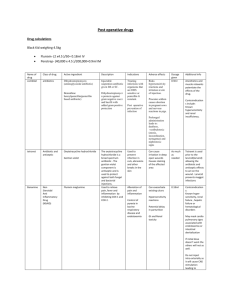
Antibiotic Stewardship Process Maps

Antibiotic Stewardship Process Maps
Stage 1 – Environmental Scan and Initial Planning
1
Identify problem
(IPC and Pharmacy data)
2
Understand the hospital:
Patient type
Hospital size
Areas of speciality
Number of ICUs
Talk to
Doctors
Current/ retrospective review: antibiotic utilisation and organism resistance/ prevalence profiles
5
Resources
Ensure there are suitable resources available (eg Pharmacists)
Train the resources
March, 2011
3
Know the Doctors:
Key Opinion Leaders?
Doctor specialities?
Which units do the Doctors admit to?
Who is willing to participate in a programme?
4
Identify major role players
Communicate and obtain support where possible from:
All Doctors
Microbiologist/s
Pharmacist/s
IPC Practitioner
Nursing staff
Antibiotic Stewardship Process Maps
Stage 2 - Creating Awareness and Preparing the Ground
March, 2011
1
Identify problem and obtain permission to propose solutions via Antibiotic
Stewardship
2
Have a formalised communication session/ presentation/ launch programme/ CPD event to as many Doctors as possible:
Specialist meeting
Medical/ Physician Advisory Committees
Infection Control meetings
Special event
4
Provide education on appropriate antibiotic use
Microbiologist/s to assist
All Doctors
Pharmacist/s
IPC Practitioner
Nursing staff
Hospital Management
3
Memo to Doctors and Nursing staff:
Overview
Intervention types, which unit, how often
Antibiotic Stewardship Process Maps
Stage 3 - Establishing a Team
1
Identify the team members
Key Doctors
Microbiologist/s
Pharmacist/s
IPC Practitioner
Unit Managers
2
Establish the committee:
Initial meeting
Establish primary interventions
Agree to certain intervention tools
Discuss progress reports
3
Review IPC data:
Alert organism profile
Organism resistance/ surveillance profile
March, 2011
4
Initial ward
Decide on the appropriate area to initiate the programme
Suggested intervention tools:
1.
Daily antibiotic report per patient
2.
Daily checklist – ward round
3.
Reconciliation reports – Antibiotic/s to pathogen/s
4.
Hazardous Biologic Agent report – in units & trend analysis
5.
Treatment guidelines available in the hospital
6.
Record pharmacist interventions
7.
Means to communicate to Doctors: a.
One-on-one discussion b.
Phone call c.
Text/ sms message d.
Note on chart e.
Other note format
Antibiotic Stewardship Process Maps March, 2011
Stage 4 - Establishing Extent of the Problem; Stage 5 - Set goals & Prioritise Interventions
1 – Pathology
Appropriate specimens are taken?
Prompt lab results?
Microbiology results for all patients on antibiotics?
Treatment tailored to pathogen?
2 – Local sensitivity data available for pathogens:
IPC – organism report
Lab data (Ampath, Lancet,
NHLS etc)
3 – Microbiologist available to consult:
If not – contact labs to find someone to work with. Contact number available in all relevant areas.
Determine the problem
(7 points to consider)
Agree process to follow with the committee
If not followed, further direct discussion (peer to peer, microbiologist, pharmacist, committee)
4 – Empiric/ treatment guidelines available in all areas:
Ampath general guidelines
Committee to tailor guidelines based on local organism prevalence and resistance patterns
6 – Pharmacist resource:
Identify interested pharmacist/s
Employ pharmacists with clinical interest
5 – Surgical prophylaxis guidelines:
Available in theatre?
Correct antibiotics per procedure?
No high level agents used?
Prophylaxis given 1 hr before incision?
Antibiotics stopped when patient out of theatre or within 24 hours (as appropriate)?
Antibiotic Stewardship Process Maps
Stage 6 - Measurement
March, 2011
1 – Organism report
Monthly
2 – Antibiotic/ Pathology cumulative report from the Labs
Weekly
9 – Antibiotics used for surgical prophylaxis
Weekly
Measurement tools (9 to consider)
8 – Antibiotic utilisation report
Duration of therapy
More than 3 agents at a time
Duplicate cover
Monthly
7 – Interventions suggested vs accepted comparison
Monthly
3 – Antibiotic report per patient
Daily
5 – Pharmacist notes
Daily
6 – Pharmacist suggested intervention report
Monthly
4 – Pharmacist checklist/
Patient summary chart
Daily
Antibiotic Stewardship Process Maps
Stage 7 - Review of Effectiveness; Stage 8 - Spread
1 – Daily, weekly, monthly reports
Relevant individuals to prepare and monitor their reports for trends
March, 2011
2 – Discuss at the committee meeting
3 – Communicate as agreed by the committee
Positive outcomes , such as:
8.
Positive change in pathogen resistance patterns
9.
Decreased ICU stays
10.
Decreased ventilator days
11.
Increased acceptance of interventions
12.
Positive change to antibiotic prescribing habits
13.
Decreased costs (overall)
Publish data and communicate successes to all stakeholders
Spread the intervention/s to more units within the hospital
No progress changes or challenges faced:
1.
Consider the obstacles, obtain feedback and find solutions
2.
Committee to agree to intervention changes
3.
Consult with key opinion leaders
4.
Have education sessions if necessary
5.
Communicate intervention alterations to all stakeholders
Monitor progress and review outcomes at next committee meeting