How to read a CXR fact sheet
advertisement

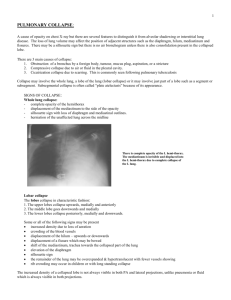
How to Read a CXR Proforma Patient and CXR data: projection, posture Adequacy: easily visible mid-thoracic IV spaces Degree of inspiration – diaphragm at levels of 8th -11th ribs posteriorly (or 5th - 6th ribs anteriorly) Degree of rotation – central spinous processes of thoracic vertebrae, equidistant from medial ends of clavicles Airway: Trachea: central; slight deviation to R as crosses aortic arch Pushed away: large pleural effusion; large/tension pneumothorax; aortic aneurysm; mediastinal mass Pulled towards: collapse; pul fibrosis; lobectomy, pneumonectomy Breathing: Lungs, Pleura (effusion, thickening, calcification) Lung outlines: look for pneumothorax, bullae, collapse, consolidation, effusions, masses, pleural changes; on lateral view lung lucency should increase towards diaphragm Increased lucency towards diaphragm = COPD, pneumothorax Decreased lucency towards diaphragm = alveolar / interstitial fluid, effusion, Consolidation Air bronchogram: tubular outline of an airway made visible by filling of the surrounding alveoli by fluid or inflammatory exudates Caused by: lung consolidation; pulmonary edema; nonobstructive pulmonary atelectasis; severe interstitial disease; neoplasm; normal expiration Circulation: Heart: 1/3 to R of thoracic spinous processes, CTR <50% R heart border = RA; Poor distinction = consolidation of RML L heart border = LV; Poor distinction = lingular consolidation Increased CTR = AP film; LVD, CCF, pericardial effusion Pulmonary vessels Diaphragm: R higher than L by 1-3cm Loss of outline = fluid, consolidation or collapse Flat diaphragm = COPD Gas under diaphragm = rupture of hollow viscus; Post-laparoscopy Mediastinum: Hila: at T6-7 level; made of pul arteries and veins; L hilum 1-2cm higher and square shaped; R hilum V shaped Width: <8cm superiorly on PA at carina (or >25% diameter of chest) Wide: AP view; unfolded aortic arch, thoracic AA, aortic rupture; mediastinal lymphadenopathy; retrosternal thyroid, thymoma; paravertebral mass; oesophageal dilation Bones: lesions or fractures Soft tissues: don’t miss mastectomy Tubes Views Describing abnormalities: mediastinal / central / peripheral; UZ/MZ/LZ (according to lobe if lateral film available); number; size; shape; effects on adjacent structure PA: Preferred view Transverse fissure: from Jx of upper 1/3 and lower 2/3 lateral chest to R hilum Lat: Helps delineate and localize masses, lesions or consolidation – esp if they are obscured by heart and diaphragm L image, L lung: oblique fissure, as shown from T4 to 3cm post to where diaphragm and sternum meet R image, R lung: horizontal and oblique fissures, as shown ÂP: Magnifies heart and mediastinum Associated with rotational artefact Expiratory: helpful for small pneumothroax / gas trapping with FB Neonatal CXR Atelectasis Consolidation Lobe collapse Heart 60-65% chest width Bronchial branching may give sense of air bronchograms Thymus (involution occurs age 6yrs; not usually seen after 2yrs; is anterior on lateral; L lobe larger than R; extends as low as 4th costal cartilage; lung markings visible through it; does not displace trachea) Neonatal RDS: miliary nodulation in lower zones / diffuse; ground glass; air bronchogram CF: bronchiectasis, peribronchial consolidation Varicella pneumonia: widespread nodules Collapse or incomplete expansion of the lung or part of the lung segmental/subsegmental collapse linear/curvilinear/wedge-shaped increased density with apex at hilum; often assoc with volume loss; shift towards; may be compensatory hyperinflation of adjacent lobes, or hilar elevation / depression; air bronchogram can occur Compression: In lumen: mucus plug In wall: tumour, scarring, TB, post-radiation Extrinsic: LN’s, pleural effusion Describe: homogenicity, discreteness of margin, cavitation, effect on heart border Fluid (inflammatory, aspiration, pneumonia) Cells (bronchoalveolar Ca, sarcoidosis, lymphoma) Protein (alveolar proteinosis) Blood (pul haemorrhage – Goodpastures, high altitude, bleeding disorders, mitral stenosis) Silhouette sign: Silhouette of heart borders, a’ing and d’ing aorta, aortic knuckle and hemidiaphragms should be clearly visible; obliteration of any of these borders suggests pathology Note, pathology in posterior pleural cavity and lower mediastinum cause overlap but not obliteration of heart border Look for: loss of vol of lobe, loss of lucency, displacement of fissures, wider spacing of vascular shadows of rest of lung LUL collapse Loss of aortic knuckle and upper L heart border Retrosternal band