NATIONAL PATHOLOGY ACCREDITATION ADVISORY COUNCIL
REQUIREMENTS FOR TRANSFUSION LABORATORY PRACTICE
(Second Edition 2013)
NPAAC Tier 4 Document
Print ISBN: 978-1-74241-958-9
Online ISBN: 978-1-74241-959-6
Publications approval number: 10207
Paper-based publications
© Commonwealth of Australia 2013
This work is copyright. You may reproduce the whole or part of this work in unaltered form
for your own personal use or, if you are part of an organisation, for internal use within your
organisation, but only if you or your organisation do not use the reproduction for any
commercial purpose and retain this copyright notice and all disclaimer notices as part of that
reproduction. Apart from rights to use as permitted by the Copyright Act 1968 or allowed by
this copyright notice, all other rights are reserved and you are not allowed to reproduce the
whole or any part of this work in any way (electronic or otherwise) without first being given
the specific written permission from the Commonwealth to do so. Requests and inquiries
concerning reproduction and rights are to be sent to the Online, Services and External
Relations Branch, Department of Health, GPO Box 9848, Canberra ACT 2601, or via e-mail
to copyright@health.gov.au.
Internet sites
© Commonwealth of Australia 2013
This work is copyright. You may download, display, print and reproduce the whole or part of
this work in unaltered form for your own personal use or, if you are part of an organisation,
for internal use within your organisation, but only if you or your organisation do not use the
reproduction for any commercial purpose and retain this copyright notice and all disclaimer
notices as part of that reproduction. Apart from rights to use as permitted by the Copyright
Act 1968 or allowed by this copyright notice, all other rights are reserved and you are not
allowed to reproduce the whole or any part of this work in any way (electronic or otherwise)
without first being given the specific written permission from the Commonwealth to do so.
Requests and inquiries concerning reproduction and rights are to be sent to the Online,
Services and External Relations Branch, Department of Health, GPO Box 9848, Canberra
ACT 2601, or via e-mail to copyright@health.gov.au.
First published 2008
Second edition 2013 reprinted and reformatted to be read in conjunction with the
Requirements for Medical Pathology Services
Requirements for Transfusion Laboratory Practice
1
Australian Government Department of Health
Contents
Scope ........................................................................................................................................3
Abbreviations ...........................................................................................................................4
Definitions .................................................................................................................................4
Introduction ..............................................................................................................................6
1.
Patient identification and labelling.............................................................................8
2.
Transfusion laboratory records ..................................................................................9
Laboratory records .........................................................................................................9
Compatibility record ....................................................................................................10
Labelling ......................................................................................................................10
Inventory management.................................................................................................11
3.
Pretransfusion testing ................................................................................................11
4.
Antenatal and perinatal testing ................................................................................14
5.
Selection of blood components ..................................................................................14
Selection of red cells for transfusion ...........................................................................14
Selection of non-red cell blood components ................................................................15
Fresh frozen plasma, extended life plasma and cryoprecipitate ..................................15
Platelet concentrates.....................................................................................................15
6.
Transfusion in special circumstances .......................................................................15
Emergency transfusion.................................................................................................16
Massive blood loss / critical bleeding ..........................................................................16
Antenatal and neonatal settings ...................................................................................16
Transfusion of patients with Autoimmune Haemolytic Anaemia ...............................16
Recipients of haemopoietic progenitor cells ................................................................17
7.
Autologous transfusion ..............................................................................................17
8.
Transfusion reactions ................................................................................................17
9.
Storage and transport of blood components and blood products .........................17
10.
Quality Assurance and Quality Control ..................................................................18
Appendix A (Normative) .......................................................................................................19
References ...............................................................................................................................29
Bibliography ...........................................................................................................................30
Further information...............................................................................................................20
The National Pathology Accreditation Advisory Council (NPAAC) was established in 1979
to consider and make recommendations to the Australian, state and territory governments on
matters related to the accreditation of pathology laboratories and the introduction and
maintenance of uniform standards of practice in pathology laboratories throughout Australia.
A function of NPAAC is to formulate Standards and initiate and promote education programs
about pathology tests.
