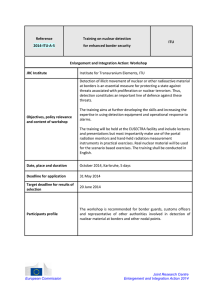
Supplemental Table 1. Processing using BP
advertisement

Supplemental Table 1. Processing using BP-SPECT, TOMPOOL and QBS BP-SPECT BP-SPECT is count-based, automatic and thus reproducible. Filtered images are backprojected to form transaxial slices, reoriented manually in order to include the entirety of both ventricles in the field of views. There is no operator interference in the determination of the size and the shape of regions used for ventricles segmentation. According to the literature, mid-ventricular locations are automatically determined by searching for maximum activity in volumetric regions likely to correspond to the RV in the short-axis [SA], horizontal long-axis [HLA] and vertical long-axis [VLA]. RVEDV VLA is defined by the contiguous voxels that contain counts ≥ 35% of the maximum end-diastolic counts found over the entire RV volume (RVEDV VLA) while avoiding the right and pulmonary artery based on Fourier phase images. Then, RVESV VLA is generated based on the ED region and phase images. Finally, RVEDV SA is generated by voxels that have > 35% of maximum RVEDV counts in SA images while avoiding LV and pulmonary artery areas. The pulmonary valve plane is placed as high as necessary to include all structures with counts that increase synchronously with LV. Biventricular EFs are computed from systolic count changes within voxels inside identified RVEDV and RVESV that have > 35% of maximum counts.(18). TOMPOOL Data are transferred to TOMPOOL as Dicom files (Horizontal Long Axis). We used the default options: down-sampling on 8 times frames, threshold at 30% of the maximal activity, approximation of the ejection curves using a reference curve (9) with 15 iterations, 80% maximal compression, and 50% minimal slope. The operator-dependent steps of the procedure are the localization of the valvular, septal, and infundibular planes by detecting change in shape and activity. According to the previous studies (10-13), the semi-automatic segmentation procedure is based on a watershed algorithm. Voxels whose value is less than 30% of the maximal activity in the acquisition are set to zero. The scintigraphic images are segmented using a fully 4D immersion approach taking adjacent slices and time frames into consideration. The 4D voxel groups generated by the watershed algorithm are then aggregated, depending on the relative position of their barycentre with respect to the septal and valvular planes, to build up three 4D regions (left ventricular, right ventricular, and extraventricular). Voxels belonging to the right ventricle and located above the infundibular plane are excluded. Further manual correction of the produced ventricular regions was not performed. QBS The main difference between this algorithm and the one used in previous versions of the software is the increased robustness introduced by the coupling of the LV and RV surfaces. The most automatic procedure was utilized in order to obtain an optimal reproducibility. Filtered images were backprojected to form transaxial slices, which were reoriented manually in order to include the entirety of both ventricles in the field of views. QBS is now a count-threshold based method but used to be a gradient-based method and the procedure was mostly defined for the analysis of the left ventricle (1, 7, 14, 15). According to the literature, the gradient based procedure is described above. The first step is to automatically approximate a static endocardial surface with a deformable ellipsoid (relative counts and counts density gradients are used). Then, a dynamic endocardial surface is computed for each gating-time interval (sampling) using temporal Fourier analysis of volumetric count density information. The plane of the pulmonary valve is then positioned and RV is separated from pulmonary artery: it has been observed that it rarely extends more than 2 pixels above the anterior wall or below the inferior wall of the identified LV limits. EF calculations were initially geometric (based on the number of voxels in EDV and ESV), but they are count-based in the newest version. The new count-based segmentation algorithm operates in consecutive steps: initial filtering and VCC calculation to separate ventricles, atria and extra-cardiac structures; ventricular surface fit (one surface surrounding both LV and RV); septal surface fit (one surface describing the interventricular septum); surface resampling into separate LV and RV surfaces; optional RV pulmonary conus truncation; ROI computation based on selected threshold; count-based calculations (using counts and number of voxels). Each surface fit uses a weighting scheme that takes into account counts, first and second derivatives along rays defined in a local coordinate system. Supplemental Table 2. CMR: parameters of acquisition and processing. CMR imaging was performed according to CMR guidelines and using the optimal pulse sequences. Images were acquired on two 1.5-T scanners (Magnetom Avanto 1.5T, Siemens; Ingenia 1.5T, Philips) with multiplane localizers. The parameters of acquisition parameters and the processing are described in Supplemental Table 2. The best cut-off values in order to diagnose a dilatation of the RV or an impairment of the right function were calculated according to the normal values obtained in previous MRI studies (EDV>88mL/m², EF≤45%, CO<4L/min)(16), (17). The cut-off value for EDV enlargement was defined as superior to 167mL. We used two protocols of cine cardiac MR imaging: Single-breath-hold-true-Fast Imaging with Steady-state Precession [FISP] (Siemens, FOV: 380mm, slice thickness: 8mm with 0mm interslice gaps,TR: 24.96ms, TE: 1.56ms, Flip Angle:80°) and Balanced Turbo FieldEcho (TFE) (Philips, FOV: 320mm, slice thickness: 8mm with 0mm interslice gaps, TR: 3ms, TE: 1.51ms, TFE factor 16, Flip Angle:60°). During breath-holding, prospective ECG-gated cine CMR was performed with 35 frames per cardiac cycle. The parameters were assessed, on 10 to 12 short axis contiguous slices from tricuspid valves to apex. Two experimented radiologist examined images off-line using ARGUS software (v4.02, Siemens). Those two physicians were blinded from the results from the physicians performing the T-ERNV calculations and were therefore different physicians. Contours of the endocardial border were drawn manually on short axis on all phases. The operator defined visually the basal slice, the apical slice, ES and ED. CMR values were derived by the modified Simpson’s rule from regions that were defined to conform to endocardial borders. Ventricular volumes were determined as the sum of the slice cavity volumes. In the basal slice of the short axis, both in ED and ES, only the portion of the right ventricle outflow tract below the level of the pulmonary valve was included. For the inflow part of the RV, the blood volume was excluded from the RV volume if the surrounding wall was thin and not trabeculated since it was considered to be in the right atrium. The apical slice was the last slice containing blood in the cavity. Papillary muscles and trabeculations were included in the endocardial contouring to improve reproducibility Supplemental Figure 1. Automatic delineation of the endocardial contour by BPSPECT. Images acquired in short-axis [SA], horizontal long-axis [HLA] and vertical longaxis[VLA] are compared in four patients.A delineation of the RV (yellow) and of the left ventricle (white) according to BP-SPECT is showed in three patients (B, C and D) and compared to MRI (A). This figure illustrates the absence of anatomical information on TERNV, the complex shape of the right ventricle and thus the interest of automatic software. Supplemental Figure 2. Semi-automatic definition of the valve planes by TOMPOOL. Horizontal-long-axis tomographic slices are showed in five patients. This figure illustrates the fact that the manual delineation of the right ventricle would be time consuming and that the delineation of the endocardial contour is easier when the right ventricle is larger. TOMPOOL being a semi-automatic software, the operator defines manually the valve planes and should theoretically be more reliable and appropriate in order to assess RV function. However the manual delineation of the valve plane leads to a decrease reproducibility. References: (1) (2) (3) (4) (5) (6) (7) (8) (9) (10) (11) (12) (13) (14) De Bondt P, Claessens T, Rys B, De Winter O, Vandenberghe S, Segers P et al. Accuracy of 4 different algorithms for the analysis of tomographic radionuclide ventriculography using a physical, dynamic 4-chamber cardiac phantom. Journal of nuclear medicine : official