of opacity with well defined oblique fissure on lateral LLL collapse RUL collapse Loss of L hemidiaphragm and descending aorta Triangular opacity between heart shadow and spine on lateral Loss of ascending aorta and upper R heart border Opacity at RUZ apex of mediastinal border Deviation of trachea to R RML collapse: Loss of R heart border (vague R pericardiac haze) On lateral, 2 fissures start to approximate (depression of horizontal) causing wedge opacity pointing to hilum RLL collapse: R heart border unaffected Triangular density posteromedially Loss of R hemidiagphragm Lingular consolidation: loss of L heart border Pneumonia Interstitial lung disease SHITFACED Airspace opacity / lobar consolidation / interstitial opacities Normal/incr volume (volume loss NOT seen); no shift; not centred at hilum; can cause air bronchograms Lobar: strep pneumoniae; uniform opacity confined to one lobe; air bronchograms seen; may be ill defined if not adjacent to one of the fissures; may be small assoc pleural effusion Lobular: staph; multifocal, patchy Lower zones: legionella Upper zones: klebsiella Round pneumonia: C Burnetti, S pneumoniae, L pneumophilia, S aureus Bronchial: ill defined areas of patchy opacity (eg. Post-op, aspiration) Diffuse: community acquired, nosocomial, Immunocompromised Miliary pattern / intersitital: TB, varicella pneumonia; air bronchogram not seen Sarcoidosis Histiocytosis Idiopathic Tumour: mets, lymphangitis Failure Autoimmune: SLE, RA, scleroderma, polymyositis; granulomatosis; hypersensitivity pneumonitis Collagen vascular disease Environmental: Asbestos, silicosis, farmer’s lung, coal Drugs: Methotrexate, amiodarone Other: atypical pneumonia, fungal, viral; radiation pneumonitis Lung asbcess Bacterial: staph aureus, Klebsiella, anaerobes, G-ives, TB, aspiration pneumonia; bronchial obstruction; if multiple, think of R sided bacterial endocarditis Fungal (eg. Aspergillosis, cryptococcal) If assoc with pleural effusion: staph aureus, anaerobes, Gives, TB Immuncompetent: anaerobes more common Immunocompromised = staphs 2-10% mortality if community acquired, 60% if hospital acquired; shows AF level (present if communicates with bronchioles; dense area of consolidation if doesn’t and will need CT to diagnose) Cavitating lung lesions CAVITY Cancer: more likely if anterior; esp if SCC; advanced Hodgkins Autoimmune: granulomatosis, sarcoidosis, Wegener’s RA, progressive massive fibrosis Vascular: septic emboli and pul infarct Infectious: 2Y TB, abscess, cocci, infected bullae / cysts TB Pleural effusion ARDS PE Trauma: traumatic cyst Young: bronchogenic cyst, laryngotracheal papillomatosis 1Y small area consolidation in lower UL or upper LL, adenopathy, pleural effusion Post-1Y TB hilar LN calcification, small calcified nodule (Ghon focus) 2Y cavitating lung lesions with surrounding fibrosis (esp in UL with elevation of hila and incr lucency of remaining lung fields), focal patchy airspace disease, no hilar lymphadenopathy Miliary 1-2mm diffuse nodules Erect: blunting CP angle (lateral on PA, posterior on lat); >100ml to see on PA, 75ml to see on Lat; upper margin should be concave – if flat, also pneumothorax; can cause tracheal shift (unlike consolidation) Supine: graded haze, denser at base; vascular shadows can be seen through effusion; if large, fluid cap over apex; do lateral decubitus Causes: CCF, infection, trauma, PE, tumour, autoimmune disease, renal failure; if large, more likely Ca R sided – Meig’s syndrome (ovarian Ca) L sided – pancreatitis, chylothorax, CCF Bilat pul infiltrates with air bronchograms occuring after 12hrs clearing after 5/7 fibrosis with reticular pattern after 7/7 Westermark’s sign (oligaemia in area of involvement); Hampton’s hump Increased size of hilum (thrombus impaction); Atelectasis with elevation of hemidiaphragm and linear densities; Pleural effusion; Consolidation CCF Upper lobe diversion (upper lobe vessels usually smaller than lower), basilar and hilar infiltrates, widening of vascular pedicle, peribronchial cuffing, Kerly B lines (also found in silicosis, lymphagnitis carcinomatosis, sarcoidosis), CTR >0.5 (>0.7 in infants), pleural effusions; XR more sens than examination Pulmonary nodules Benign: unchanged for two years is almost certainly benign; completely calcified or central or stippled Calcium; solitary Suspicious: nodules with irregular calcifications or those that are off center; Multiple nodules; 1Y tumours don’t calcify, may have satellite lesions; 1Y poorly defined; may show umbilication; may have linear strands connecting to hilum (lymphatics), usually double in size in 1-6/12 