Physiology 30 [5-11
advertisement

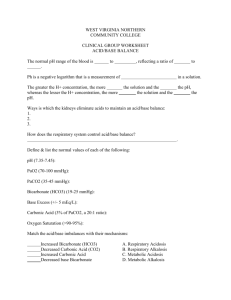
Physiology 30: Acid-Base Regulation - - - All enzyme systems in body are influenced by H+ concentration o Normally kept at low level (.00004 mEg/L) and precisely regulated (within 3-5 nEq/L) Acids release H+ in solutions (ex. HCl, H2CO3) Base accepts H+ (ex. HCO3, HPO4, proteins [i.e. Hgb]) o Alkali = molecule formed by combo of 1+ alkaline metals (Na, K, Li, etc) with highly basic ion like OHStrong acid = rapidly dissociates and releases H+ (HCl); weak acid = less likely to dissociate (H2CO3) Strong base = reacts rapidly and strongly with H+ (OH-); weak base = binds H+ weakly (HCO3) o Most acids and bases in ECF are weak In extreme conditions [H+] can vary from 10 nEq/L to 160 nEq/L without causing death pH = log(1/[H+]) = -log [H+] o normal pH of arterial blood = 7.4 and venous blood = 7.35 (extra CO2) acidosis <7.4 and alkalosis >7.4 (limits of survival 6.8-8) o intracellular pH slightly lower than plasma (metabolism produces acid) -> 6-7.4 o pH of urine 4.5-8 and in stomach 0.8 Chemical acid-base buffer systems of body fluids, respiratory center, and kidneys regulate [H+] (in order of speed of reaction) Buffer = reversibly bind H+ (Buffer + H+ ↔ H Buffer) o With high H+ pushed to right as long as buffer available Bicarbonate buffer system: weak acid (H2CO3) and bicarbonate salt (NaHCO3) o CO2 + H2O ↔ H2CO3 (via carbonic anhydrase) CA abundant in lung alveoli and renal tubules o -- → H H2CO3 ← o - + HCO3- Weak ionization NaHCO3 ← --→ Na + + HCO3- NaHCO3 in ECF; ionizes almost completely o ↑H + HCO3 → H2CO3 → CO2 + H2O (strong acid stimulates respiration) o NaOH + H2CO3 → NaHCO3 + H2O (CO2 in blood decrease, inhibits respiration, renal HCO3 excretion) Dissociation constant K’ = H+ x HCO3/H2CO3 o Cannot be directly measured but CO2 dissolved in blood directly proportional to H2CO3 so… H+ = K x CO2/HCO3 K is only 1/400 of K’ CO2 = 0.03 x Pco2 ← measured in labs Henderson-Hasselbalch equation = -log H+ = -log pK – log (0.03 x Pco2)/HCO3o pH = pK – log (0.03 x Pco2)/HCO3- OR pH = 6.1 + log HCO3-/ (0.03 x Pco2) HCO3 concentration is regulated by kidneys, Pco2 controlled by rate of respiration Disturbance in ECF [HCO3] = metabolic; Disturbance in Pco2 = respiratory + - + - - - - - When HCO3 and CO2 are equal, pH = pK (6.1). When acid added, HCO3 buffers. When base added, CO2 converts to HCO3 Bicarbonate buffer system is most effective in central part of titration curve (around pK) o Between 5.1-7.1 units still effective but beyond this ineffective o Most powerful extracellular buffer system Phosphate buffer system: role in buffering renal tubular fluid and intracellular fluids o Main elements: H2PO4 and HPO4 HCl + Na2HPO4 → NaH2PO4 + NaCl (strong acid replaced by weak acid) NaOH + NaH2PO4 → Na2HPO4 + H2O (strong base replaced by weak base) o pK of 6.8 allows system to operate near max buffering power o important in tubular fluids of kidney because phosphate becomes greatly concentrated in tubules, tubular fluid has lower pH than ECF o important in buffering ICF because phosphate greater in ICF Proteins as buffers: o Diffusion of elements of bicarbonate buffer system causes pH in ICF to change with ECF o H+ + Hgb ↔ HHgb 60-70% of chemical buffering of body fluids is inside cells (ICF proteins) but takes longer to kick in All buffer systems work together because H+ common in all = isohydric principle o H+ = K1 x (HA1/A1) = K2 x (HA2/A2) = K3 x (HA3/A3) Respiratory regulation of acid-base balance = second line of defense o CO2 formed by intracellular metabolism and diffuses into blood to lungs (1.3 mol/L normally in ECF = Pco2 of 40 mmHg) Change in pulmonary ventilation or rate of CO2 formation changes ECF Pco2 o High alveolar ventilation lowers PCO2 H+ concentration affects rate of alveolar ventilation (compensation for high pH not as effective as response to reduced pH) o Respiratory system acts as negative feedback controller of [H+] Cannot return [H+] to normal when disturbance outside