348WHO DG Message at IFRC Side Event in Rio
advertisement
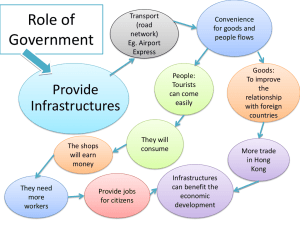
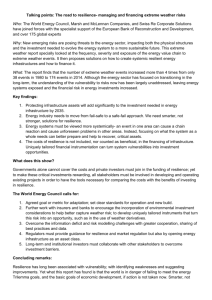
Local action and partnerships for more resilient people and communities (IFRC, UNDP, World Bank) 2010 was a watershed year. The mega-disasters in Haiti and Pakistan opened the eyes of the world to the impact of natural disasters on vulnerable populations. Despite massive international assistance, neither country has fully recovered. Those events had three main consequences 1. International assistance must become much faster, better coordinated, and more closely aligned with priority needs, with constant quick adjustments in strategies and approaches. It must be prepared to gear up quickly to respond to the unexpected, like the cholera outbreak in Haiti. 2. Efforts must be made to strengthen resilience and reduce vulnerability. Earthquakes and floods that same year in other places, with well-functioning infrastructures, also for health, were far less destructive, deadly and socially disruptive. 3. The international community must anticipate more of these mega-disasters as the climate changes. It must also anticipate large population displacements and the likelihood of “environmental refugees”: people who cannot return home because the land is scorched or flooded. 1 Fortunately, many of the newer initiatives for international health development have capacity-building as a built-in objective, with well-designed strategies for channeling assistance in ways that strengthen existing infrastructures and services, including the capacity to generate and interpret basic health data. Accountability means counting. Without basic health information, we are pouring money into a black hole. At a time when money is extremely tight, the momentum for better health will continue only when we can clearly demonstrate that investments bring results. Another trend, that became starkly obvious last year, compels the health and development community to invest in the strengthening of basic health infrastructures, ideally with the goal of reaching universal health coverage. Last year’s events included the Arab spring and protests all around the world expressing intolerance of vast and growing social inequalities. These events opened the eyes of the world to the dangers of inequality. It can topple governments and destabilize large geographical areas. As we also learned last year, discontent is contagious, fuelled in part by easy access to social media. Universal health coverage is a powerful equalizer. 2 A well-functioning health system, with equitable financing that protects against catastrophic medical bills, promotes social cohesion and stability. As numerous studies show, health outcomes are best when equity and fairness are explicit policy goals, regardless of the level of per capita spending on health. In other words, money alone will not buy better health. Policies that aim for fairness have a much better chance. Equity must also extend to schemes for social protection and health insurance. Lack of access to health services impoverishes people because they cannot work when ill or debilitated by disease. Using health services impoverishes people because, lacking any form of health protection, they pay bills out of pocket or by selling off a household asset, sinking them even deeper into poverty. 460 words Facts Annual government expenditures on health range from as little as $1 per person to nearly $7,000. The difference in life expectancy between the richest and poorest countries now exceeds 40 years. An estimated 2.7 billion people live in countries with no safety net to cover medical costs. 3 Some 85 countries, representing 65% of the world’s population, do not have reliable cause-of-death statistics. This means that causes of death are neither known nor recorded, and health programmes are left to base their strategies on crude and imprecise estimates. In 2012, more than 50 million people in 16 countries are expected to require humanitarian assistance. Hospitals and clinics are the backbone of community resilience when disaster strikes. Access to new “clean energy” technologies can help these facilities continue to function during emergencies, when they are needed most. 4