Publications produced by NPAAC are issued as accreditation material to provide guidance to
laboratories and accrediting agencies about minimum Standards considered acceptable for
good laboratory practice.
Failure to meet these minimum Standards may pose a risk to public health and patient safety.
Scope
The Requirements for Transfusion Laboratory Practice is a Tier 4 NPAAC document and
must be read in conjunction with the Tier 2 document Requirements for Medical Pathology
Services. The latter is the overarching document broadly outlining Standards for good
medical pathology practice where the primary consideration is patient welfare, and where the
needs and expectations of patients, Laboratory staff and referrers (both for pathology requests
and inter-Laboratory referrals) are safely and satisfactorily met in a timely manner.
Whilst there must be adherence to all the Requirements in the Tier 2 document, reference to
specific Standards in that document are provided for assistance under the headings in this
document.
The Requirements for Transfusion Laboratory Practice is for use by transfusion Laboratory
personnel for the purpose of transfusion testing and safe transfusion Laboratory practice.
Current Australian and New Zealand Society of Blood Transfusion (ANZSBT)1 and National
Blood Authority (NBA)2 documentation may be used for further guidance.
These Requirements encompass:
documentation and accurate patient identification systems to minimise clerical errors
and misidentification
retention of records, data and documentation
red cell serology testing in the pretransfusion, antenatal and perinatal settings
requirements necessary for the use of computers and computer software in transfusion
Laboratory practice
quality assurance and quality control programmes for reagents, techniques and
personnel
selection and provision of appropriate blood and blood products
inventory management, storage and handling of blood and blood products
investigation of adverse events associated with transfusion.
There are additional requirements and recommendations that may apply in certain
circumstances e.g. special requirements for blood products in defined patient groups.
Abbreviations
ANZSBT
AS
IAT
ISO
IVD
NATA
NPAAC
RCPA
TGA
Australian and New Zealand Society of Blood Transfusion
Australian Standard
Indirect Anti-globulin Test
International Organization for Standardization
In Vitro Diagnostic Medical Device
National Association of Testing Authorities, Australia
National Pathology Accreditation Advisory Council
Royal College of Pathologists of Australasia
Therapeutic Goods Administration
Definitions
Blood components
means, generically in this document, red cells, platelets, fresh frozen
plasma, cryoprecipitate, cryodepleted plasma and whole blood.
Blood products
means, generically in this document, manufactured fractionated
plasma products.
Computer
crossmatching
means application of computer software to perform all the validity
checks required for the issue of compatible blood.
Confirmatory or
check group or
forward group
means testing of red cells for ABO and Rh(D) status using
commercial reagents.
External Quality
means a program in which multiple Specimens are periodically sent
to members of a group of Laboratories for analysis and/or
Assessment
In vitro diagnostic
medical device
(IVD)
identification, in which each Laboratory’s results are compared with
those of other Laboratories in the group and/or with an assigned
value, and reported to the participating Laboratory and others. Such a
program may also compare an individual’s results with their peer
group.
means a medical device test if it is a reagent, calibrator, control
material, kit, Specimen receptacle, software, instrument, apparatus,
equipment or system, whether used alone or in combination with
other diagnostic goods for in vitro use.
It must be intended by the manufacturer to be used in vitro for the
examination of Specimens derived from the human body, solely or
principally for the purpose of giving information about a
physiological or pathological state, a congenital abnormality or to
determine safety and compatibility with a potential recipient, or to
monitor therapeutic measures.
The definition of an IVD does not encompass products that are
intended for general Laboratory use that are not manufactured, sold or
presented for use specifically as an IVD.
In-house IVD
means an IVD that is developed de novo, or developed or modified
from a published source, or developed or modified from any other
source, or its intended purpose, within the confines or scope of a
Laboratory or Laboratory network, and is not supplied for use outside
the Laboratory or Laboratory network.
Commercial IVDs being used clinically for a purpose other than that
originally intended by the manufacturer are also classed as in-house
IVDs and are subject to the requirements of this standard.
Quality Assessment
means a measurement and monitoring function of quality assurance
for determining how well health care is delivered in comparison with
applicable standards or acceptable bounds of care.
Quality Assurance
means part of quality management focused on providing confidence
that quality requirements will be fulfilled.
