-88S. Aujesky, D., Roy, P. M., Verschuren, F., Righini, M., Osterwalder, J., Egloff, M., et al. (2011). Outpatient versus inpatient treatment for patients with acute pulmonary embolism: An international, open-label, randomised, non-inferiority trial. Lancet, 378(9785), 41-48. Bates, S. M., Jaeschke, R., Stevens, S. M., Goodacre, S., Wells, P. S., Stevenson, M. D., et al. (2012). Diagnosis of DVT: Antithrombotic therapy and prevention of thrombosis, 9th ed: American college of chest physicians evidence-based clinical practice guidelines. Chest, 141(2 Suppl), e351S-418S. Garcia, D. A., Baglin, T. P., Weitz, J. I., Samama, M. M., & American College of Chest Physicians. (2012). Parenteral anticoagulants: Antithrombotic therapy and prevention of thrombosis, 9th ed: American college of chest physicians evidence-based clinical practice guidelines. Chest, 141(2 Suppl), e24S-43S. Kearon, C., Akl, E. A., Comerota, A. J., Prandoni, P., Bounameaux, H., Goldhaber, S. Z., et al. (2012). Antithrombotic therapy for VTE disease: Antithrombotic therapy and prevention of thrombosis, 9th ed: American college of chest physicians evidence-based clinical practice guidelines. Chest, 141(2 Suppl), e419S-94S. Mercat, A., Diehl, J. L., Meyer, G., Teboul, J. L., & Sors, H. (1999). Hemodynamic effects of fluid loading in acute massive pulmonary embolism. Critical Care Medicine, 27(3), 540-544. Wells, P. S., Owen, C., Doucette, S., Fergusson, D., & Tran, H. (2006). Does this patient have deep vein thrombosis? JAMA : The Journal of the American Medical Association, 295(2), 199-207. Zondag, W., Mos, I. C., Creemers-Schild, D., Hoogerbrugge, A. D., Dekkers, O. M., Dolsma, J., et al. (2011). Outpatient treatment in patients with acute pulmonary embolism: The hestia study. Journal of Thrombosis and Haemostasis : JTH, 9(8), 1500-1507. Zondag, W., Mos, I. C., Creemers-Schild, D., Hoogerbrugge, A. D., Dekkers, O. M., Dolsma, J., et al. (2011). Outpatient treatment in patients with acute pulmonary embolism: The hestia study. Journal of Thrombosis and Haemostasis : JTH, 9(8), 1500-1507. Stein, P. D., Beemath, A., Matta, F., Weg, J. G., Yusen, R. D., Hales, C. A., et al. (2007). Clinical characteristics of patients with acute pulmonary embolism: Data from PIOPED II. The American Journal of Medicine, 120(10), 871-879. Uptodate.com “Approach to the diagnosis and therapy of lower extremity deep vein thrombosis” “Diagnosis of acute pulmonary embolism” “Treatment of acute pulmonary embolism” “Fibrinolytic (thrombolytic) therapy in acute pulmonary embolism and lower extremity deep vein thrombosis” Case: A 57 yo male with a PMH of diabetes, HTN, and HLD presents to the emergency department with a chief complaint of LLE cramping. He first noted cramping in the back of his left calf. He states that it has been increasing in severity and that there may now be some swelling. VS: T 37.1C HR 72 BP 143/71 SpO2 93% on Room air. BMI 33. PE: Obese male, LLE is slightly enlarged, erythematous, with pitting edema at the ankle. Skin is tender with increased warmth. Pulses are intact. Labs: BMP and CBC are without abnormality. You suspect the patient has a deep vein thrombosis (DVT), prior to any diagnostic study, what historical points would you like to cover? (i.e. risk factors, signs/symptoms) - Any history of prolonged immobilization (illness, injury, stroke, travel) Recent surgical procedures Trauma Previous VTE Malignancy - Females: oral contraceptives, hormone therapy, pregnancy Family history Rheumatologic disease or medications (hydralazine) that may raise suspicion for antiphospholipid antibody What diagnostic study would you use to confirm your diagnosis? LE ultrasound; D-dimer, and probability scoring to be discussed later in case. OPTIONAL: Diagnostic algorithm is more complicated: In moderate/high prob cases if only proximal (vs whole leg) US is done and is negative, study should be repeated in one week OR d-dimer should be sent. If dimer is negative, no further testing, if dimer is positive, repeat prox US in one week. At UNM whole leg US is done thereby avoiding these scenarios. Diagnosis of LLE DVT is confirmed, therapy is started and patient is discharged after an uneventful and brief hospital stay. Case continued: 3 years later the same gentleman presents to the ED with a chief complaint of chest pain. He reports onset about 24hours ago. The sensation is continuous left sided, stabbing in nature, has been gradually worsening over time. Upon questioning he does note an