Atopic Dermatitis - ND Center for Nursing
advertisement

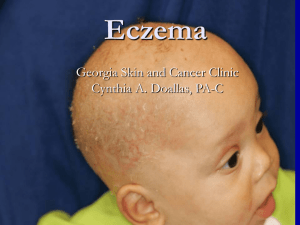
Running head: ATOPIC DERMATITIS 1 Critical Appraisal Topic Atopic Dermatitis By Jamie P. Slettedahl University of Mary, Bismarck, ND 8/1/2015 ATOPIC DERMATITIS Clinical Scenario T. M. is a 34-year-old female who presents to the clinic with history of atopic dermatitis and asthma. She has been treated for atopic dermatitis in the past with steroid and topical creams. These medications have provided relief, but T. M. feels when she experiences symptoms of atopic dermatitis they seem to be getting worse with each occurrence. What other treatment(s) or therapy could you offer during the office visit today? Background Several lines of evidence suggest that the incidence of psychiatric comorbidities, including major depression and anxiety disorders, is increased among patients with atopic dermatitis and may be influenced by factors such as perceived disease severity and quality of life (Vestergaard & Deleuran, 2014). A longitudinal cohort study evaluated the risk of developing major depression or anxiety disorders later in life among more than 8000 adolescents and adults with atopic dermatitis and age- and sex-matched controls (Cheng, Hsu, Huang, Bai, Su, Li, & Chen, 2015). Patients with atopic dermatitis had a six- and fourfold increased risk of developing major depression or anxiety disorders, respectively. These findings suggest that the identification and treatment of psychiatric comorbidities are important aspects of the management of patients with atopic dermatitis (Cheng et al, 2015). PICO Question Will adult patients with chronic atopic dermatitis have reduction exacerbations and pruritis through psychological interventions along with pharmacological treatment compared to a pharmacological treatment alone? Article 1 Summary Research has suggested a co-morbid association between atopic dermatitis and depressive disorder according to cross-sectional studies of 8,208 individuals with atopic dermatitis without psychiatric history and age/sex matched controls between 1998 and 2008 (Cheng et al, 2015). Subjects were 2 ATOPIC DERMATITIS identified during follow-up having developed depressive disorders, major depression, and anxiety disorders (Cheng et al, 2015). Stratification by age, individuals with atopic dermatitis were prone to developing both depressive disorders (95% CI: 4.01-7.99) and major depression (95%: 3.75-15.23) with increasing age correlated with atopic dermatitis. Although, further studies are required to clarify possible underlying mechanisms between atopic dermatitis and depression, it is clear that those patients with atopic dermatitis, regardless of age, are at risk for developing depression and need to be clinical assessed for appropriate adjunct therapy (Cheng et al, 2015). Level II Evidence Strengths: This study provides a high level of quality due to several factors, longitudinal cohort study and the number of subjects that participated in the research. In addition, level II evidence is matched with lack of opinion and author bias. Weakness: One particular weakness addressed in the study is that more information is needed on evaluating psychological interventions of atopic dermatitis patients. Opportunities: Atopic dermatitis affects adolescence and adults. Including psychological interventions with patient s with atopic dermatitis diagnosis will explore mental health status, which will have healthcare dividends as the individual’s ages. Threats: One treat or obstacle I feel is relevant is patient compliance and willingness to carry through with psychological interventions. Providers have a unique opportunity to stress education and preventative approaches with the usefulness of adjunct therapy. Article 2 Summary A study done by Wittkowski & Richards (2007), examined the benefits of cognitive behavior therapy in the treatment of patients with atopic dermatitis. This study was shown to demonstrate the usefulness of cognitive behavior therapy (CBT) as an adjunct to conventional dermatological care by minimize the negative impact of atopic dermatitis and thereby reducing overall atopic dermatitis related distress 3 ATOPIC DERMATITIS (Wittkowski & Richards, 2007). The study indicated sustained improvements in the patient’s quality of life and a reduction in perceived stigmatization through CBT. One limitation addressed in this study was the lack of objective assessment of atopic dermatitis severity (Wittkowski & Richards, 2007). Nevertheless, considerations in the use of psychiatric therapy such as CBT as an adjunct care is shown to reduce severity, as well as frequency of exacerbations of atopic dermatitis (Wittkowski & Richards, 2007). Level III Evidence Strengths: This evidence is rated level III due to the fact it includes case reports, single case study and author opinions. Weaknesses: This study indicated that there was a lack of objective assessment of atopic dermatitis severity with author opinions. In addition, this study is 8 years of age. Information specific for this PICO question was limited. Therefore, due to the particular search criteria and other aged research articles, this was allowed to be entered into assignment. Opportunities: As CBT expands and implemented in many aspects of medicine, not only is this becoming a widely used treatment option, but also will provide a need to fill positions for nurse practitioners. Threats: One particular threat is patient willingness to carry out therapy. Many patients may view CBT in terms of what is wrong with them, rather than an adjunct therapy. It will be most advantageous for nurse practitioners to make special efforts to calm patient fears and reluctance with CBT to reach therapy compliance. Clinical Bottom Line Both studies have demonstrated the importance in looking further into the needs of the patient with atopic dermatitis. Treatment should extend beyond the prescription of oral steroid and topical mediations with an appreciation of psychological interventions. These psychological interventions have been shown to be an appropriate adjunct therapy with atopic dermatitis. In addition, occurrences of 4 ATOPIC DERMATITIS atopic dermatitis has been reduced when assessing the patient’s psychological status by reducing depressive disorders and improving quality of life. These exceed patient outcomes versus pharmacological interventions alone. Therefore, treatment must involve the whole patient and include both physical and emotional health for successful treatment in a clinical setting as research has shown. 5 ATOPIC DERMATITIS 6 Questions As a nurse practitioner, how would you educate your patient on atopic dermatitis (eg triggers, flare-ups, prevention)? Would you inquire about allergy testing? What are some pharmacological treatment options for atopic dermatitis? Details from the research articles indicate an important connection with psychological interventions. How would you work this discussion into the treatment of atopic dermatitis with a young adult knowing that managing this condition is long-term with sensitivity to body image? When would you as a nurse practitioner determine the need to place a dermatological referral for a patient suspected with atopic dermatitis? What, if any complementary alternative therapies could be used for atopic dermatitis? ATOPIC DERMATITIS 7 References Cheng, C., Hsu, J., Huang, K., Bai, Y., Su, T., Li, C., & ... Chen, M. (2015). Risk of developing major depressive disorder and anxiety disorders among adolescents and adults with atopic dermatitis: A nationwide longitudinal study. Journal Of Affective Disorders, 17860-65. doi:10.1016/j.jad.2015.02.025 Wittkowski, A., & Richards, H. (2007). How beneficial is cognitive behaviour therapy in the treatment of atopic dermatitis? A single-case study. Psychology, Health & Medicine, 12(4), 445-449. Vestergaard, C., & Deleuran, M. (2014). Advances in the Diagnosis and Therapeutic Management of Atopic Dermatitis. Drugs, 74(7), 757-769. doi:10.1007/s40265-014-0219-3