I really appreciate your great reviews. Even though there were many
advertisement
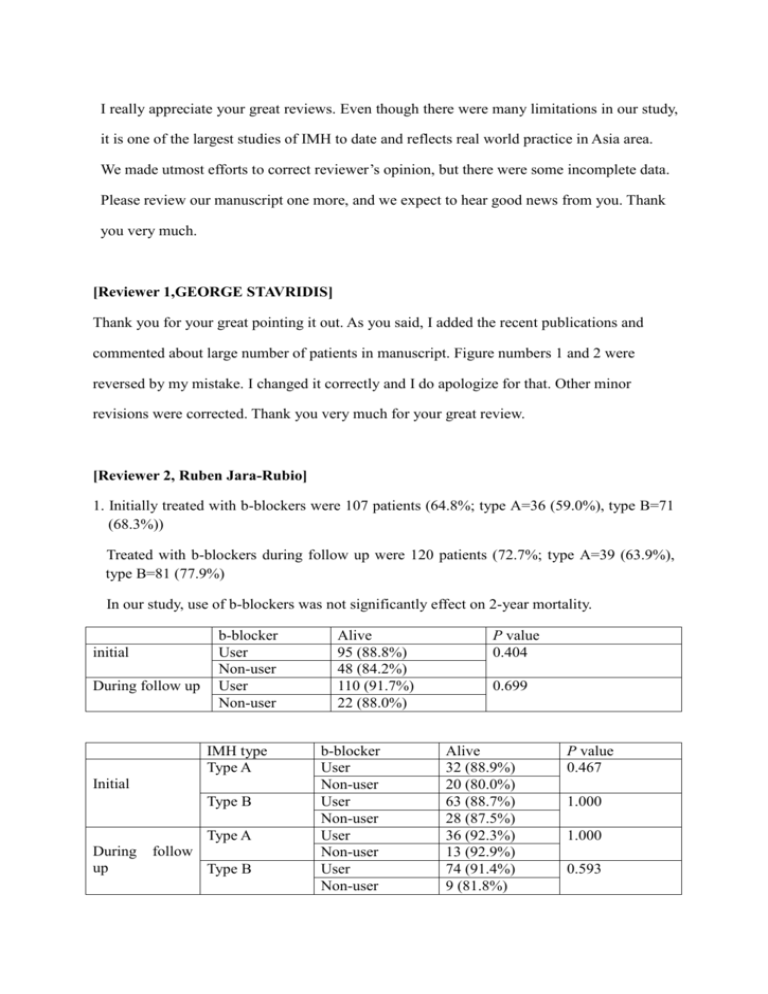
I really appreciate your great reviews. Even though there were many limitations in our study, it is one of the largest studies of IMH to date and reflects real world practice in Asia area. We made utmost efforts to correct reviewer’s opinion, but there were some incomplete data. Please review our manuscript one more, and we expect to hear good news from you. Thank you very much. [Reviewer 1,GEORGE STAVRIDIS] Thank you for your great pointing it out. As you said, I added the recent publications and commented about large number of patients in manuscript. Figure numbers 1 and 2 were reversed by my mistake. I changed it correctly and I do apologize for that. Other minor revisions were corrected. Thank you very much for your great review. [Reviewer 2, Ruben Jara-Rubio] 1. Initially treated with b-blockers were 107 patients (64.8%; type A=36 (59.0%), type B=71 (68.3%)) Treated with b-blockers during follow up were 120 patients (72.7%; type A=39 (63.9%), type B=81 (77.9%) In our study, use of b-blockers was not significantly effect on 2-year mortality. initial During follow up b-blocker User Non-user User Non-user IMH type Type A Initial Type B Type A During up follow Type B Alive 95 (88.8%) 48 (84.2%) 110 (91.7%) 22 (88.0%) b-blocker User Non-user User Non-user User Non-user User Non-user P value 0.404 0.699 Alive 32 (88.9%) 20 (80.0%) 63 (88.7%) 28 (87.5%) 36 (92.3%) 13 (92.9%) 74 (91.4%) 9 (81.8%) P value 0.467 1.000 1.000 0.593 2. Yes, all patients enrolled in this study were Asian race. 3. 20 patients (32.8%) with type A IMH had pericardial effusion. Among them, 6 patients were initially treated surgically and 1 patient had timely surgery after initial medical treatment. Total of 7 patients with surgically treated, 1 patient died during hospitalization and others were alive during 2-year follow up. The rest of 13 patients who were treated medically even though presence of the pericardial effusion, 1 patient died suddenly during hospitalization and 2 patients died during follow up. So, the mortality rate were 14.3% in surgically treated group and 23.1% in medically treated group in patients with pericardial effusion (P = 1.000). I’m sorry that we didn’t measure the amount of pericardial effusion and cardiac tamponade or not. However, among 20 patients, there were 3 patients who showed shock (initial systolic BP < 90mmHg) and they treated medically without operation. They survived until follow up period. 4. In our study, 22 patients (36.1%) with type A IMH had large aortic diameter (>50mm). Among them, 9 patients were treated surgically and all patients were alive. However, among 13 patients with medical treatment, 2 patients died during hospitalization and another 2 patients died during follow up period. Therefore the mortality rate were 30.8% in medically treated group and 0% in surgically treated group in patients who had large aortic diameter (>50mm) (P = 0.115). Other minor revisions were corrected according to your opinion. Thank you very much for your great review. [Reviewer 3, MATTHEW PANAGIOTOU] Major 1. As shown in manuscript, admission duration was longer in emergency surgery group than medical therapy and timely surgery group (Type A; 29 ± 14 vs. 16 ± 8, P = 0.008 Type B; 26 vs. 17 ± 13, P = 0.492). Even though, hospital costs of these two different therapies can’t know exactly, shorter admission duration and reduction of operation charge can reduce total hospital costs in patients with medical therapy and timely surgery. And as you pointed out, we changed final conclusion. Minor 1. Thank you for your good point. I changed the results correctly. 2. I added sentences “in some cases”, as you pointed out medical therapy is not enough to manage all patients with type A IMH and many studies try to find out prognostic factor and build criteria for surgical treatment. 3. As we mentioned in manuscript, low rates of CT follow-up were limitation of our study. Because it was a retrospective analysis, it can’t be helped. I do apologize for that. 4. The 2 years mortality of surgery is 7.2%. Only 1 patient died out of 14 who were operated on (Total number was not 18). 5. 11 patients of type A IMH group progressed to aortic dissection in 2 years. Among them, 3 patients were treated with operation and 2 patients died. Others were left untreated with chronic dissection without symptoms. In type B group, 8 patients progressed to aortic dissection and 1 patient underwent operation. The patient died because of postoperative bleeding. Others were left untreated with chronic dissection without symptoms. [Reviewer 4, PIERLUIGI L STEFANO] Major 1. I really apologize for my mistake about some reversed data in abstract. I changed it correctly and added recent publications as you point out. Minor 1. I added acronym in tables and figures. Figure numbers 1 and 2 were reversed and I correct it to right. 2. Surgical techniques include aorta graft replacement (20 cases) and Hybrid EVAR (1 case).