SUPPLEMENTAL MATERIAL - Springer Static Content Server
advertisement
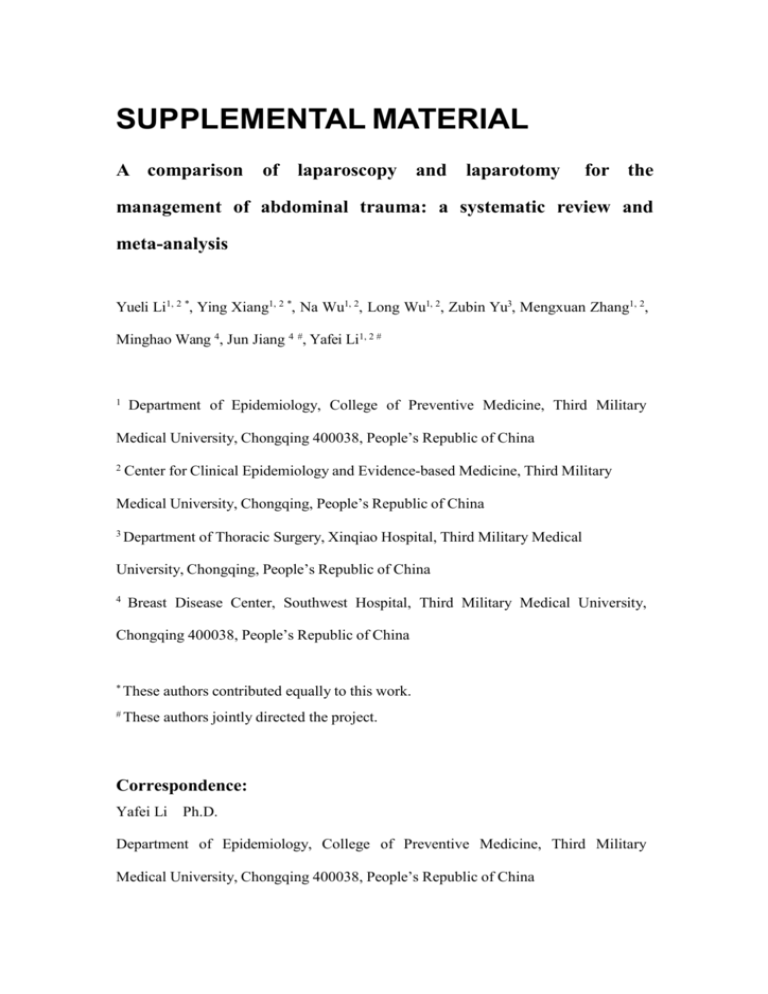
SUPPLEMENTAL MATERIAL A comparison of laparoscopy and laparotomy for the management of abdominal trauma: a systematic review and meta-analysis Yueli Li1, 2 *, Ying Xiang1, 2 *, Na Wu1, 2, Long Wu1, 2, Zubin Yu3, Mengxuan Zhang1, 2, Minghao Wang 4, Jun Jiang 4 #, Yafei Li1, 2 # 1 Department of Epidemiology, College of Preventive Medicine, Third Military Medical University, Chongqing 400038, People’s Republic of China 2 Center for Clinical Epidemiology and Evidence-based Medicine, Third Military Medical University, Chongqing, People’s Republic of China 3 Department of Thoracic Surgery, Xinqiao Hospital, Third Military Medical University, Chongqing, People’s Republic of China 4 Breast Disease Center, Southwest Hospital, Third Military Medical University, Chongqing 400038, People’s Republic of China * These authors contributed equally to this work. # These authors jointly directed the project. Correspondence: Yafei Li Ph.D. Department of Epidemiology, College of Preventive Medicine, Third Military Medical University, Chongqing 400038, People’s Republic of China E-mail: liyafei2008@hotmail.com Telephone: +86 23 68752293 Supplementary Table 1. Newcastle-Ottawa Quality assessment score scale Supplementary Table 2. Characteristics of case report studies included for meta-analysis Supplementary Table 3. Newcastle-Ottawa Scale score of included cohort studies Supplementary Table 4. Cochrane Collaboration’s risk of bias assessment results of included RCTs Supplementary Table 5. The publication bias of RCT and cohort studies by Begg’s tests Supplementary Table 6. The publication bias of case series reports by Begg’s tests Supplementary Figure 1. Flow diagram of literature search and study selection Supplementary Figure 2. The pooled incidence of postoperative complications in treating patients with abdominal trauma Supplementary Figure 3. The pooled perioperative mortality rate in treating patients with abdominal trauma Supplementary Figure 4. The pooled cure rate in treating patients with abdominal trauma Supplementary Figure 5. Comparison of time to postoperative exhaust of laparoscopy with open laparotomy in treating patients with abdominal trauma Supplementary Figure 6. Comparison of duration of pain of laparoscopy with open laparotomy in treating patients with abdominal trauma Supplementary Figure 7. Comparison of time to out of bed of laparoscopy with open laparotomy in treating patients with abdominal trauma Supplementary Figure 8. Comparison of time to regular diet of laparoscopy with open laparotomy in treating patients with abdominal trauma Supplementary Figure 9. The pooled incidence of missed injuries in treating patients with abdominal trauma Supplementary Figure 10. The pooled incidence of conversions in treating patients with abdominal trauma Supplementary Table 1. Newcastle-Ottawa Quality assessment score scale Item Score NOS score scale for cohort studies† Selection (1) Representativeness of the exposed cohort Truly representative of the average status in the community 1 Somewhat representative of the average status in the community 1 Selected group of users eg nurses, volunteers 0 No description of the derivation of the cohort 0 (2) Selection of the non exposed cohort Drawn from the same community as the exposed cohort 1 Drawn from a different source 0 No description of the derivation of the non exposed cohort 0 (3) Ascertainment of exposure Secure record (eg surgical records) 1 Structured interview 1 Written self report 0 No description 0 (4) Demonstration that outcome of interest was not present