respiratory system (Effective between 50-75% feedback gain of 1-3) o Respiratory regulation of acid-base balance is a physiologic type of buffer system (acts rapidly until kidneys take over) o Abnormalities of respiration (emphysema) -> respiratory acidosis and inability to respond to metabolic acidosis Renal control of acid-base balance: o HCO3 filtered continuously into tubules and H+ secreted o Body produces 80mEq of nonvolatile acids (can’t be excreted by lungs) and removed by kidney most HCO3 reabsorbed conserving primary buffer system but must react with H+ to form H2CO3 first o Kidneys regulate ECF [H+] via secretion of H+, reabsorption of filtered HCO3 and production of new HCO3 - - - - - - - H+ secretion and HCO3 reabsorption occur in all tubules except descending and ascending thin limbs of loop of Henle o Bicarb reabsorption: 85% in proximal tubule, 10% in TAL, and 5% in early distal tubule All secrete H+ by Na/H counter-transport (sodium-hydrogen exchanger protein) Gradient established by Na/K ATPase on basolateral membrane CO2 (from diffusion or metabolism) combines with H2O -> H2CO3 (via carbonic anhydrase) -> dissociates into HCO3 and H+ o H+ secreted in tubules counter to Na and HCO3 moves with Na out into blood H+ secretion and HCO3 filtration combine -> H2CO3 -> CO2 + H2O. CO2 diffuses into tubular cell and recombines with H2O -> H2CO3 -> HCO3 + H+ o HCO3 diffuses into blood via Na-HCO3 co-transport in proximal tubule and Cl-HCO3 exchange in late proximal tubule, TAL, and collecting tubules Each time H+ formed in tubular epithelial cells, HCO3 also formed and released back into blood HCO3 and H+ “titrate” each other in tubules (slight excess of H+ to rid nonvolatile acids) o Excess H+ complete reabsorption of HCO3, excess HCO3 exceeds H+ available In late distal tubule -> H+ secreted by primary active transport (via hydrogen-transporting ATPase) -> occurs in intercalated cells o CO2 in cell combines with H2O -> H2CO3 -> HCO3 (reabsorbed) + H+ (secreted) o Only 5% of total H+ secreted (important for max acidic urine pH 4.5) Only small H+ excreted in ionic form. Most excretion via combo with phosphate and ammonia buffers (urate and citrate too) o In excess H+ in ECF, kidneys reabsorb all filtered HCO3 and generate new HCO3 Phosphate buffer carries excess H+ into urine, generates new HCO3 o HPO4 and H2PO4 concentrated in tubular fluid and pK of system 6.8 o When all HCO3 reabsorbed, excess H+ + HPO4 -> H2PO4 (excreted as NaH2PO4) Net effect is addition of new HCO3 to blood o Only 30-40 mEq/day of phosphate available to buffer Ammonia buffer (NH3 and NH4+): synthesized from glutamine (AA metabolism in liver) -> metabolized in tubules to form 2 NH4 and 2 HCO3 (new bicarbonate) o HCO3 transported with Na across basolateral membrane and NH4 secreted (countertransport with Na) o In collecting tubules H+ secreted combining with NH3 (diffuses into lumen) -> NH4+ (impermeant so excreted) For each NH4+ excreted, a new HCO3 is generated and added to blood o Ammonia buffer subject to physiologic control Increased ECF [H+] stimulates glutamine metabolism and vice versa o H+ eliminated via ammonia buffer = 50% of acid excreted and 50% of new HCO3 In chronic acidosis, dominant mechanism by which acid is eliminated is excretion of NH4+ Bicarbonate excretion = V x U[HCO3] - - - - - - New HCO3 = H+ secretion o Calculated by measuring NH4 excretion = V x U[NH4+] NonHCO3, nonNH4 buffer in urine measured by determining titratable acid o titrate strong base NaOH to pH of 7.4. mEq required = mEq of H+ added to tubule fluid Net acid excretion = NH4+ excretion + urinary titratable acid – HCO3 excretion o Must equal nonvolatile acid production in body o In acidosis, net addition of HCO3 back to blood; in alkalosis, negative net acid secretion Most important stimuli for increasing H+ secretion by tubules in avidosis = increase in Pco2 of ECF (respiratory acidosis) and increase in [H+] of ECF (respiratory or metabolic acidosis) o ↑Pco2 -> ↑ H+ formation in tubular cells -> secretion