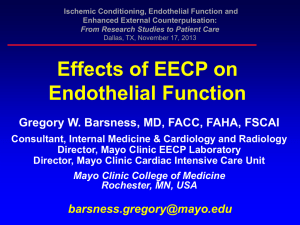
EECP Articles
advertisement

EECP as a Noninvasive Treatment of Endothelial Dysfunction Cross section of an artery showing a monolayer of endothelial cells lining the inner wall of the artery. The arterial wall is composed of smooth muscle cells and collagen. By John CK Hui, Ph.D. Introduction Over the past 30 years, endothelium has emerged as the key regulator in the initiation and progression of 1-4 cardiovascular disease. The endothelium is the monolayer of endothelial cells lining in the direction of blood flow along the lumen of all blood vessels. The endothelial cells function as a protective barrier and facilitate bi-directional transport of macromolecules and blood gases between all tissues and circulating blood. Endothelial cells also control vasomotor function, regulating vasodilatation and vasoconstriction by 5,6 the release of nitric oxide (NO) and endothelin-1 (ET-1). These neurohomonal factors play a vital role in hypertension, reduction of oxidative stress and arterial stiffness. Vascular endothelium is also responsible for the regulation of angiogenic vascular remodeling, metabolic, anti-inflammatory, and anti-thrombogenic processes. Endothelial cells also play a critical role in the process of atherosclerosis, leading to coronary, renal and peripheral artery disease. Endothelial dysfunction initiates expression of endothelial adhesion molecule-1 and monocyte chemoattractant protein-1 which incorporate circulating macrophage monocytes and Tcells into the subendothelial space, changing them into macrophage foam cell, while at the same time promoting smooth muscle cell proliferation and migration, and increased platelet activity and coagulation, leading to thrombosis, atherogenesis and neointimalization. Enhanced External Counterpulsation (EECP) ® An EECP therapy system consists of three sets of inflatable pressure cuffs wrapped around the calves, the lower and upper thighs, including the buttocks. The cuffs are rapidly and sequentially inflated, starting from the calves and proceeding upward to the buttocks during the relaxation (diastolic) phase of each heartbeat, creating a strong arterial retrograde flow towards the heart and significantly increasing blood flow to the coronary arteries at a time when resistance to coronary blood flow is at its lowest level. The inflation of the cuffs also simultaneously increases the volume of venous blood returned to the right side of the heart, providing greater filling of the ventricle for ejection. Just before the beginning of the next cardiac cycle when the heart begins to contract, all three cuffs simultaneously deflate, leaving an empty vascular space in the lower extremities to receive blood ejecting from the heart, thereby significantly reducing the workload of the heart. The inflation/deflation activity is monitored constantly and coordinated by a microprocessor that interprets electrocardiogram signals, monitors heart rhythm and rate information, and actuates the inflation and deflation in synchronization with each cardiac cycle. The inflation/deflation cycle is repeated every heartbeat, increasing energy supply to the heart, improving cardiac output, while at the same time reducing the workload of the heart. The QRS complex of the electrocardiogram is used to provide a triggering signal for the calf inflation valve to open around the peak of T-wave, the lower thigh valve will open 50 ms later, to be followed by the upper thigh valve another 50 ms later. The pressure in the cuffs will hold as long as possible to allow maximization of diastolic augmentation. Then all threedeflation valves will open at the same time around the peak of P-wave to let the emptied peripheral vasculature to receive the blood ejected by the heart, leading to systolic unloading. ® There are many pathophysically pathways by which EECP therapy achieves its long-term clinical 7 beneficial effects. There is evidence of improved endothelial function via the hemodynamic effects of increased shear stress on the arterial wall, reducing arterial stiffness and