Quality control
means the study of those errors that are the responsibility of the
Laboratory, and the procedures used to recognise and minimise them.
This study includes all errors arising within the Laboratory between
the receipt of the Specimen and the dispatch of the report. On some
occasions, the responsibility of the Laboratory may extend from the
collection of the Specimen from the patient and the provision of a
suitable container, to the dispatch and delivery of the report.
Internal quality control:
means processes and activities that are used within the Laboratory to
monitor the day-to-day operational and analytical performance of test
procedures. These activities may include on-going instrument
standardisation checks, instrument maintenance, analysis of control
material, statistical or graphical assessment of results from control
material.
Requirements for
Medical Pathology
Services (RMPS)
means the overarching document broadly outlining standards for good
medical pathology practice where the primary consideration is patient
welfare, and where the needs and expectations of patients, Laboratory
staff and referrers (both for pathology requests and inter-Laboratory
referrals) are safely and satisfactorily met in a timely manner.
The standard headings are set out below –
Standard 1 – Ethical Practice
Standard 2 – Governance
Standard 3 – Quality Management
Standard 4 – Personnel
Standard 5 – Facilities and Equipment
A – Premises
B – Equipment
Standard 6 – Request-Test-Report Cycle
A – Pre-Analytical
B – Analytical
C – Post-Analytical
Standard 7 – Quality Assurance
Reverse group
means testing of plasma or serum for the presence of anti-A and/or
anti-B to confirm results of a forward group.
Transfusion reaction
means any adverse event related to the transfusion of blood
component.
Transfusion record
means, for the purpose of this document, the patient’s Laboratory
record.
Introduction
Transfusion medicine is an essential part of medical practice and is critical to patient care.
The use of blood products and blood components provides essential therapeutic support in a
broad range of medical and surgical settings, and is associated with recognised risks.
The Requirements for Transfusion Laboratory Practice document is the NPAAC Standard to
be used to assure the safety, quality and efficacy of transfusion testing, associated transfusion
Laboratory practice, non-transfusion related blood group immunohaematology testing and for
accreditation purposes and must be read in conjunction with the Tier 2 document
Requirements for Medical Pathology Services.
Transfusion testing includes terms specific for this area of practice, and these are defined in
the ‘Definitions’ section of this document. Importantly, to assist in the interpretation of the
requirements, the terms ‘blood component’ and ‘blood product’ have been used to distinguish
between components produced within donor centres, and fractionated plasma derivatives.
NPAAC has produced these mandatory Requirements, in conjunction with ANZSBT1, for the
accreditation of transfusion Laboratories.
The ANZSBT is the pre-eminent specialist society in Laboratory and clinical transfusion
practice and has developed a number of guidelines in transfusion practice relevant to this
document.1
Future revisions of this document will be undertaken following the usual NPAAC practice
and ANZSBT Guidelines, and will also take into account initiatives from other professional,
national or federal organisations including TGA, NBA, Australian Red Cross and the
Australian Commission on Safety and Quality in Health Care dealing with regulatory
frameworks, haemovigilance, quality use and transport of blood components and products.
These Requirements are intended to serve as minimum Standards in the accreditation process
and have been developed with reference to current and proposed Australian regulations and
other standards from the International Organization for Standardization including:
AS ISO 15189 Medical laboratories – Requirements for quality and competence
These Requirements should be read within the national pathology accreditation framework in
conjunction with the current version of each of the following NPAAC documents:
Tier 2 Document
Requirements for Medical Pathology Services
All Tier 3 Documents
Tier 4 Document
Requirements for Procedures Related to the Collection, Processing, Storage and Issue
of Human Haemopoietic Progenitor Cells
In addition to these Standards, Laboratories must comply with all relevant state and territory
legislation.
In each section of this document, points deemed important for practice are identified as either
‘Standards’ or ‘Commentaries’.
A Standard is the minimum requirement for a procedure, method, staffing resource or
facility that is required before a Laboratory can attain accreditation – Standards are
printed in bold type and prefaced with an ‘S’ (e.g. S2.2). The use of the word ‘must’
in each Standard within this document indicates a mandatory requirement for
pathology practice.