at start of study Yes 1 No 0 Comparability (1) Comparability of cohorts on the basis of the design or analysis Study controls for the most important factor 1 Study controls for any additional factor 1 Outcome (1) Assessment of outcome Independent blind assessment 1 Record linkage 1 Self report 0 No description 0 (2) Was follow-up long enough for outcomes to occur? Yes 1 No 0 (3) Adequacy of follow up of cohorts Complete follow up - all subjects accounted for 1 Subjects lost to follow up unlikely to introduce bias 1 Item Score Follow up rate is low and no description of those lost 0 No statement 0 A study can be awarded a maximum of one score for each numbered item within the Selection and Outcome categories. A maximum of two scores can be given for Comparability. Supplementary Table 2. Characteristics of case report studies included for meta-analysis First author Year Country Subtype of abdominal trauma Study design Treatment method VAL Control Number of participants VAL Zhao GQ [30] 2013 China Traumatic splenic rupture Case report Laparoscopic surgery 68 Yang YL [31] 2013 China Case report 2013 China Laparoscopic surgery Laparoscopic surgery 80 Ni KY [32] Blunt abdominal trauma Blunt abdominal trauma Yin YH [33] 2012 China Blunt abdominal trauma Case report Laparoscopic surgery 56 Lan MY [34] 2011 China Blunt abdominal trauma Case report Laparoscopic surgery 52 Guo SW [35] 2010 China Blunt abdominal trauma Case report Laparoscopic surgery 59 Chen QW [36] 2010 China Case report 2008 China Laparoscopic surgery Laparoscopic surgery 98 Yin J [37] Blunt abdominal trauma Blunt abdominal trauma Case report Case report 56 57 The main results reported* Control Missed injuries 0,conversions 6,complications 2,mortality 0,cure rate 91.2%(62/68) Missed injuries 0,conversions 15,complications 0 Missed injuries 0,conversions 16,complications 0,mortality 0,cure rate 71.4%(40/56) Missed injuries 0,conversions 10,complications 0,mortality 0,cure rate 82.1%(46/56) Missed injuries 0,conversions 24,complications 0,mortality 0,cure rate 53.8%(28/52) Missed injuries 0,conversions 15,mortality 0,cure rate 74.6%(44/59) Conversions 22,mortality 0,cure rate 77.6%(76/98) Missed injuries 0,conversions 19,complications 1,mortality Li CY [38] 2007 China Blunt abdominal trauma Abdominal trauma Case report Laparoscopic surgery Laparoscopic surgery 58 Zhou ZG [39] 2013 China Gao YD [40] 2006 China Abdominal trauma Case report Laparoscopic surgery 68 Chen WY [41] 2013 China Abdominal trauma Case report Laparoscopic surgery 60 Ke LX [42] 2012 China Abdominal trauma Case report Laparoscopic surgery 100 Kou BY [43] 2011 China Abdominal trauma Case report Laparoscopic surgery 74 Hu XP [44] 2012 China Case report 2011 China Laparoscopic surgery Laparoscopic surgery 54 Zhao YT [45] Abdominal trauma Abdominal trauma Yang ZQ [46] 2011 China Abdominal trauma Case report Laparoscopic surgery 326 Case report Case report 55 72 1,cure rate 66.7%(38/57) Missed injuries 1,conversions 8,complications 0,mortality 0 Missed injuries 3,conversions 10,complications 2,cure rate 81.8%(45/55) Missed injuries 6,conversions 31,complications 5,mortality 0,cure rate 54.4%(37/68) Missed injuries 0,conversions 11,mortality 0,cure rate 81.7%(49/60) Missed injuries 0,conversions 51,complications 3,mortality 0,cure rate 46%(46/100) Missed injuries 0,conversions 25,complications 1,mortality 0,cure rate 66.2%(49/74) Missed injuries 0,conversions 21,complications 8,mortality 0 Missed injuries 0,conversions 11,complications 1,mortality 0,cure rate 84.7%(61/72) Missed injuries 0,conversions 42,mortality 0,cure rate 87.1%(284/326) Wei JB [47] 2011 China Abdominal trauma Case report