Solitary pul nodule: 30-40% malignant; <3cm Adenoma: usually central, hilar, smooth and round; 1% of all neoplasms Neoplasia: assoc with collapse, hilar enlargement, elevated hemidiaphragm, bony destruction, lines lymphatic infiltration with connects to hilum Mets: usually more sharply defined than 1Y; multiple; colon, breast, renal cell, testicular, TCC, melanoma If diffuse rather than nodular: prostate, stomach, pancreas, lymphoma, thyroid If calcify: breast, osteogenic Ca, thyroid, ovarian, mucinous adenoCa Adenocarcinoma (35-50%): peripheral Emphysema Pulmonary fibrosis SCC (30%): central, hilar involvement, cavitation common Small cell (15-20%): central; hilar and mediastinal masses Large cell (10-15%): peripheral; large; cavitation present Bronchoalveolar (3%): peripheral; rounded; air bronchograms Carcinoid (<1%): well-defined endobronchial lesion Other: lymphoma Infection (round pneumonia (esp children and young adults; C Burnetti, S pneumoniae, L pneumophilia, S aureus); atelectasis; abscess; miliary TB (cavitation, calcification), varicella pneumonia, histoplasmosis, aspergilloma, fungal, Nocardia infection, hydatid disease Vascular: AVM, haemartoma (smooth 2-4cm lobulated with popcorn calcification), PE, infarct Autoimmune: more likely multiple; granuloma, RA, Wegener’s, fibrotic lung disease (eg. Silicosis) Other: pleural plaques, bronchial atresia, sequestration, chrondroma Hyperinflation with flattening of diaphragms; Increased retrosternal space; Bullae (have no vessels and are not perfused); Enlargements of PA / RV; reduced vascular markings esp in periphery; long thin heart, clockwise rotation of heart; kyphosis and sternal bowing Ground-glass (suggests idiopathic) / reticular appearance; volume loss with linear opacities bilaterally; multiple nodules Honeycomb lung; SETCARP Upper zone (SETCARP): Silicosis (multiple nodules, hilar LN with egg shell calcification) Sarcoidosis (mediastinal > paratracheal nodes, calcification rare, miliary nodulation and large nodules) Eosinophilic pneumonia TB Coal miner’s pneumoconiosis, CF Aspergillosis, ank spond Radiation therapy PCP, pneumoconiosis BADRASH Lower zone (BADRASH): Bronchiectasis Aspiration Drugs RA Asbestosis (shaggy heart from adhesions, pleural thickening and calcification, mesothelioma) Scleroderma Hamman Rich syndrome, histiocytosis BIGHIPS Honeycomb (BIGHIPS): Bleomycin Idiopathic Granulomas Histiocytosis Interstitial pneumonia Pneumoconiosis Sarcoid Drugs (methotrexate, nitrofurantoin, hydralazine, amiodarone), paraquat, smoke inhalation, ARDS Pneumothora x Etched diaphragm (1) / mediastinum (2) : contrasted with air in pleural space; diaphragm may be flattened Deep sulcus sign (3): abnormally prominent/deep lateral CP angle Visible visceral pleura (4), Mediastinal / tracheal shift, Uneven lung density, Absent lung markings, subC emphysema DD: scapula, skin fold, bullae, companion shadow, post-pleurectomy, drain tube track line Pneumomediastinum Hydropneumothora x Streaky lucencies over mediastinum extending into neck Elevation of parietal pleura along mediastinal borders Causes: Asthma, whooping cough, surgery, traumatic tracheobronchial rupture, abrupt changes in intrathoracic pressure (eg. coughing, vomiting), ruptured oesophagus, barotrauma, cocaine Trauma, thoracentesis, surgery, ruptured oesophagus, empyema Mediastinal masses Pleural masses MALLETS Extra-pleural masses Pericardial effusion Ant: between heart and sternum Upper: LN’s, thyroid mass Middle: LN, ascending aortic aneurysm, thymus, teratoma, lipoma Lower: fat pad, pericardial cyst, hernia Middle: LN; Aortic aneurysm; pul art; Bronchogenic cyst Post: between heart and spine Upper: pharygneal pouch, neurogenic tumour Middle: hiatus hernia, dlated oesophagus, descending aoric an. Lower: hernia, neurogenic tumour, TB of spine, Hodgkins Are broad based to chest wall, usually 2Y Mesothelioma Adenocarcinoma, asbestosis Lymphoma, Leukaemia Empyema (or loculated pleural effusion) Thymoma Splenosis Rib tumour; Rib infection Neurofibroma / schwannoma; Lipoma Globular enlarged heart shadow; 400-500ml fluid present to be seen on CXR (200ml for pleural effusion) Fat pad sign: soft tissue stripe >2mm between epicardial fat (blue arrows) and ant mediastinal fat (red arrows) seen anterior to heart on lateral view Hilar lymphadenop athy Inflammation (sarcoidosis, silicosis) Neoplasm (lymphoma, metastases, bronchogenic carcinoma) Infection (TB, histoplasmosis, infectious mononucleosis) May be vascular disease (eg, pul HTN – will have more smooth border) Notes from: See p 490 TinTin for non infectious causes of pul infiltrates