A Commentary is provided to give clarification to the Standards as well as to provide
examples and guidance on interpretation. Commentaries are prefaced with a ‘C’ (e.g.
C1.2) and are placed where they add the most value. Commentaries may be normative
or informative depending on both the content and the context of whether they are
associated with a Standard or not. Note that when comments are expanding on a
Standard or referring to other legislation, they assume the same status and importance
as the Standards to which they are attached. Where a Commentary contains the word
‘must’ then that Commentary is considered to be normative.
Please note that Appendix A is normative and is an integral part of this document.
Please note that all NPAAC documents can be accessed at NPAAC Publication Website
While this document is for use in the accreditation process, comments from users would be
appreciated and can be directed to:
The Secretary
NPAAC Secretariat
Department of Health
GPO Box 9848 (MDP 951)
CANBERRA ACT 2601
Phone:
+61 2 6289 4017
Fax:
+61 2 6289 4028
Email: NPAAC Email Address
Website: NPAAC Website
1.
Patient identification and labelling
(Refer to Standard 6A in Requirements for Medical Pathology Services)
Accurate patient identification and Specimen labelling are crucial to patient safety. Failure to
comply with these requirements remains a significant cause of patient morbidity and
mortality.
S1.1
The request form must include a collector declaration similar to that below,
which must be signed by the person collecting the patient’s Specimen
immediately following verification of patient identity at time of collection:
I certify that I collected the accompanying specimen from the above patient whose
identity was confirmed by enquiry and/or examination of their name band and that
I labelled the specimen immediately following collection and before leaving the
patient.
S1.2
Where there is an electronic request, both the requestor and the collector must
be identified.
C1.2 (i) Where the request has been transported electronically there must be a
documented protocol indicating how the patient is to be identified at the point of
collection.
C1.2 (ii) If there is a current pretransfusion group and screen request, verbal requests
for blood group dependent blood components or blood products may be
accepted. These must be documented by the Laboratory.
S1.3
Specimen labelling must be correct, adequate and unambiguous.
C1.3(i) The patient’s details should be handwritten on the Specimen tube.
If pre-printed labels are used, they must comply with RMPS.
Hand-held computers in conjunction with barcode scanners and label printers
or radio-frequency identification (RFID) systems are available that facilitate
secure patient identification at the time of Specimen collection. The use of
such systems must be in accordance with the Specimen requirements.
C1.3(ii) The label must include the date and time of collection and the collector’s
name / initials.
2.
Transfusion Laboratory records
(Refer to Standard 6 in Requirements for Medical Pathology Services)
Laboratory records
S2.1
Where pretransfusion record management is computerised, the Laboratory
information system must comply with NPAAC’s requirements that address
information communication and retention of records.
S2.2
Each patient’s Laboratory transfusion record for blood components must
contain the following information
Patient (recipient):
(a)
family name and given name(s)
(b)
medical record number or date of birth
(c)
date and time of Specimen collection and expiry date
(d)
ABO/Rh(D) blood group
(e)
antibody screen results or antibody specificity where applicable
(f)
antigen typings where available
(g)
identification of the person performing the compatibility testing.
Blood component:
(a)
component type
(b)
donation/batch number
(c)
ABO/Rh(D) blood group (where applicable)
(d)
expiry date of the component
(e)
date and time of issue.
For fractionated blood products to individual patients the record must include:
(a)
family name and given name(s)
(b)
medical record number or date of birth
(c)
product type
(d)
donation/batch number
(e)
expiry date of the product
(f)
date and time of issue.
For fractionated blood products to a clinical area the record must include:
(a)
component type
(b)
donation/batch number
(c)
clinical area sent to
(d)
date and time of issue
(e)
expiry date of product.
Compatibility record
S2.3
A permanent record of each unit of blood component issued to a patient must
contain the following:
(a)
patient’s family name and given name(s)
(b)
medical record number or date of birth
(c)
ABO/Rh(D) blood group and antibody screen of patient
(d)
component details including type, donation number, blood group and
expiry date
(e)
details of any special requirements, warnings or other relevant
information.
Labelling
S2.4
A ‘compatibility’ label must be securely attached to each blood component unit
or blood product unit once pretransfusion testing (or selection) is completed and
the unit is allocated to the patient. It must contain the following information:
Patient (recipient):
(a)
family name and given name(s)
(b)
medical record number or date of birth
(c)
ABO/Rh(D) blood group.