providing protective effects against inflammation, thereby inhibiting intimal hyperplasia and atherosclerosis. There is also evidence suggesting that EECP therapy triggers a neurohomonal response by improvement of endothelial function that induces the production of growth and vasodilatation factors, which together with the hemodynamic ® effects of increasing pressure gradient across the occlusive site during EECP therapy, promotes the recruitment of new arteries, while exisiting blood vessels dilate and normalize in function. The recruitment of new arteries, known as “collateral blood vessels”, bypasses blocked or narrowed vessels and increase blood flow to ischemic areas of the organs that are receiving an inadequate supply of blood. A summary of the proposed mechanisms of action of EECP therapy is shown in the following diagram: ® EECP Therapy: Mechanisms of Action Acute Hemodynamic Effects Increase shear Stress Systolic Unloading Diastolic Augmentation Increase Cardiac Output Improve Endothelial Function Vasodilation: NO↑ ET-1↓ Vascular resistance ↓ Arterial Stiffness ↓ Intimal Hyperplasia ↓ Circulating Endothelial Progenitor Cell ↑ Angiogenesis: microvascular density↑ Proinflammatory Cytokines and Adhesion Molecules: TNF-α↓, MCAP– 1 ↓ Reduce hypertension Improve Blood Flow Reduce atherosclerosis Clinical Benefits: Sequential inflation of three sets of cuffs at the end of systole Lower ThighCuffsUpper Thigh CuffsCalfSimultaneous deflation of all three sets of cuffs at the end of diastole Lower ThighUpper ThighCuffsCalf Published clinical data showing effectiveness of EECP therapy in improving endothelial dysfunction Historically, an external counterpulsation (ECP) device is a cardiac assist device that reduces the workload of the heart and increases energy supply to the myocardium. The objectives of ECP devices are the maximal reduction of systolic blood pressure so that the heart does not have to generate high pressure to eject the volume of arterial blood for the metabolic need of the body, and maximal augmentation of diastolic pressure to increase coronary perfusion pressure to increase coronary blood flow when resistance to coronary flow is at its lowest level. The optimal ECP operation is to achieve the maximization of the ratio of the area under the diastolic pressure to the area under the systolic pressure. 1. Acute hemodynamic effects of EECP (Enhanced External Counterpulsation): Increase cardiac output and coronary blood flow The physiological and clinical goal of EECP is the improvement of cardiac function and increase of cardiac output, as demonstrated by the increase of velocity of blood flow in the descending aorta using 8,9 Doppler echocardiography. Systolic time velocity integral as a measure of stroke volume (SV) increased up to 60-70% over control with the heart rate (HR) remaining stable, demonstrating a significant increase in cardiac output. EECP also created a significant diastolic retrograde blood flow, generating a bidirectional pulsatile fin the descending aorta, increashear stress on the endothelium. EECP also resulted in a dramatic increase in intracoronary pressure and intracoronary flow velocity 10 measured by using a coronary catheter sensor-tipped guidewire. Coronary diastolic pressure increased 93% from 71 10 at baseline to 137 ± 21 mm Hg durinEECP, p<0.0001; with a decrease icoronary systolic pressure of 15%from 116 ± 22 to 99 ± 26 mm Hg, p=0.002. The intracoronary average peak velocity increased 109% from 11 ± 5 at baseline to 23 ± 5 cm/sec during EECP, p=0.001. The signific inDescending Aorta ControlDuring EECP Stroke volume Diastolic retrograde flow Doppler echocardiography of the descending aorta 2. Effects of EECP pulsatile blood flow: increase endothelial shear stress Endothelial shear stress flowing blood on the endothelial surface of the arterial wall and is expressed in un 2222 tress is proportional to the product of the blood viscosity (μ) and the spatial gradient of blood velocity at the wall. Low endothelial shear stress modulates endothelial gene expression through complex mechanoreception