Laparoscopic surgery 102 Shi JQ [48] 2011 China Abdominal trauma Case report Laparoscopic surgery 87 Gao ZJ [49] 2011 China Abdominal trauma Case report Laparoscopic surgery 60 Xu GC [50] 2011 China Abdominal trauma Case report Laparoscopic surgery 62 Zhao CS [51] 1998 China Case report 1998 China Laparoscopic surgery Laparoscopic surgery 68 Shao RQ [52] Abdominal trauma Abdominal trauma Chou HM [53] 2010 China Abdominal trauma Case report Laparoscopic surgery 62 Mei GS [54] 2009 China Abdominal trauma Case report Laparoscopic surgery 80 Nu HQ [55] 2009 China Abdominal trauma Case report Laparoscopic surgery 52 Case report 60 Missed injuries 0,conversions 18,complications 3,mortality 0,cure rate 82.4%(84/102) Missed injuries 0,conversions 20,complications 3,mortality 0,cure rate 77%(67/87) Missed injuries 12,conversions 5,mortality 0,cure rate 91.7%(55/60) Missed injuries 0,conversions 16,complications 3,mortality 0,cure rate 74.2%(46/62) Conversions 4 Missed injuries 1,conversions 8,complications 1,mortality 1,cure rate 85%(51/60) Missed injuries 0,conversions 13,complications 0,mortality 0,cure rate 79%(49/62) Missed injuries 0,conversions 4,complications 0,mortality 0,cure rate 95%(76/80) Missed injuries 0,conversions 16,complications 1,mortality 0,cure rate 69.2%(36/52) Tian SL [56] 2009 China Abdominal trauma Case report Laparoscopic surgery 60 Ran QH [57] 2009 China Abdominal trauma Case report Laparoscopic surgery 76 Shi XZ [58] 2009 China Case report 2009 China Zhang XH [60] 2008 China Laparoscopic surgery Laparoscopic surgery Laparoscopic surgery 61 Chen XX [59] Abdominal trauma Abdominal trauma Abdominal trauma Sun ZG [61] 2006 China Abdominal trauma Case report Laparoscopic surgery 85 Ma D [62] 2005 China Abdominal trauma Case report Laparoscopic surgery 58 Huang H [63] 2003 China Abdominal trauma Case report Laparoscopic surgery 50 Zhou C [64] 2011 China Case report 2011 China Laparoscopic surgery Laparoscopic surgery 72 Qin C [65] Abdominal stab wounds Abdominal trauma with Case report Case report Case report 58 52 60 Missed injuries 0,conversions 22,complications 0,mortality 0,cure rate 63.3%(38/60) Missed injuries 0,conversions 11,complications 0,mortality 0,cure rate 85.5%(65/76) Missed injuries 0,conversions 13,complications 4,mortality 0 Missed injuries 0,conversions 10,complications 2,mortality 0 Missed injuries 0,conversions 13,complications 9,mortality 0,cure rate 75%(39/52) Missed injuries 0,conversions 22,complications 4,mortality 0,cure rate 74.1%(63/85) Missed injuries 0,conversions 15,complications 0,mortality 0,cure rate 74.1%(43/58) Missed injuries 5,conversions 27,complications 8,mortality 0,cure rate 46%(23/50) Missed injuries 0,conversions 14,complications 5,mortality 0 Missed injuries 0,complications 2 Ahmed N [66] 2005 USA Saribeyoqlu K [67] 2007 Turkey Ivatury RR [68] 1993 New York Sitnikov V [69] 2009 Russia Chol YB [70] 2003 Korea Zantut LF [71] 1997 Brazil Sosa JL [72] 1995 USA *VAL,video-assisted laparoscopy; " gastrointestinal injuries Penetrating abdominal wounds Abdominal stab injuries Case report Laparoscopic surgery 52 Missed injuries 0,conversions 12,complications 3,mortality 0 Case report Diagnostic and therapeutic laparoscopy Laparoscopic surgery 88 Missed injuries 1,conversions 18,mortality 0 100 Conversions 54,complications 10,mortality 3 Penetrating abdominal wounds Small bowel injuries in abdominal trauma Abdominal trauma Penetrating abdominal wounds Case report Abdominal gunshot wounds Case report ", not applicable. Case report VAL 819 Complications 97,mortality 19 Case report Therapeutic laparoscopy Diagnostic and therapeutic laparoscopy Laparoscopic surgery 