Blood component:
(a)
donation or batch number
(b)
ABO/Rh(D) blood group
(c)
statement of compatibility
(d)
identity of the person affixing the label.
Inventory management
S2.5
The Laboratory must have systems in place to trace every blood component or
blood product which it issues, whether this is to a patient, clinical area, another
facility or disposal. The Laboratory must record the following information in
relation to each blood component or blood product it receives (according to
national or jurisdictional policy):
(a)
source
(b)
donation or batch number
(c)
blood component or blood product type
(d)
ABO/Rh(D) group (where applicable)
(e)
date and time received
(f)
expiry date
(g)
recipient's family name, given name(s), medical record number or date of
birth
(h)
date and time of issue
(i)
3.
the fate of the blood component or blood product (issued, recalled,
expired, transferred, or discarded).
Pretransfusion testing
(Refer to Standard 6 in Requirements for Medical Pathology Services)
S3.1
An ABO and Rh(D) group must be determined for all Specimens accepted for
pretransfusion testing.
C3.1
Forward and reverse groups must be performed for all Specimens for
pretransfusion testing. For newborns and confirmatory groups, only the
forward group is required.
S3.2
When performing blood grouping, all discrepancies must be resolved (eg. with
historical records).
S3.3
The ABO and Rh(D) group must be confirmed before red cells are transfused
by:
S3.4
(a)
comparing the current findings with those recorded for previous
Specimens; or
(b)
repeating the test (manual or automated) on the same Specimen by
re-testing on a separate occasion to the first test; or
(c)
testing a second Specimen collected separately from the original
Specimen.
C3.3
Where possible in manual testing, a second worker, having no prior knowledge
of the initial result, should perform the second test. A reverse ABO group is
not mandatory when performing this confirmatory group check. If automated
equipment is used the group check should be performed by reloading and
rescanning the Specimen.
The ABO group of all donor red cell units and the Rh(D) group of those labelled
as Rh(D) negative must be confirmed by the Laboratory undertaking the
pretransfusion testing.
C3.4(i)
Blood group confirmation of donor red cell units must be performed by a
forward group check.
C3.4(ii) In the case of a branch Laboratory accepting units for pretransfusion testing
from the parent Laboratory and the latter has checked the group of the units
and the Laboratories are on the same IT and blood bank inventory systems,
then the branch Laboratory can proceed directly to the pretransfusion
testing. Confirmatory weak D testing of donor red cell units is not required.
S3.5
Pretransfusion testing must include an antibody screen capable of detecting
potentially clinically significant red cell antibodies.
C3.5
Clinically significant antibodies are generally considered to be those, which
are reactive by the indirect antiglobulin test (IAT) performed at 37°C. Note
that anti-A, -B and -A, B must always be regarded as clinically significant.
If the patient is known to have a red cell antibody, testing to exclude formation
of additional antibodies must be undertaken for each new Specimen received
if it is to be used for further crossmatching (see Appendix A).
S3.6
The reagent red cells used for antibody screening must come from at least two
separate group O donors and between them express the following antigens: C, c,
D, E, e, M, N, S, s, K, k, Fya, Fyb, Jka, Jkb and Lea.
The cells from different donors must not be pooled to achieve the desired range
of antigen expression. One cell must be of R1R1 and another of R2R2
phenotype. The following phenotypes must be represented in the screening cells:
Jk(a+b-), Jk(a-b+), Fy(a+b-) and Fy(a-b+).
C3.6(i) Anti-Kpa and anti-Cw are rarely of clinical significance; consequently
Kpa + and Cw+ screening cells are not essential.
C3.6(ii) It is also desirable to include SS and ss phenotypes in the screening cells.
S3.7
Antibody identification must be performed using a reagent red cell panel
employing at least the method(s) by which the antibody is detectable.
S3.8
The specificity of antibodies detected during antibody screening must be
investigated and clinical significance assessed (see Appendix A).
C3.8
S3.9
Antibody identification must be confirmed by typing patient’s cells for
corresponding antigen(s) (if not transfused in the past 3 months), if antisera are
available. Antibody identification may be referred to a reference Laboratory.