and mechanotransduction processes, inducing an atherogenic endothelial phenotype 11 and formation of an early atherosclerotic plaque. Therefore the significant increase of pulsatile, oscillatory flow in the aorta durEECP treatment provides a form of “massage” on the endothelium and improves its function. Effect of EECP on endothelial shear stress has been reported in an animal moZhang in 112 ultrasound system during EECP in thebrachial artery was significantlcompared with the pre-EECP measurement (24.62±4.74 versus 59.48±13.60 cm/sec, p<0.001). Theinternal diameter (id) of the right brachial artery was not significantly changes durinEECP (1.65±0.42 versus 1.68±p<0.05). The blood viscosity (μ) wa3.8±0.4 mPa (0.038±0.004 poise). Thpeak diastolic endothelial shear stress (τ) d τ 2 (dynes/cm ) = (4 μ V) / (id) Peak diastolic endothelial shear stress during EECP increased more then 23. Blood vessels vasodilate in response to an increase of flow through rather to the endothelial shear stress. Conversely, low shear stress leads to const remodel vasodilation occurs in the earliest stages of atherosclerosis, and this endothelial dysfunction is now considered to be the link between such risk factors as dyslipidemia, hypertension, diabetes mellitus, cigarette smoking, hyperhomocysteinemia, and aging to cardiovascular disease. 13,14 The endothelial response to shear stress activates a varietysignaling pathways, including endotheoxide synthase (eNOs), an enzyme rethe synthesis of nitric oxide (NO), the key endothelium-derived relaxing factor that plays a† p< 0.05 versus CHOL group 150200eNOs (% of control) †eNOs ring EECP was calculated using the formula: 10.71 dynes/cm2; p<0.001). tone and reactivity. EECP has been shown to increase the expression of eNOs by Zhang and co-workers in a hypercholesterolemic pigs 12 model using Western blotting technique. Expression of eNOs was significantly decreased in the group of pigs (N=28) fed with high-cholesterol diet for 15 weeks compared with the 7 pigs with normal diet served as control (p=0.009). 1 hour daily of EECP for 34±2 hours was initiated in 17 pigs after 8 weeks of atherogenic diet and eNOs expression of the EECP treated group was 3.16 times that of thecholesterol group (p=0.023). 4. EECP therapy increases the release of nitric oxide and reduces. In response to endothelial shear stress, Nitric Oxide (NO) is synthesized in th In addition, NO also inhibits platelet and white cell activation and maintains the vascular smooth muscle cells in a nonproliferative state. More importantly, NO interacts with products of oxidative stress such as superoxide and hydrogen peroxide. Oxidative stressproduced from any cardiovascular risk factors is one of the leading causes of endothdysfunction. EECP 16 published later in 2006. This study examined whether the flow mediated increase in endothelial shear stress would activate plasma levels of the potent vasoactive agents ET-1 and NO. Thirteen coronary disease patreceived 1-hour daily EECPtreatment for a total of 36 hourand their ET-1 and NO were measured serially at baseline (Control), after the 1st, 12th, 24and 36th hours of EECP, and at 1 and 3 months post-EECP. During the course of treatment, plasma NO progressively increased and plasma ET-1 progressively decreased. After 36 hours of EECP, there was a 62 ± 17% increase in plasma NO compared with baseline (43.6 ± 4.27.1 ± 2.6 μmol/L; p<0.0001),a 36 ± 8% decrease in plasm1 level (76.7 ± 9.5 versus 119.8.5 pg/L; p<0.0001). At 3 months after completion of EECP, NO remained 13 ± 11% above baseline (p=0.002), and ET-1 remained 11 ± 10% below baseline (p=0.0068). These results demonstrate that EECP therapy has a dose related, sustained effect in stimulating endothelial cell production of the vasodilator, NO, and in deceasing production of the vasocontrictor, ET-1, supporting the hypothesis that EECP improves endothelial function. In another study, Masuda and colleagues demonstrated that EECP significant increased plasma NO levels compared with baseline in 1patients with chronic stable anginthe day after the