78 Missed injuries 0,conversions 0,complications 3,mortality 0 Conversions 207,complications 10,mortality 4 Case report 510 121 Missed injuries 0,conversions 39,mortality 0 Supplementary Table 3. Newcastle-Ottawa Scale score of included cohort studies Selection First author Ouyang M Tian LF Yang T Li YC Liang TC Cai W Hou QZ Zheng JJ Liao CH Khubutiya MSh Streck CJ Feliz A Lin HF Cherkasov M Cherry RA Lee PC Comparability Outcome Total score Representati -veness of the exposed cohort Selection of the non exposed cohort Ascertainment of exposure Demonstration that outcome of interest was not present at start of study Comparability of cohorts on the basis of the design or analysis Assessment of outcome Was follow-up long enough for outcomes to occur Adequacy of follow up of cohorts 0 0 0 0 0 0 0 0 0 0 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 2 2 2 2 2 2 1 1 2 2 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 8 8 8 8 8 8 7 7 8 8 0 0 0 0 1 1 1 1 1 1 1 1 1 1 1 1 2 1 2 2 1 1 1 1 1 1 1 1 1 1 1 1 8 7 8 8 0 0 1 1 1 1 1 1 2 2 1 1 1 1 1 1 8 8 Supplementary Table 4. Cochrane Collaboration’s risk of bias assessment results of included RCTs First Random Allocation Blinding of author sequence concealment generation Blinding of Incomplete Selective Other participants outcome outcome reporting bias and assessment data personnel Li XY Zuo CH Low risk Unclear Low risk Low risk Low risk Low risk Low risk Unclear Unclear Low risk Low risk Low risk Low risk Low risk Leppaniemi A Karateke F Kawahara NT Unclear Unclear Low risk Low risk Low risk Low risk Low risk High risk Unclear Low risk Low risk Low risk Low risk Low risk High risk Unclear Low risk Low risk Low risk Low risk Low risk Supplementary Table 5.The publication bias of RCT and cohort studies by Begg’s tests Outcome Coef t value P value 95% CI Postoperative complications -0.439 -1.95 0.075 [-0.93,0.05] Perioperative mortality rate -0.246 -0.69 0.560 [-1.78,1.29] Length of hospital stay -1.748 -0.69 0.501 [-7.11,3.62] Operation time 0.561 0.10 0.925 [-12.59,13.72] Amount of intraoperative blood loss -11.442 -4.55 0.045 [-22.27,-0.62] Time to postoperative exhaust -16.179 -0.97 0.385 [-62.27,29.91] Duration of postoperative pain 4.492 74.10 0.009 [3.72,5.26] Length of ICU stay -24.520 -8.94 0.071 [-59.36,10.32] Time to out of bed 1.399 34.29 0.001 [1.22,1.58] Time to regular diet -55.881 -5.22 0.035 [-101.95,-9.81] Coef, coefficient; CI, confidence interval Supplementary Table 6.The publication bias of case series reports by Begg’s tests Outcome Coef t value P value 95% CI Postoperative complications 1.698 2.22 0.036 [0.12,3.28] Missed injuries 3.372 5.98 0.002 [1.92,4.82] Conversions 3.542 2.65 0.012 [0.84,6.25] Perioperative mortality rate 0.746 1.02 0.382 [-1.58,3.07] Cure rate -5.819 -5.80 0.000 [-7.88,-3.76] Coef, coefficient; CI, confidence interval Articles identified (n=1753) Articles excluded after reading titles and abstracts, which do not contain abdominal trauma or laparoscopy (n=1534) through database searching Articles excluded that are duplicate (n=7) Articles included before reading the full text(n=212) 148 articles were not relevant or the subjects were insufficient 64 articles included in the systematic review and meta-analysis Supplementary Figure 1. Flow diagram of literature search and study selection Supplementary Figure 2. The pooled incidence of postoperative complications in treating patients with abdominal trauma. Forest plots of proportion and overall proportion with 95% CI in case series reports. Black square indicates the proportion, with the size of the square inversely proportional to its variance, and horizontal lines represent 