increase in pain when taking a deep breath, but denies cough or shortness of breath. VS: T 36.7 HR 95 BP 147/76 RR 14 SpO2 92% on room air, HT 170cm WT 80kg PE: NAD, lungs clear to auscultation, you do note some increased discomfort when patient is asked for a deep inspiration. LE exam reveals no evidence of previous swelling, no erythema, pulses intact. CXR: Heart appropriate size. No parenchymal opacity. Left costrophrenic angle is slightly blunted. EKG: Non-specific ST changes in the inferior leads Labs: CBC: WBC 10.7 HH 13/41 PLT 230 Chem 7: Electrolytes WNL, Cr of 1.5 (at baseline) INR 1.01 Further history reveals that the patient completed 6 months of anticoagulation without issue prior to being instructed to stop. He denies any new medical history other than “weak kidneys”, medications, or recent surgeries. He is up to date with his HCM including vaccinations and colonoscopy. He does note that his daughter was recently home sick with an upper respiratory illness. You suspect that this patient may have a pulmonary embolus. What are common signs and symptoms of PE? - Dyspnea at rest or on excursion Pleuritic chest pain Orthopnea LE swelling or pain Wheezing Tachypnea Tacycardia - Rales Decreased breath sounds Accentuated P2 JVD CV collapse S/S of DVT Given the available data, what is the likelihood (pre-test probability) that the patient does have a PE and how does that affect you next step. Wells criteria: *Modified, simplified system with results of likely vs unlikely* Total >4 = PE likely 3pt Clinical signs of DVT 3pt *PE is most likely diagnosis 1.5pt Tachycardia >100 1.5pt Immobilization/surgery in last four weeks 1.5pt Past history of DVT/PE 1pt Hemoptysis 1pt Active malignancy (on treatment or treated w/in last 6 mo) If score is ≤ 4: Patient could be tested with a highly sensitive d-dimer. The dimer has negative predictive value meaning that paired with a low pre-test probability, a negative d-dimer could “rule out” the disease. A positive d-dimer does not favor the disease, but does necessitate further diagnostic testing. Note that this is not valid in patients with high pre-test probability and d-dimer has no utility in that scenario. This patient scores a 1.5 ± 3 depending if the physician feels that PE is the most likely diagnosis. The supporting evidence is lack of other diagnosis, non-specific inferior abnormalities on EKG, and evidence of small pleural effusion CXR without parenchymal abnormality. If your team of learners insists on a score of 1.5 report the d-dimer as positive and move on. Choose your next diagnostic test while discussing the available options as well your rational. 1. Catheter guided angiography: Considered “gold standard.” Not often ides due to invasive nature as well as the availability of validated non-invasive testing. 2. Spiral CT w/contrast non-coronary angio protocol: Iodinated contrast is injected IV, Contrast mixes in the RV prior to flowing into the pulmonary vasculature. The images are timed such that they are captured at the correct moment. Sensitivity varies widely by study 53-98, specificity ~90%. Should not be used in patient with renal insufficiency. 3. V/Q scan: A nuclear medicine study that shows ventilation and profusion mismatch. Are interpreted as high, low, and intermediate probability. Must be matched with pre-test probability to be useful. Difficult to interpret if patient has underlying parenchymal disease, does not differentiate between acute and chronic PE, could theoretically be fooled by AVM. 4. LE US: Even though you are considering diagnosis of PE, DVT and PE are treated the same. US is non-invasive without contrast or radiation. Due to this patient’s renal insufficiency (CrCl 48.8) the risk of contrast induced nephropathy should prompt a discussion, while it could be argued that patient’s crcl is not low enough to be a true contraindication to IV contrast, V/Q scan (or even LE u/s to start) would be an appropriate choice in the situation. Ventilation profusion scan is read as high probability for PE. What treatment(s) you start and why? Answer: Enoxaparin 1.5mg/kg q24h AND warfarin* The tempting answer would be IV UFH, both due to the patient’s renal status and due to the perceived onset of action of heparin. As above, the patient’s crcl is 48.8 making non-dose-adjusted enoxaparin an option. Fondaparinux may require monitoring and dose adjustment with crcl of 30-50 and is a less appropriate option. Warfarin can/should be started the same day as treatment. The American