start of EECP, and 1 week, 1 month after completion of35 hours of 17 daily 1-hour EECP treatment (p<0.02). The treadmill exercise time, time to 1 mm ST-segment depression, perfusion in ischemic regions of the myocardat rest and during dipyridamole stress measured 11 by N-ammonia positron emission tomography inthese patients also improved signifendothelial function via increase oto the observed clinical benefits of EECP treatment. There are s with endothe 18,19 follow-up compared with patients with preserved endothelial function. More importantlythe observation that an intervention improves endothelial function in a group of patients suffering from cardiovascular 20 disease suggests that the intervention will also reduce cardiovascular risk. Currently the most promising noninvasive endothelial function testinthe endothelial-dependent, flow-mediated dilation of the brachial artery using high-resultrasound. In 2003 that improvement in per 21 EECP treatment in patients with symptomatic coronary artery disease (CAD). Reactive hyperemiaperipheral arterial tonometry (RH-PAT), a noninvasive method to assess peripheral endothelial function by using a device manufactured by Itamar Medical in measuring reactive hyperemic response in the finger (Endo PAT 2000, FDA 510k032was performed in 23 patients with refractory angina undergoing a 1-hour daily EECP total course of 35-hour treatment. In each patient RH-PAT measurements were performed th before and after the first, at midcourse (17 hour), and after the last EECP course. In addition, RH-PAT response was assessed one month after completion of EECP therapy. RH-PAT index, a measured of reactive hyperemia, was calculated as the ratio of the dpulse volume during reactive hyperemia divided by that at rest. EECP was associated withsignificant immediate increase in average RH-PAT index after each treatment period (p<0.05). In addition, average RH-PAT index at one-month follow-up was significantly higher than that before EECP therapy (p<0.05), demonstrating EECP therapy provided long Nitric Oxide measured by the Griess method in 11 CAD patients. Control: before EECP therapy. Next day: 1 day following completion of 35hour course of therapy. 1 week: 1 week after completion of therapy , and 1 month: 1 month after completion. # p<0.02 vs control, and p<0.01 vs next day. improvement of endothedysfunction in patieCAD. No major adverse cardiovascular evennoted during the study perio In addition to RH-measurement of endothelial function, Canadian Cardiovascular function (CCS) class and Duke Activity Status Index (DASI) score were uassess the clinical benefEECP therapy. EECP therled to an improvement by oCCS class in 12 (52%) patients and by two CCS class in 5 (22%) patients, whereas 6 (26%) patients showed no change in CCclass. in this study, 74% experience an improvement in their functional status. Similarly, 17 (74%) patients reported improvement in their functional status, as measured by the DASI score. Moreover, average RHPAT before initiation of EECP therapy and one month after completion of therapy significantly increased only in patients showing improvement functional CCS class or DASI score. Patients failed to show improvement in their endotheliafunction also failed to improve their cardiac function class and status, demonstrating a direct relationship between endothelial dysfunction and cardiovascular disease, supporting the role of EECP as an effective therapeutic strategy for patients with endothelial dysfunction. 