publication, Society of Nuclear Medicine 2005;46:165-71. Nichols K, Saouaf R, Ababneh AA, Barst RJ, Rosenbaum MS, Groch MW et al. Validation of SPECT equilibrium radionuclide angiographic right ventricular parameters by cardiac magnetic resonance imaging. Journal of nuclear cardiology : official publication of the American Society of Nuclear Cardiology 2002;9:153-60. Van Kriekinge SD, Berman DS, Germano G. Automatic quantification of left ventricular ejection fraction from gated blood pool SPECT. Journal of nuclear cardiology : official publication of the American Society of Nuclear Cardiology 1999;6:498-506. Nichols KJ, Van Tosh A, Wang Y, Palestro CJ, Reichek N. Validation of gated blood-pool SPECT regional left ventricular function measurements. Journal of nuclear medicine : official publication, Society of Nuclear Medicine 2009;50:53-60. Nichols KJ, Van Tosh A, De Bondt P, Bergmann SR, Palestro CJ, Reichek N. Normal limits of gated blood pool SPECT count-based regional cardiac function parameters. The international journal of cardiovascular imaging 2008;24:717-25. Nichols K AA, Rheem J, et al. . Accuracy of gated blood pool SPECT ventricular function parameters: validation by MRI [abstract]. Journal of the American College of Cardiology 2001;37. Nichols K, Humayun N, De Bondt P, Vandenberghe S, Akinboboye OO, Bergmann SR. Model dependence of gated blood pool SPECT ventricular function measurements. Journal of nuclear cardiology : official publication of the American Society of Nuclear Cardiology 2004;11:282-92. Akinboboye O, Nichols K, Wang Y, Dim UR, Reichek N. Accuracy of radionuclide ventriculography assessed by magnetic resonance imaging in patients with abnormal left ventricles. Journal of nuclear cardiology : official publication of the American Society of Nuclear Cardiology 2005;12:418-27. Caderas de Kerleau C, Crouzet JF, Ahronovitz E, Rossi M, Mariano-Goulart D. Automatic generation of noise-free time-activity curve with gated blood-pool emission tomography using deformation of a reference curve. IEEE transactions on medical imaging 2004;23:48591. Mariano-Goulart D, Collet H, Kotzki PO, Zanca M, Rossi M. Semi-automatic segmentation of gated blood pool emission tomographic images by watersheds:application to the determination of right and left ejection fractions. European journal of nuclear medicine 1998;25:1300-7. Mariano-Goulart D, Dechaux L, Rouzet F, Barbotte E, Caderas de Kerleau C, Rossi M et al. Diagnosis of diffuse and localized arrhythmogenic right ventricular dysplasia by gated bloodpool SPECT. Journal of nuclear medicine : official publication, Society of Nuclear Medicine 2007;48:1416-23. Mariano-Goulart D, Piot C, Boudousq V, Raczka F, Comte F, Eberle MC et al. Routine measurements of left and right ventricular output by gated blood pool emission tomography in comparison with thermodilution measurements: a preliminary study. European journal of nuclear medicine 2001;28:506-13. Sibille L, Bouallegue FB, Bourdon A, Micheau A, Vernhet-Kovacsik H, Mariano-Goulart D. Comparative values of gated blood-pool SPECT and CMR for ejection fraction and volume estimation. Nuclear medicine communications 2011;32:121-8. Daou D, Harel F, Helal BO, Fourme T, Colin P, Lebtahi R et al. Electrocardiographically gated blood-pool SPECT and left ventricular function: comparative value of 3 methods for ejection fraction and volume estimation. Journal of nuclear medicine : official publication, Society of Nuclear Medicine 2001;42:1043-9. (15) Van Kriekinge S BD, Germano G. Automatic quantification of left and right ventricular ejection fractions from gated blood pool SPECT [abstract]. Circulation 1999;100. (16) Haddad F, Hunt SA, Rosenthal DN, Murphy DJ. Right ventricular function in cardiovascular disease, part I: Anatomy, physiology, aging, and functional assessment of the right ventricle. Circulation 2008;117:1436-48. (17) Lorenz CH, Walker ES, Morgan VL, Klein SS, Graham TP, Jr. Normal human right and left ventricular mass, systolic function, and gender differences by cine magnetic resonance imaging. Journal of cardiovascular magnetic resonance : official journal of the Society for Cardiovascular Magnetic Resonance 1999;1:7-21.

![The Politics of Protest [week 3]](http://s2.studylib.net/store/data/005229111_1-9491ac8e8d24cc184a2c9020ba192c97-300x300.png)