95% CI. The pooled results are indicated by the gray diamond. CI, confidence interval. Supplementary Figure 3. The pooled perioperative mortality rate in treating patients with abdominal trauma. Forest plots of proportion and overall proportion with 95% CI in case series reports. Black square indicates the proportion, with the size of the square inversely proportional to its variance, and horizontal lines represent 95% CI. The pooled results are indicated by the gray diamond. CI, confidence interval. Supplementary Figure 4. The pooled cure rate in treating patients with abdominal trauma. Forest plots of proportion and overall proportion with 95% CI in case series reports. Black square indicates the proportion, with the size of the square inversely proportional to its variance, and horizontal lines represent 95% CI. The pooled results are indicated by the gray diamond. CI, confidence interval. Supplementary Figure 5. Comparison of time to postoperative exhaust of laparoscopy with open laparotomy in treating patients with abdominal trauma. Forest plots of MD and overall MD with 95% CI between group of laparoscopy and group of open laparotomy. Green square indicates the MD, with the size of the square inversely proportional to its variance, and horizontal lines represent 95% CI. The pooled results are indicated by the black diamond. MD, mean difference; CI, confidence interval. Supplementary Figure 6. Comparison of duration of pain of laparoscopy with open laparotomy in treating patients with abdominal trauma. Forest plots of MD and overall MD with 95% CI between group of laparoscopy and group of open laparotomy. Green square indicates the MD, with the size of the square inversely proportional to its variance, and horizontal lines represent 95% CI. The pooled results are indicated by the black diamond. MD, mean difference; CI, confidence interval. Supplementary Figure 7. Comparison of time to out of bed of laparoscopy with open laparotomy in treating patients with abdominal trauma. Forest plots of MD and overall MD with 95% CI between group of laparoscopy and group of open laparotomy. Green square indicates the MD, with the size of the square inversely proportional to its variance, and horizontal lines represent 95% CI. The pooled results are indicated by the black diamond. MD, mean difference; CI, confidence interval. Supplementary Figure 8. Comparison of time to regular diet of laparoscopy with open laparotomy in treating patients with abdominal trauma. Forest plots of MD and overall MD with 95% CI between group of laparoscopy and group of open laparotomy. Green square indicates the MD, with the size of the square inversely proportional to its variance, and horizontal lines represent 95% CI. The pooled results are indicated by the black diamond. MD, mean difference; CI, confidence interval. Supplementary Figure 9. The pooled incidence of missed injuries in treating patients with abdominal trauma. Forest plots of proportion and overall proportion with 95% CI in case series reports. Black square indicates the proportion, with the size of the square inversely proportional to its variance, and horizontal lines represent 95% CI. The pooled results are indicated by the gray diamond. CI, confidence interval. Supplementary Figure 10. The pooled incidence of conversions in treating patients with abdominal trauma. Forest plots of proportion and overall proportion with 95% CI in case series reports. Black square indicates the proportion, with the size of the square inversely proportional to its variance, and horizontal lines represent 95% CI. The pooled results are indicated by the gray diamond. CI, confidence interval.