1.0 0.5 01st h17th h35th h1-month follow-up *N=18Pre-Post-*p<0.05; †p<0.05 vs pre EECP index on 1st, 17th and 35th hr J Am Col Cardiol 2003:41101761-8*PAT Index 2.0Despite significant cardiac risk profiles and advanced CAD among patients included Results of the Mayo Clinic were supported by another paper in 2003 by Shechter and co-workers using the endothelial-dependent, flow-mediated dilation (FMD) of the brachial artery with high-resolution 22 ultrasound technique to assess endothelial vasomotor function. This is a prospective age-matched controlled study. The endothelial function in 20 consecutive CAD patients (15 males), mean age 68 ± 11 years, with refractory angina pectoris CCS class III and IV, unsuitable for coronary revascularization was assessed by FMD before and after their ECP treatment. These measurements were compared with 20 matched control CAD patients (17 males). There were no significant group differences in baseline characteristics between the ECP and Control group, with 75% in CCS class IV. There were no significant changes in concomitant medication use and no serious adverse effects throughout the study. After completion of 35 hours of daily 1 hour ECP treatment, FMD improved significantly from baseline 3.1 ± 2.2% to 8.2 ± 2.1%; p=0.01), whereas there were no changes in the Control group within the 2-month period. ECP also improved angina symptoms by a reduction in mean number of sublingual nitrate tablets consumption per day (from 4.2 ± 2.7 to 0.4 ± 0.5; p<0.001), compared with no change in the Control group (4.5 ±2.3 to 4.4 ± 2.6; p=0.87). The mean CCS class also improved significantly in the ECP group (3.5 ± 0.5 to 1.9 ± 0.3; p<0.0001), with no change in the Control group (3.3 ± 0.6 to 3.5 ± 0.5; p=0.89). This study demonstrates that ECP intervention compared with controls results in significant improvement in endothelial dysfunction and cardiac function status. In 2004, Bonetti and co-workers reported a very interesting case of a 29 year-old woman with chest pain 23 despite medications with various calcium antagonists, β-blocker and antidepressant. Coronary angiography revealed structurally normal vessels. Administration of adenosine into the left coronary system showed an intact endothelium-independent microvasculature response; with a normal coronary flow reserve of 2.5. However, intracoronary infusion of grades doses of endothelium-dependent -6 -4 vasodilator acetylcholine (10 to 10 mol/L) into the left anterior descending (LAD) artery was associated with a progressive decrease in coronary flow, ultimately resulted in complete LAD occlusion, compatible with the presence of severe endothelial dysfunction of both the coronary microvasculature and the coronary macrovasculature. Despite the addition of an angiotensin-converting enzyme (ACE) inhibitor and L-arginine supplementation to the patient’s existing treatment regimen, the patient symptoms worsened during the subsequent months and severely impaired her functional capacity. Patient status changed from CCS Class III to CCS class IV. Patient was treated with 35-hour of daily 1-hour course of EECP. After completion of EECP, the patient was free of angina and was able to perform her daily activities without the dyspnea or fatigability experienced before EECP. At the last follow-up visit 3 months after completion of EECP therapy, the patient was symptom free with a medication regimen of calcium channel blockade, ACE inhibitor and L-arginine supplementation. Endothelial dysfunction is considered to be major key early event in atherosclerosis. This case is interesting because the patient had no traditional cardiovascular risk factors and no manifestations of advanced atherosclerotic disease and Baseline 2-month after EnrollmentJ Am Coll Cardiol 2003;42:2090-5 yet suffered from severe coronary endothelial dysfunction. The sustained clinical improvement after a standard course of EECP in a patient with severely symptomatic coronary endothelial dysfunction supports the concept that EECP can be used as a treatment of endothelial dysfunction. 