Emergency Preparedness in Obstetrics
advertisement
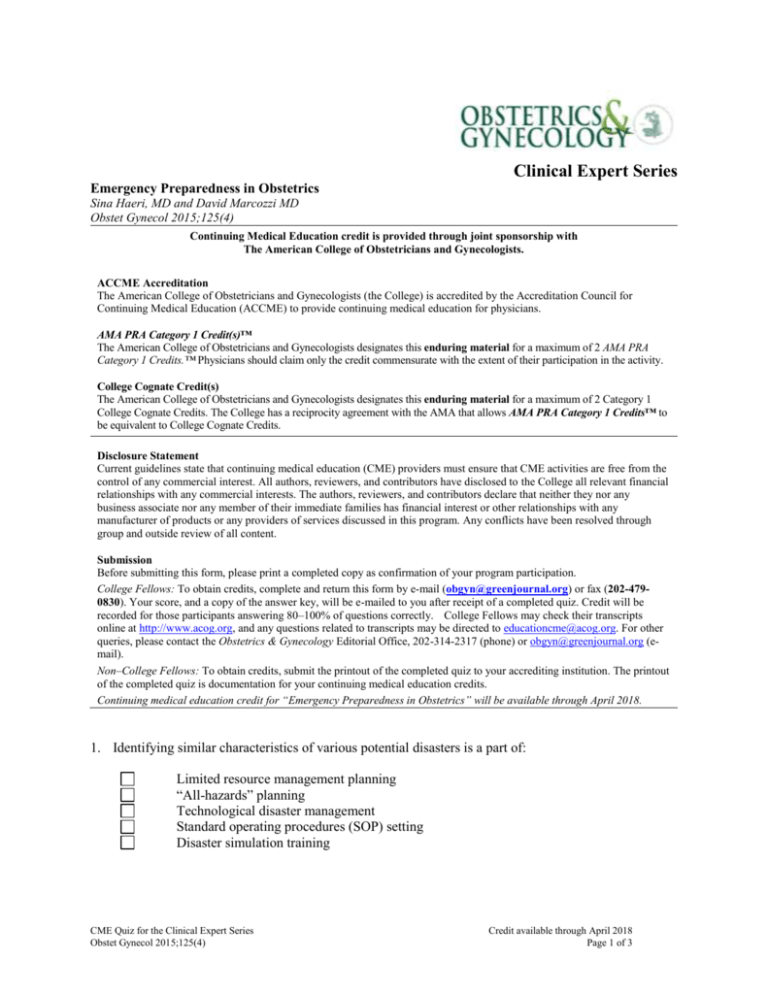
Clinical Expert Series Emergency Preparedness in Obstetrics Sina Haeri, MD and David Marcozzi MD Obstet Gynecol 2015;125(4) Continuing Medical Education credit is provided through joint sponsorship with The American College of Obstetricians and Gynecologists. ACCME Accreditation The American College of Obstetricians and Gynecologists (the College) is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians. AMA PRA Category 1 Credit(s)™ The American College of Obstetricians and Gynecologists designates this enduring material for a maximum of 2 AMA PRA Category 1 Credits.™ Physicians should claim only the credit commensurate with the extent of their participation in the activity. College Cognate Credit(s) The American College of Obstetricians and Gynecologists designates this enduring material for a maximum of 2 Category 1 College Cognate Credits. The College has a reciprocity agreement with the AMA that allows AMA PRA Category 1 Credits™ to be equivalent to College Cognate Credits. Disclosure Statement Current guidelines state that continuing medical education (CME) providers must ensure that CME activities are free from the control of any commercial interest. All authors, reviewers, and contributors have disclosed to the College all relevant financial relationships with any commercial interests. The authors, reviewers, and contributors declare that neither they nor any business associate nor any member of their immediate families has financial interest or other relationships with any manufacturer of products or any providers of services discussed in this program. Any conflicts have been resolved through group and outside review of all content. Submission Before submitting this form, please print a completed copy as confirmation of your program participation. College Fellows: To obtain credits, complete and return this form by e-mail (obgyn@greenjournal.org) or fax (202-4790830). Your score, and a copy of the answer key, will be e-mailed to you after receipt of a completed quiz. Credit will be recorded for those participants answering 80–100% of questions correctly. College Fellows may check their transcripts online at http://www.acog.org, and any questions related to transcripts may be directed to educationcme@acog.org. For other queries, please contact the Obstetrics & Gynecology Editorial Office, 202-314-2317 (phone) or obgyn@greenjournal.org (email). Non–College Fellows: To obtain credits, submit the printout of the completed quiz to your accrediting institution. The printout of the completed quiz is documentation for your continuing medical education credits. Continuing medical education credit for “Emergency Preparedness in Obstetrics” will be available through April 2018. 1. Identifying similar characteristics of various potential disasters is a part of: Limited resource management planning “All-hazards” planning Technological disaster management Standard operating procedures (SOP) setting Disaster simulation training CME Quiz for the Clinical Expert Series Obstet Gynecol 2015;125(4) Credit available through April 2018 Page 1 of 3 2. An effective method to increase community disaster preparedness for pregnant women is through: Public service announcements Childbirth classes Hospital-sponsored Internet sites Community opinion surveys Emergency medical services (EMS) provider training 3. When planning for sheltering in place for the pregnant woman and her family, the amount of water that should be set aside is: 0.5 gallon per person per day 1.0 gallon per person per day 1.5 gallons per person per day 1.0 gallon per person per day plus 1.5 gallons per pregnant person 700 mL per kg of combined weight of those sheltering, including infants 4. In preparing for a possible office closure during a disaster, it is most important that disaster planning include: Provision for physical security of the practice Off-site record storage and access Planning for utility cutoff (eg, gas service) Answering machine messages Policies on overtime pay 5. Under emergency conditions the “standard of care”: Remains unchanged Is specified by accreditation bodies Must be determined by the chief of staff Is determined by the nature of the emergency Is limited to essential care 6. Which of the following areas can be pressed into service to meet the specific needs of high-risk neonates during an emergency? Conference rooms Post-anesthesia care units Secured waiting areas Operating rooms Semi-private postpartum rooms CME Quiz for the Clinical Expert Series Obstet Gynecol 2015;125(4) Credit available through April 2018 Page 2 of 3 7. Obstetric disaster triage is best accomplished by: Patient’s family members Advanced practice nurses Obstetric physicians Maternal-fetal medicine specialists Emergency room physicians 8. A pregnant patient beyond 24 weeks of gestation has to undergo an emergency laparotomy for treatment following major trauma. Delivery should be: Dictated by normal obstetric considerations By hysterotomy at the time of laparotomy Delayed pending steroid administration By transcervical evacuation at the time of surgery --- 9. A core body temperature less than 95°F in a pregnant patient may result in: Increased cardiac output Increased plasma volume Bradycardia Disseminated intravascular coagulation Hypervigilance 10. When a pregnant women is exposed to an explosion in an enclosed space, the patient or fetus should be monitored for: Uterine rupture Placental abruption Neonatal deafness Fetal skeletal damage Fetal pulmonary damage College ID Number: Name: Address: City/State/Zip: E-mail Address: Actual time spent completing this activity (you may record up to 2 hours): CME Quiz for the Clinical Expert Series Obstet Gynecol 2015;125(4) Credit available through April 2018 Page 3 of 3