The Laboratory must have procedures in place to exclude incompatibility
between the recipient and donor.
C3.9
It is essential that ABO incompatibility is excluded by whatever procedure is
used. Group specific red cells must not be released solely on the basis of
historical records. Only group O red cells are to be released in an emergency
situation where there is no current group and screen.
S3.10 If a computer crossmatching and remote release facility is used the following
conditions must be met:
(a)
a comprehensive, validated, electronic data management system is in
place
(b)
a valid pretransfusion Specimen has been tested in accordance with the
requirements of S3.1 and S3.5
(c)
there are no clinically significant antibodies detectable in the current
Specimen and there is no history of clinically significant antibodies.
S3.11 For a patient who has been transfused in the previous 3 months, Specimens must
not be used more than 72 hours after collection.
C3.11 The appropriate storage time for Specimens collected from
immunocompromised or pregnant patients should be determined at the
discretion of the Laboratory in conjunction with the attending clinician.
S3.12 Specimen validity for pretransfusion testing is predicated by appropriate
Specimen storage.
C3.12 The following table outlines the requirements for Specimen storage in relation
to transfusion and pregnancy status.
Criteria
The patient, in the last three
months has been transfused
Patients known not to have
been transfused in the
previous three months (refer
to S3.11)
Specimen collected in
advance of elective surgery
(‘preadmission’ Specimens)
and where the patient’s
history clearly excludes
transfusion or pregnancy in
the previous three months
Specimen Validity
72 hours
Storage conditions
7 days
2–6 C
1 month
Serum/plasma must be
separated and stored frozen at
or below
–20°C
2–6 C
The above are working limits for Specimen storage if used for serological testing.
4.
Antenatal and perinatal testing
(Refer to Standard 6 in Requirements for Medical Pathology Services)
S4.1
Request form and Specimen labelling for antenatal and perinatal testing must
conform with the requirements in Section 1.
S4.2
When performing blood grouping on antenatal patients, any discrepancy with
historical records must be resolved.
S4.3
Antibody screening and identification of detected antibodies must be performed
consistent with the requirements in S3.5, S3.6 and S3.7.
S4.4
The requirements for pretransfusion testing during pregnancy must be in
accordance with Section 3.
5.
Selection of blood components
(Refer to Standard 6B in Requirements for Medical Pathology Services)
Selection of red cells for transfusion
S5.1
There must be clearly written policies on the selection of red cells for both
routine and exceptional transfusion situations.
C5.1
S5.2
Red cells that are negative for the relevant antigen where a clinically
significant antibody is present or there is historical evidence of a clinically
significant antibody, must be selected if available and time and clinical
circumstances permit.
Group O red cells must be selected when the patient's ABO group cannot be
determined.
C5.2(i)
If a confirmed Rh(D) group cannot be obtained, Rh(D) negative red cells
should be used until a definitive result is available.
C5.2(ii)
Red cell components should be of the same ABO and Rh(D) type as the
patient whenever possible. Use of Rh(D) positive red cells in postmenopausal women and males who are Rh(D) negative may need to be
considered in times of shortage.
C5.2(iii)
When transfusion is unavoidable and serologically compatible units are
not available, taking into consideration the specificity of the antibody,
incompatible units may be given after consultation between the
responsible medical officer and a senior specialist from the transfusion
Laboratory.
C5.2(iv)
Patients undergoing long-term transfusion regimens should have an
extended phenotype performed (for example Cc, Ee, Jka, Jkb, Fya, Fyb,
M, K, Ss – refer to S3.5) before their initial transfusion. Consideration
should be given to providing red cells of the patient’s Rh and K types
where readily available.
Selection of non-red cell blood components
Fresh frozen plasma, extended life plasma and cryoprecipitate
S5.3
Plasma components of different blood groups must not be pooled.
C5.3(i)
Plasma components of any Rh(D) type may be given without regard to the
recipient’s Rh(D) status. Anti-D immunoglobulin is not required if Rh(D)
negative recipients receive plasma components from Rh(D) positive
donors.
C5.3(ii)
Plasma components should be ABO-compatible with the recipient.
