File - Pricilla Puente`s Nursing Portfolio
advertisement

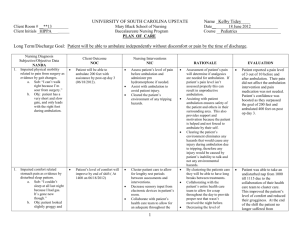
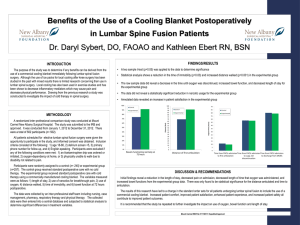
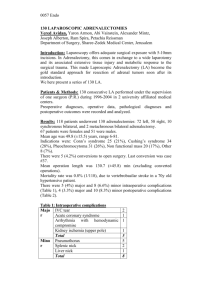
Running head: EBP PAPER 1 EBP Paper Pricilla Puente University of South Florida EBP PAPER 2 EBP Paper “Early ambulation is the most significant general nursing measure to prevent postoperative complications” (Canavarro, n.d.). According to Healee (2011), delayed ambulation after hip surgery is associated with poor hospital outcomes and emphasizes the importance of early ambulation after hip surgery. The purpose of this research paper is to describe the benefits of postoperative ambulation, list the medical complications that postoperative ambulation prevents, explain the purpose of postoperative ambulation, describe how soon to begin postoperative ambulation, and describe medical and nursing intervention and care guidelines as applied to postoperative patients. Pathophysiology There are a variety of common postoperative complications related to immobility. According to Kehlet (2007), the pathogenesis of cardiac complications include cardiac stimulation and pulmonary complications include impaired pulmonary and diaphragmatic function. Thromboembolisms may form as a result of altered coagulatory balance. Cerebral dysfunction may occur related to surgical stress. Infection may also be a result of contamination and/or immunosuppression. Afferent stimulation and constipation related to anesthesia may cause nausea and gastrointestinal dysfunction. Impaired wound healing may be a result of malnutrition, catabolism, and infection. Fatigue reduced functional capacity, and convalescence may be a result of a loss of muscle tissue and function, immobilization and impaired cardiovascular adaptation to exercise. Kehlet stated that the benefits of postoperative ambulation include improved oxygenation/respiratory function, cardiovascular function, wound healing, and renal function. Postoperative ambulation also reduces the risk for respiratory infections and prevents EBP PAPER 3 pneumonia. Michota (2009) stated that postoperative ambulation also restores normal bowel function by promoting gastrointestinal motility as agents used for general anesthesia can cause constipation after surgery. For example, benzodiazepines slow the movement of stool in the colon and barbituates depress the central nervous system and directly impact the colon’s motility. Adequate blood flow discourages the formation of blood clots and enhances healing; thus, postoperative ambulation also decreases the risk of deep vein thrombosis and pulmonary embolisms which are two life-threatening conditions (Michota, 2009). Medical/Nursing Interventions and Care Guidelines Canavarro concluded that the optimum time to ambulate is the day after surgery within the first 24-36 hours before complications have occurred. If ambulation begins later than the third postoperative day, then few benefits are obtained, if any. Ambulation should take place post-operative day one with initial evaluation, patient education, mobility, functional training, as well as increased range of motion and motor control. As a part of patient-centered care, patient’s concerns about early mobilization must be acknowledged and patient education should begin as soon as possible after surgery. Parker stated that ambulation should be conducted systemically and consistently. A multi-focal approach should be used to see best results with regards to patient outcomes. To decrease pain, encourage partial weight bearing ambulation to relieve weight, pressure, and stress on the affected leg. For example, a walker may be used to relieve stress on the affected limb. Maximum comfort should be ensured to provide the patient with encouragement and support for ambulation. EBP PAPER 4 Clinical Relevance/Application A 66 year-old female with a history of degenerative joint disease (DJD) and osteoarthritis (OA) fell down a flight of stairs and fractured her right hip. After a consultation with the orthopedic surgeon, the patient decided to undergo a right total hip arthroplasty. The patient was hesitant, afraid, and unwilling to participate in postoperative ambulation. The nurse acknowledged the patient’s wish to not ambulate post-operative day one. The patient had been on bed rest for two days post op. Patient is now experiencing a productive cough, severe constipation, impaired wound healing, and decreased circulation to her surgical site. Upon assessment the nurse noted some wheezing and crackles in the lungs. Ambulation was now medically indicated and attempts were made to get the patient up and walking. On first attempt, patient complained of dizziness and nausea. This was documented, doctor made aware, and attempts scheduled for later in the day. On second attempt, patient was questioned about the earlier dizziness and nausea, it was no longer present. The patient, assisted by staff, got up, fell, and broke her ankle. The nurse in the scenario assessed the patient prior to getting her up. The nurse saw no reason for the patient to not ambulate. She made an attempt to carry out the physicians orders following applicable standards of care. Ambulation was completely appropriate in this case. The patient was assessed to be safe to ambulate within the nursing scope of practice. The fall was unfortunate, but cannot be attributed to negligence on the nurse’s part. Medical/Nursing Interventions and Care Guidelines Nursing interventions include getting a patient up and walking. This will minimize the chances of complications such as deep vein thrombosis, pneumonia, pulmonary emboli, and decubitus ulcers (Michota, 2009). The nurse’s role is to first verbalize the patient the important EBP PAPER 5 of mobilization postoperatively. A nurse must be armed with evidence and perhaps an institution based protocol to motivate the patient to ambulate post-surgery. It is a nurse’s responsibility to offer patient resources in patient-friendly language describing the importance of early ambulation and the health care team’s role (including the patient). Gaps include the fact that any post-operative patient can have complications related to immobilization or not. For example, a patient having hip replacement can form a clot after surgery and develop a stroke, pulmonary embolus, deep vein thrombosis, or other complications. Even if surgery and nursing care afterwards were appropriate, in absence of negligence, there’s no guarantee that complications will not occur. Thus, desired outcomes are not always guaranteed and complications do occur as every patient is different. EBP PAPER 6 References Canavarro, K. (n.d.) Early Postoperative Ambulation. Annals of Surgery, 124. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1803619/. Healee, D.J., McCallin, A., & Jones, M. (2011). Older adult’s recovery from hip fracture: A literature review. International Journal of Orthopedic and Trauma Nursing, 15. Retrieved from http://www.orthopaedictraumanursing.com/article/S18781241(10)00056-0/abstract. Kehlet, H. (1997). Multimodal approach to control postoperative pathophysiology and rehabilitation. British Journal of Anesthesia, 78. Retrieved from http://bja.oxfordjournals.org/content/78/5/606.abstract Michota, F.A. (2009). Prevention of venous thromboembolism after surgery. Cleveland Clinic Journal of Medicine, 76. Retrieved from http://www.ccjm.org/content/76/Suppl_4/S45.full. Parker, R.J. (2011). Caring for a Patient Undergoing Total Knee Arthroplasty. Orthopedic Nursing, 30. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/21278547