6. Effects of EECP treatment on arterial stiffness, a manifestation of endothelial dysfunction Arterial stiffness is a strong independent predictor of cardiovascular outcomes above and beyond traditional cardiovascular risk factors in both healthy subjects and patients with high risk of coronary artery 24,25 disease. Muscular arterial stiffness is related to smooth muscle tone and NO bioavailability. Under basal conditions, NO is continually released from healthy endothelial cells and serves to inhibit adhesion of platelets and leukocytes to the vessel wall. After diffusion to the media, NO activates the enzyme guanyl cyclase, which increases formation of cyclic guanosine monophosphate (cGMP) to relax smooth muscle cells and maintain vascular patency and distensibility. When the endothelium becomes dysfunctional, bioavailability of NO is limited, impairing smooth muscle cell relaxation, leading to arterial stiffness. The effect of EECP treatment on artery stiffness has been examined by Nichols and co-workers using applanation tonometry to measure radial artery pressure waveforms for the generation of the central 26 aortic pressure waveforms using a mathematical transfer function. The constructed aortic pressure waveform can be considered to have two components, the forward flow from cardiac ejection (from Pd to Pi) and reflected wave from peripheral (Ps-Pi). As arterial stiffness incretransmission velocity of both forward and reflected waves increase, causing the reflected wave to arrive earlier in late systole, increasing systolic blood pressure, left ventricular (LV) workload and therefore tension time index. The augmentation of aortic pressure can be expressed as augmented pressure [AP=(Ps-Pi)] or Augmentation Index and the myocardial energy wasted in overcoming this additional systolic pressure can be cal Nichols and colleagues measured the radial artery pressure waveforms of 20 patients with stable refractory angina before and after 34 1-hour EECP sessions. The heart rate and ejection duration did not change with EECP treatment. Brachial systolic and pulse pressure reduced significantly from 132 ± 18 to 121 ± 18 mm Hg (p<0.001) and 61 ± 15 to 54 ± 16 mm Hg (p<0.001) respectively. Aortic systolic pressure reduced from 120 ± 18 to 108 ± 18 mm Hg (p<0.001), and aortic pulse pressure from 48 ± 14 to 41 ± 16 mm Hg Pressure Waveforms Pressure without reflectionPsPiPdPulse Pressure = (Ps – Pd) Augmentation Index = AIx =(Ps – Pi) / (Ps – Pd) Time for pressure wave to travel from aortic root and back = Δt p Wasted LV pressure energy = 2.09 X Δtp * (Ps – Pi) LVWorkload=TensionTimeIndex=areaundersystolicwave (p<0.001). Mean blood pressure also decreased significantly from 92 ± 13 to 84 ± 9.5 mm Hg (p<0.001). Associated with the fall in arterial blood pressure was an improvement in wave reflection characteristics. Compared with baseline, reflected wave augmented pressure AP decreased from 13 ± 7.1 to 8.7 ± 6.8 mm Hg (p<0.001) after EECP treatment, and Alx referenced at a heart rate of 75 beats/min reduced from 18 ± 9.6 % to 12 ± 8.4 % (p<0.01), indicating a significant reduction of arterial stiffness. The reduced arterial stiffness caused a decrease in transmission velocity and increase travel time Δtp/2 of the reflected wave from the lower body to the heart (p<0.001), and a decrease in reflected wave systolic duration Δtr from 182 ± 33 to 168 ± 41 ms (p<0.01). The improvement in arterial wall properties and wave reflection characteristics indicated a significant reduction in LV workload. These afterload changes were associated with improvement in indexes of myocardial oxygen demand. The reduction in wave reflection pressure with EECP treatment and the associated decrease in wave reflection duration caused a decline in LV wasted energy. Also, compared with baseline, the tension-time index (representing myocardial oxygen demand) also reduced significantly (p<0.001). EECP treatment reduces arterial stiffness was also supported by the findings of Levenson and co-workers in a prospective, randomized, controlled study using high-resolution ultrasound Echo-Doppler evaluation of the diameters of the carotid artery in 30 patients (28 males and 2 females) with stable coronary artery 27 disease. The patients were randomly assigned to either an active EECP group (n=15) with 300 mm Hg applied pressure or a sham group (n=15) with less then 75 mm Hg of applied external counterpulsation pressure during EECP treatment. All subjects underwent 35 hours of either sham or active st th th counterpulsation. Echo-Doppler studies were performed after the 1 hour, the 17 hour and the 35 hour of EECP therapy. A longitudinal scan of both right and left common