However, at times of short supply of AB plasma group A plasma may be
used for AB recipients.
Platelet concentrates
S5.4
Individual units of different ABO blood groups must not be pooled.
C5.4(i)
Platelet concentrates should be of the same ABO group as the recipient.
Where crossing ABO groups is necessary consideration should be given to
the type of platelet component, whether obtained by apheresis (currently
suspended in plasma) or pooled (in platelet additive solution).
C5.4(ii) It is important to ensure, where possible, that platelets from Rh(D)
positive donors are not given to Rh(D) negative females of child bearing
potential. If this occurs then administration of Rh(D) immunoglobulin at
the recommended dosage may be considered to limit the risk of
sensitisation.
6.
Transfusion in special circumstances
(Refer to Standard 6 in Requirements for Medical Pathology Services)
Emergency transfusion
S6.1
Specimens must be labelled in accordance with routine pretransfusion practice
and standard pretransfusion testing performed (see Section 1 and Section 3).
S6.2
Red cells must not be issued in emergency situations on the basis of an historical
blood group alone.
C6.2(i)
If there is insufficient time to complete full pretransfusion testing, ABO
and Rh(D) compatible red cells (preferably group specific) may be issued
once the patient’s ABO and Rh(D) blood group has been determined (see
S3.1).
C6.2(ii)
Plasma components should be ABO-compatible with the recipient.
However, at times of short supply of AB plasma group A plasma may be
used for AB recipients. Where blood components are required before
pretransfusion testing can be performed:
(a)
red cells must be group O
(b)
plasma components must be group AB.
S6.3
If the antibody screen is positive or a subsequent crossmatch incompatible, the
treating clinician must be informed.
S6.4
The Laboratory must have criteria for the issue of Rh(D) positive red cells and
platelets when Rh(D) negative stocks of these components are limited.
S6.5
Red cells issued before completion of pretransfusion testing must be clearly
labelled for example ‘Uncrossmatched blood’ or ‘Emergency issue compatibility testing not completed’.
C6.5
Rh(D) positive red cells and platelets should not be given to Rh(D) negative
females with child bearing potential, except in life threatening circumstances.
If this occurs then administration of anti-D immunoglobulin may be
considered to limit the risk of sensitisation.
Massive blood loss / critical bleeding
S6.6
The Laboratory must have a written policy for provision of blood components
and blood products in massive blood loss / critical bleeding.
Antenatal and neonatal settings
Guidance on the selection and use of blood components and blood products in antenatal and
neonatal settings should be sought from current ANZSBT documentation1.
Transfusion of patients with Autoimmune Haemolytic Anaemia
S6.7
The Laboratory must have a written procedure for the serological investigation
of patients prior to provision of red cell components, if clinically necessary, for
patients found to have autoantibodies due to autoimmune haemolytic anaemia
(AIHA). Prior to the provision of red cells, consultation with the treating
clinician must occur.
Recipients of haemopoietic progenitor cells
S6.8
Laboratories involved in the provision of blood components to recipients of
haemopoietic stem cell grafts must have clear protocols on the selection of blood
components with respect to ABO and Rh(D) groups of recipient and donor.
C6.8
7.
Guidance relating to the use of blood components in this setting should be
sought from the NPAAC document Requirements for Procedures Related to
the Collection, Processing, Storage and Issue of Human Haemopoietic
Progenitor Cells and from ANZSBT documentation1.
Autologous transfusion
(Refer to Standard 6A in Requirements for Medical Pathology Services)
S7.1
All Laboratories involved in the provision of a pre-donation autologous blood
service must have clear protocols for the collection, testing, storage and issue of
these units, as appropriate to the service provided.
S7.2
All autologous units must be clearly labelled to distinguish them from allogeneic
(homologous) units (and stored in a separate designated area). Screened and
unscreened autologous units must be separated and stored in designated areas.
S7.3
Pretransfusion testing, labelling and documentation must be performed in
accordance with S1, S3 and S5.
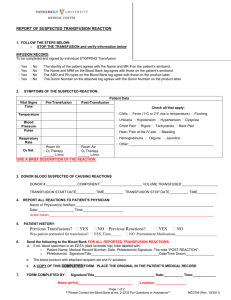
8.