College of Chest Physicians makes the following recommendations: - In patients with acute PE, we suggest LMWH or fondaparinux over IV UFH In patients with acute PE treated with LMWH, we suggest once- over twice-daily administration In patients with acute PE, we recommend early initiation of VKA (eg, same day as parenteral therapy is started) over delayed initiation. * There is disagreement on the starting dose of warfarin. The ACCP suggest 10mg for 2 days, other sources (including the UNM pharmacists) would suggest 5mg. Other considerations: In patients with cancer and who are pregnant, LMWH is the preferred long term treatment. Warfarin is teratogenic. Studies in cancer patients suggest reduced recurrence rates with LMWH over warfarin, other agents are poorly studied. The ACCP supports LMWH in both scenarios. How long would you continue the overlap of SC/IV therapy and warfarin? What is the goal INR? Parenteral anticoagulation should be continued for at least 5 days and until the INR is 2.0 or above for at least 24 h. Goal INR 2.0-3.0 Should this patient be admitted to the hospital? There is some data to suggest that patients can be safe to discharge once appropriate therapy is defined, and in a very specific patient population. Essentially the patient would have little to no comorbid disease, no hypoxemia or hemodynamic changes, no bleeding risk, no con-current DVT of the leg, and good family support and means to obtain their medications and understand their disease. You decide to admit the patient to the hospital. You receive a call at 3am. The Patient’s O2 sat dropped below 90 prompting the nurse to initiate NC O2 supplementation which promptly increased the spO2. The nurse calls to inform you of this development, as well as his current vitals HR 103 BP 96/50. What is your first step? While thrombolytics are indicated in patient with acute PE and hypotension, the first choice would be a small fluid bolus (<500ml). This can improve hypotension, however, this should not be tried more than once. Fluid boluses over 500cc may cause right ventricular strain and subsequent failure. Your initial choice does not lead to improvement, repeat vitals show: HR 115, BP 86/46, Patient now on 4L NC with SpO2 of 90%. Detail your next actions. At this point, thrombolytics are indicated. No specific agent is recommended over another, but short infusion (2h) is recommended by the ACCP. Thrombolytics can be administered by PIV, however central access and pressor support may be needed while the medication is prepped and prior to effect. Patient makes full recovery and is ready for discharge. How long should therapy continue? Patient has two unprovoked VTEs, indication for indefinite therapy. Briefly 1st unprovoked = at least 3mo. 1st provoked = duration of provoking incident or 3mo. In all scenarios, patients should be periodically evaluated to re-assess risk/benefit ratio. One method of re-assessment uses d-dimer as a risk after therapy is completed. Example: Patient completes 3mo of therapy for 1st DVT, 4 weeks later he is symptoms free, but a d-dimer check is positive. In this case therapy would continue as he is “high risk for recurrence MKSAP 16 Questions Pulmonary and critical care #89: Diagnosing PE – Answer A Hematology Oncology #29: Treat a patient with acute VTE – Answer C Hematology Oncology #53: Treat DVT and cancer – Answer B Pulmonary and critical care #97: Treat PE in patient with kidney disease – Answer E Post Module Evaluation Please place completed evaluation in an interdepartmental mail envelope and address to Dr. Wendy Gerstein, Department of Medicine, VAMC (111) or give to Dr. Patrick Rendon at UNM Hospital. 1) Topic of module:__________________________ 2) On a scale of 1-5, how effective was this module for learning this topic? _________ (1= not effective at all, 5 = extremely effective) 3) Were there any obvious errors, confusing data, or omissions? Please list/comment below: ______________________________________________________________________________ ______________________________________________________________________________ ______________________________________________________________________________ ______________________________________________________ 4) Was the attending involved in the teaching of this module? Yes/no (please circle). 5) Please provide any further comments/feedback about this module, or the inpatient curriculum in general: 6) Please circle one: Attending Resident (R2/R3) Intern Medical student