carotid arteries allowed visualization of the lumen-intima and media-adventitia interfaces of the proximal and distal wall, the maximum diameter (dmax) and minimum diameter (dmin) were then determined for each cardiac cycle, average over 3-4 successive cycles. Average brachial blood pressures were measured during carotid examination and the mathematically transformed to central systolic pressure (Ps) and central diastolic pressure (Pd). Measurement of arterial stiffness can be estimated by the nondimensional pressure-independent β stiffness index: β stiffness index = Ln(Ps/Pd)/DD where DD = (Dmax-Dmin)/Dmin is the arterial distension. Carotid artery blood flow was measured and carotid vascular resistance (CVR) can be calculated as CVR=Mean blood pressure /volume blood flow (ml/min). Platelet cGMP content was measured at baseline and after 17 and 35 hour of EECP therapy. There were no significant between-group differences in baseline clinical characteristics or in baseline carotid hemodynamics values. There were no major complications occurred during EECP treatment. The absolute change from baseline before EECP in the β stiffness index was significantly reduced at 1 hour (p<0.01), 17 hour (p<0.001) and 35 hour (p<0.01) after EECP treatment in the active EECP group, and this decrease was statistically different when compared with controls at 1 and 35 hour (p<0.05, respectively). Also, in contrast to controls, mean carotid blood flow in patients receiving active EECP increased significantly at 1 hour (p<0.05) and again more strongly at 35 hour (p<0.001), with a trend present at 17 hour (p=0.07). The difference between groups was significant at 17 hour (p<0.05) and 35 hour (p<0.01). Carotid vascular resistance was concomitantly reduced in active EECP treated group at 17 hour (p<0.05) and 35 hour (p<0.01), showing a significant difference between groups in carotid vascular resistance at 17 hour (p<0.01) and 35 hour (p<0.001). Adjustment for multiple covariates (age, sex, systolic and diastolic blood pressure, body mass index, smoke, glucose and low-density lipoprotein cholesterol) did not change the observed differences in arterial stiffness or vascular resistance between the study groups. Platelet cGMP contents increased at 1, 17 and 35 hour by 0.019 ± 0.02, 0.058 ± 0.05 8 and 0.052 ± 0.05 pmol/10 platelets in controls and by 0.097 ± 0.02, 0.059 ± 0.08 and 0.087 ± 0.09 pmol/108 platelets in the active EECP treated groups respectively. Platelet cGMP in the active group negatively correlated with β stiffness index (n=59, r=-0.32, p<0.05), but not in patients in the control group. Results of this study suggest that active EECP therapy relaxes the smooth muscle tone of the carotid artery and consequently decreases their arterial stiffness via the signaling product of NO pathways, supporting the hypothesis that EECP therapy improves endothelial dysfunction. th Recently, Braith and co-workers reported in the 2009 American College of Cardiology 58 Annual Scientific Session the results of a prospective, randomized, controlled study on the effects of EECP in the 28 peripheral endothelial functions of 30 symptomatic patients with CAD (20 active and 10 sham). Control (Sham) EECP Active EECP Variables Baseline BFMD (%) 4.2 ± 0.7 Post Sham 4.3 ± 0.6 p Baseline NS 3.7 ± 0.2 PostEECP 5.8 ± 0.4 p <0.05 FFMD (%) 2.8 ± 0.4 2.8 ± 0.3 NS 2.6 ± 0.2 3.5 ± 0.3 <0.05 FBF (ml/min/100ml) 19.0 ± 1.6 18.9 ±1.5 NS 19.3 ± 1.3 23.5 ± 1.4 <0.05 CBF (ml/min/100ml) 17.1 ± 1.6 16.9 ± 1.5 NS 15.2 ± 1.4 18.8 ± 1.0 <0.05 23 ± 2 22 ± 4 NS 24.2 ± 3 16.8 ± 4 <0.05 135 ± 4 131 ± 4 NS 134 ± 3 144 ± 2 <0.05 49 ± 8 48 ± 7 NS 54 ± 9 33 ± 6 <0.05 CF-PWV (m/sec) 11.5 ± 0.7 11.6 ± 0.5 NS 12.1 ± 0.5 10.2 ± 0.4 <0.05 Plasma Nox (μmol/L) 24.8 ± 5.2 25.3 ± 6.4 NS 21.5 ± 2.5 32.8 ± 3.4 <0.05 ADMA (μmol/L) 0.75±0.07 0.74±0.09 NS 0.66 ± 0.04 0.44 ±0.03 <0.05 ED (sec) 550 ± 71 566 ± 68 NS 582 ± 40 771 ± 56 <0.05 Time to angina (sec) 366 ± 43 374 ± 31 NS 392 ± 45 602 ± 44 <0.05 VO 16.0 ± 1.5 17.0 ± 1.3 NS 17.2 ± 1.0 21.2 ± 1.3 <0.05 Ala (%) ΔT (ms) p LV -2 we (msec-mm Hg ) 2peak (ml/kg/min)