Transfusion reactions
(Refer to Standard 6 in Requirements for Medical Pathology Services)
S8.1
The Laboratory must have systems in place to identify or be notified of reactions
or other adverse events associated with transfusion.
S8.2
The Laboratory must have written procedures for the recording, management,
investigation and reporting of suspected transfusion reactions or other
transfusion-related adverse events to the relevant provider of the blood
component or blood product.
S8.3
Suspected transfusion transmission of bacterial or viral infections must be
immediately reported to the relevant manufacturer of the component or product.
9.
Storage and transport of blood components and blood
products
(Refer to Standard 3 and Standard 5 in Requirements for Medical Pathology
Services)
S9.1
There must be policies dealing with storage and transport of blood components
and blood products.
C9.1(i) Blood components and blood products must be stored in an appropriate
temperature controlled (and monitored) environment to conform with
AS 3864 Medical Refrigeration Equipment — For the Storage of Blood
and Blood Components3.
10.
C9.1(ii)
Other blood components and blood products must be stored according to
the Australian Red Cross Blood Service document Blood Component
Information (Circular of Information) 20124.
C9.1(iii)
Blood components and blood products must be transported in a manner
suitable for purpose to maintain specified transport temperatures. Where
containers are used for transport purposes, these must be validated.
C9.1(iv)
For each storage facility there must be written procedures for handling
blood components and blood products stored outside temperature
specifications
Quality Assurance and Quality Control
(Refer to Standard 7 in Requirements for Medical Pathology Services)
Appendix A (Normative)
Selection of red cells where antibodies are reactive by indirect antiglobulin test (IAT) at
37°C
Specificity
Clinically significant
Selection of unitsa
Anti-A1
Rarely
IAT crossmatch compatible
Anti-HI (in A1 and A1B patients)
Rarely
IAT crossmatch compatible
Anti-D, -C, -c, -E, -e
Yes
Antigen negative
Anti-CW
Rarely
IAT crossmatch compatible
Anti-K, -k
Yes
Antigen negative
Anti-Kpa
Rarely
IAT crossmatch compatible
Anti- Jka, -Jkb
Yes
Antigen negative
Anti-M
Sometimes
IAT crossmatch compatible
Anti-N
Sometimes
IAT crossmatch compatible
Anti-S, -s, -U
Yes
Antigen negative
Anti-Fya, -Fyb
Yes
Antigen negative
Anti-P1
Rarely
IAT crossmatch compatible
Anti-Lea, -Leb, -Lea+b
Rarely
IAT crossmatch compatible
Anti-Lua
Rarely
IAT crossmatch compatible
Anti-Wra
Rarely
IAT crossmatch compatible
High titre low-avidity antibodies
(HTLA)
Unlikely
Antibodies against low or high
frequency antigens
Depends on specificity
Local Laboratory policy or
seek advice from reference
Laboratory
Local Laboratory policy or
seek advice from reference
Laboratory
Other antibodies active by IAT at 37°C
Seek advice from reference Laboratory
a Where antigen negative red cells are specified these should also be IAT crossmatch compatible (at 37°C)]
References
1.
ANZSBT (Australian and New Zealand Society of Blood Transfusion) publications.
Available at ANZSBT Website
2.
NBA (National Blood Authority) publications. Available at <http://www.nba.gov.au>
3.
AS 3864:1997 Medical Refrigeration Equipment - For the Storage of Blood and
Blood Products, Standards Australia Ltd.
Australian Red Cross Blood Service Blood Component Information
Circular for Information 2012. Available at Red Cross
Transfusion Website
Bibliography
1.
AS4633 (ISO 15189) Field Application Document – Medical Testing –Supplementary
requirements for accreditation August 2007.
2.
BCSH Guidelines (2007), British Committee for Standards in Haematology, Newcastle,
UK, viewed 30 April 2008, <BCSH Guidelines Website>
Further information
Other NPAAC documents are available from:
The Secretary
NPAAC Secretariat
Department of Health
GPO Box 9848 (MDP 951)
CANBERRA ACT 2601
Phone:
+61 2 6289 4017
Fax:
+61 2 6289 4028
Email: NPAAC Email Address
Website: NPAAC Website