Regulation of the Menstrual Cycle
advertisement
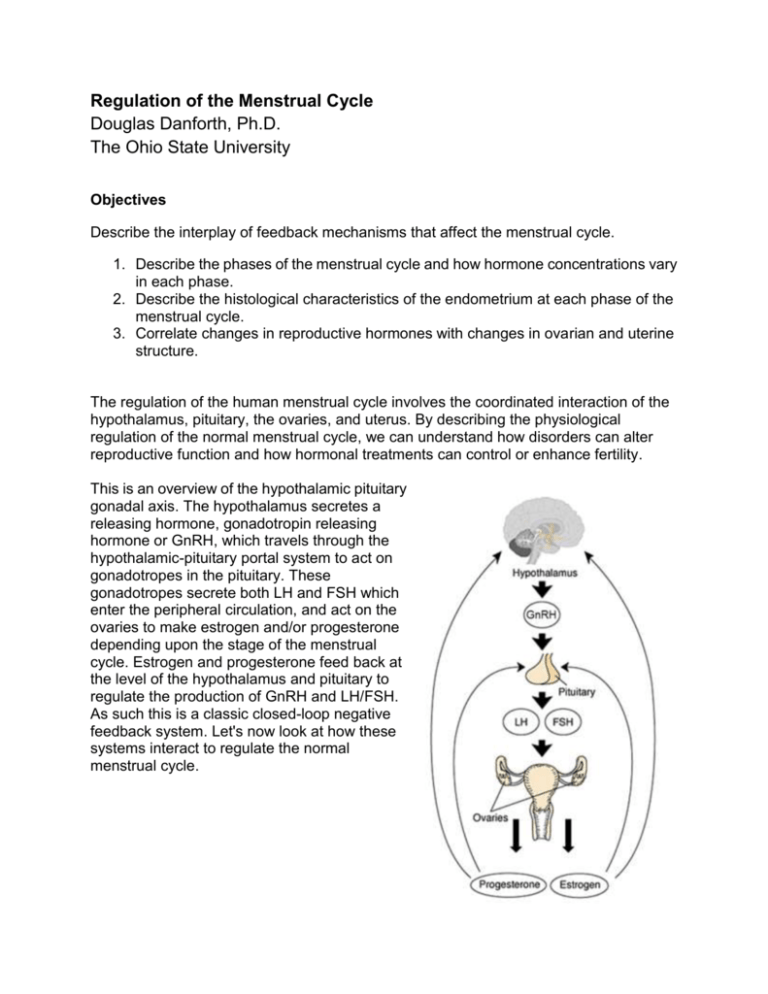
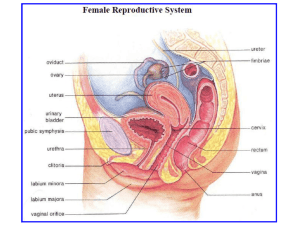
Regulation of the Menstrual Cycle Douglas Danforth, Ph.D. The Ohio State University Objectives Describe the interplay of feedback mechanisms that affect the menstrual cycle. 1. Describe the phases of the menstrual cycle and how hormone concentrations vary in each phase. 2. Describe the histological characteristics of the endometrium at each phase of the menstrual cycle. 3. Correlate changes in reproductive hormones with changes in ovarian and uterine structure. The regulation of the human menstrual cycle involves the coordinated interaction of the hypothalamus, pituitary, the ovaries, and uterus. By describing the physiological regulation of the normal menstrual cycle, we can understand how disorders can alter reproductive function and how hormonal treatments can control or enhance fertility. This is an overview of the hypothalamic pituitary gonadal axis. The hypothalamus secretes a releasing hormone, gonadotropin releasing hormone or GnRH, which travels through the hypothalamic-pituitary portal system to act on gonadotropes in the pituitary. These gonadotropes secrete both LH and FSH which enter the peripheral circulation, and act on the ovaries to make estrogen and/or progesterone depending upon the stage of the menstrual cycle. Estrogen and progesterone feed back at the level of the hypothalamus and pituitary to regulate the production of GnRH and LH/FSH. As such this is a classic closed-loop negative feedback system. Let's now look at how these systems interact to regulate the normal menstrual cycle. These are the sequence of events in the normal human menstrual cycle. 1. At the beginning of the menstrual cycle, designated as Day 1, LH and FSH levels increase. 2. The increase in FSH causes multiple early antral follicles to grow. These follicles secrete estrogen and inhibin. 3. As a result, the levels of estrogen in the circulation increase. 4. From the cohort of growing follicles, one follicle will become selected and become the dominant follicle. 5. This dominant follicle secretes large amounts of estrogen and inhibin. As a result, the circulating levels of estrogen and inhibin increase markedly. 6. The high levels of estrogen and inhibin produced by the dominant follicle, feed back on the hypothalamus and pituitary to decrease circulating FSH levels. 7. At the end of the follicular phase, when estrogen levels have reached their peak, feedback on the hypothalamus switches from negative feedback to a positive feedback event. 8. The positive feedback of estrogen results in a hypothalamic GnRH surge, which triggers an LH surge from the pituitary. 9. The high circulating levels of LH resulting from the LH surge cause three things: a. Oocyte in preovulatory follicle completes meiosis 1 b. Ovulation occurs c. Granulosa and theca cells become luteinized to form Corpus Luteum (CL). The CL secretes large amounts of progesterone (and some estrogen and inhibin). 10. Circulating levels of P, E, and inhibin increase during the early luteal phase and remain elevated for about 10 days. 11. FSH and LH levels are inhibited due to the negative feedback of P, E, and inhibin secreted by the CL. 12. Near the end of the luteal phase (10 – 12 days after ovulation) the CL begins to regress. In humans, the cause of luteolysis is unknown. 13. The regressing CL secretes lower amounts of P, E, and inhibin – thus circulating levels decrease. 14. The decrease in circulating P, E, and inhibin results in loss of negative feedback at the hypothalamus and pituitary, and circulating levels of LH and FSH increase. 