o Excessive aldosterone may increase H+ secretion by intercalated cells (Conn’s syndrome) -> alkalosis o Because of Na/H exchanger, Na reabsorption may 2ndarily increase H+ secretion Via angiotensin II (directly stimulate exchanger) and aldosterone o Hypokalemia stimulates H+ secretion and hyperkalemia inhibits (in proximal tubule) Acidosis -> decreased HCO3:H+ ratio in tubular fluid (excess H+) o Metabolic acidosis -> excess H+ from decreased HCO3 filtration Compensatory response = ↑ ventilation and generation of HCO3 in kidney o Respiratory acidosis -> excess H+ from high ECF Pco2 Compensatory response = ↑ plasma HCO3 from generation in kidney o Chronic acidosis -> increased NH4+ production (raises ECF HCO3 to correct) Alkalosis -> increased HCO3:H+ ratio in tubular fluid (not enough H+) o Respiratory alkalosis caused by ↓ plasma Pco2 (hyperventilation) Compensatory response = increased renal excretion of HCO3 o Metabolic alkalosis caused by rise in ECF [HCO3] Compensatory response = ↓ ventilation and renal HCO3 excretion Respiratory acidosis can occur from damage to respiratory centers (medulla oblongata) or decreased lung CO2 elimination (obstruction, pneumonia, emphysema, ↓ pulmonary memb SA) o Compensate with buffers of body fluids and kidneys Respiratory alkalosis from excess ventilation (psychoneurosis) or high altitude o Compensate with body fluid buffers and kidneys Metabolic acidosis from kidney failure to excrete acids, excess acid formation, ingestion or infusion of acids, or loss of base o Renal tubular acidosis = defect in renal secretion of H+ and/or reabsorption of HCO3 Inadequate amounts of titratable acid and NH4 excreted Causes: chronic renal failure, Addison’s disease, hereditary/acquired disorders (Fanconi’s syndrome) o Diarrhea (most frequent cause of metabolic acidosis) -> loss of large amounts of NaHCO3 o Vomiting of intestinal contents -> loss of HCO3 -> metabolic acidosis o Diabetes mellitus -> fats split into acetoacetic acid -> metabolic acidosis o Ingestion of acids -> acetylsalicylics (aspirin) and methyl alcohol (forms formic acid) o - - - - Chronic renal failure -> buildup of anions of weak acids not excreted, ↓GFR reduces phosphate and NH4 excretion (metabolic acidosis) Metabolic alkalosis o Diuretics (except carbonic anhydrase inhibitors) -> increase flow rate increase Na reabsorption/H+ secretion o Excess aldosterone -> milk metabolic alkalosis (Na reabsorbed, H+ secreted) o Vomiting of gastric contents -> loss of HCl (pyloric stenosis) o Ingestion of alkaline drugs -> NaHCO3 (gastritis or peptic ulcer treatment) To neutralize excess acid -> oral sodium bicarbonate, or IV sodium lactate/gluconate To treat alkalosis -> oral ammonium chloride (liberates HCl) or lysine monohydrochloride Diagnosis of acid-base disorders = o Examine pH (<7.4 acidosis, >7.4 alkalosis) o Examine plasma Pco2 and [HCO3] (normal 40 mmHg, and 24 mEq/L respectively) Expected value for respiratory acidosis: ↓ pH, ↑ Pco2, ↑ plasma HCO3 after renal compensation Expected value for metabolic acidosis: ↓ pH, ↓ plasma [HCO3] and ↓ Pco2 after respiratory compensation Respiratory alkalosis: ↑ pH, ↓ Pco2, ↓ [HCO3} Metabolic alkalosis: ↑ pH, ↑ [HCO3] and ↑ Pco2 Mixed acid-base disorder = 2+ underlying causes for disturbance o Ex. acute HCO3 loss from GI tract diarrhea (acidosis) + emphysema (acidosis) o Diagnosis -> avid-base nomogram (pH, [HCO3}, Pco2 intersect with normal range in middle) Assume sufficient time for compensatory response; within shaded area = simple acid-base disturbance. Outside shaded area = mixed Cation normally measured = Na+ and anions = Cl and HCO3 o Plasma anion gap = [Na] – [HCO3] –[Cl] = 144 – 24 – 108 = 12 mEq/L Used in diagnosing different causes of metabolic acidosis HCO3 changed so Cl must increase to compensate -> hyperchloremic metabolic acidosis HCO3 changed w/o Cl increase, unmeasured anions increased (increased anion gap) -> lactic acidosis or ketoacidosis o Important unmeasured cations = Ca, Mg, K and anions = albumin, PO4, SO4