15. This cycle ends – the next cycle begins (Step 1) Now that we understand what happens in the hypothalamus pituitary and ovaries throughout the menstrual cycle, let's look at the corresponding changes that occur in the uterine endometrium. Recall that day one of the menstrual cycle is defined as the start of menstruation and the menstrual phase lasts for several days. During this time the endometrium is shed and menstrual flow consists of a mixture of venous blood and endometrial tissue. During the early follicular phase FSH stimulates early antral follicles to accelerate their growth and begin producing greater amounts of estrogen. Estrogen from these follicles stimulates the uterine endometrium to proliferate, and endometrial thickness increases substantially during the follicular or proliferative phase of the cycle. During this phase the endometrial glands are straight and narrow, and secretions from the endometrium and uterine cervix are thin and watery. As the dominant follicle is selected and estrogen levels continue to rise, endometrial proliferation continues until the midcycle LH surge and ovulation. Recall that the primary functions of the LH surge are to 1) cause resumption of meiosis one in the pre-ovulatory oocyte, 2) ovulation of the preovulatory follicle, and 3)corpus luteum formation by luteinizing the granulocyte and theca cells from the preovulatory follicle that remained in the ovary after ovulation. The primary function of the newly formed corpus luteum is to produce progesterone which transforms the proliferative endometrium into a secretory endometrium in preparation for implantation of the embryo. Progesterone causes the endometrial glands to become sacculated and torturous, and along with the cervix they produce a thick and viscous mucus. The appropriate secretions of the secretory endometrium are essential for normal implantation of the developing embryo. In the non-fertile menstrual cycle the corpus luteum produces progesterone for approximately 2 weeks and then regresses. The cause of corpus luteum regression in humans is unclear. As the corpus luteum undergoes luteolysis its production of progesterone declines, and circulating levels of progesterone along with estrogen and inhibin, the other primary hormones of the corpus luteum, decline. This loss of progesterone support to the endometrium causes destabilization of the glands and stroma, and results in sloughing of the endometrium initiating menstruation. The decrease in progesterone, estrogen and inhibin also removes negative feedback at the level of the hypothalamus and pituitary, and circulating FSH levels increase which initiates the start of the next cycle. Let's review what we've learned so far. Normal regulation of the menstrual cycle requires the coordinated interactions of the hypothalamus, pituitary, ovaries, and uterus. The beginning of the menstrual cycle or day one is defined as the start of menstruation. Increased FSH levels at this time result in accelerated follicular growth and recruitment of the follicular cohort. From this cohort of growing follicles one follicle is selected to ovulate and becomes the dominant follicle. This dominant follicle secretes large amounts of estrogen as well as inhibin. Estrogen and inhibin feed back to the pituitary to inhibit gonadotropin secretion. Similarly estrogen acts at the endometrium to stimulate proliferation of the glands of the endometrium. At the end of the follicular phase at midcycle, the dominant follicle secretes high levels of estrogen. This estrogen feedback switches from negative feedback to a positive feedback to initiate the LH surge. It does this by stimulating a GnRH surge. The LH surge does three things: initiates completion of meiosis one in the oocyte of the pre-ovulatory follicle, it causes ovulation of that oocyte, and third it causes luteinization of the granulosa and theca cells of that follicle resulting in corpus luteum formation. The newly formed corpus luteum secretes progesterone for approximately 2 weeks during the luteal phase. The main function of progesterone is to cause a proliferative endometrium to transform into a secretory endometrium in preparation for implantation, should the oocyte be fertilized. Another consequence of elevated progesterone levels is the classic negative feedback at the level of the hypothalamus and pituitary to inhibit gonadotropin secretion. At the end of the luteal phase when the corpus luteum regresses, progesterone levels decline. The fall in progesterone causes destabilization of the endometrium which results in initiation of the menstrual flow. At the same time the decline in progesterone levels reduces negative feedback at the level of the hypothalamus and pituitary, which results in increased FSH production. This increase in FSH stimulates follicular growth and recruitment of the follicular cohort to start the next cycle