PTE Pediatric Asthma Metrics - Maine Health Management Coalition
advertisement

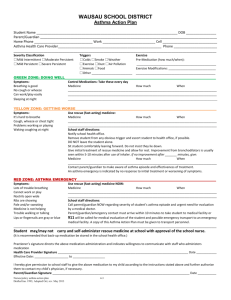
PTE Pediatric Asthma Metrics Reporting The Maine Health Management Coalition’s (MHMC) Pathways to Excellence (PTE) initiative is updating its pediatric asthma metrics. Current ratings on the MHMC website (www.getbettermaine.org) using the previous metrics, will expire on July 1, 2013. Practices have now through May 17, 2013, to submit their new data using the process as outlined below. Practices submitting data on these measures by May 17, 2013 can have their new ratings updated for July 1, 2013. Practice Name: _____________________________ Date: _____________________________ Practice Address: ______________________________ Date: Person Completing: _________________________ Phone: _____________________________ Responsible Clinician:________________________ Signature: ___________________________ ________________________________ PTE Pediatric Asthma Metrics and Scoring, Updated September 2012 Asthma Measures NUMERATOR DENOMINATOR (Note: for practices doing manual chart review, must be > 10 charts for ages 2<5 and > 20 charts for ages 5<19 Practice Rate 1. Asthma Assessment Max Points for Measure Practice Points Achieved(Practice Rate multiplied by Maximum Points Available)* 15 2. Lung Function Testing (Note: Ages 5<19) 3. Medication Therapy 15 15 4. Influenza Vaccination 15 5. Patient Self Management Plan 15 6 Documented Tobacco Exposure/Use 7. BMI % 15 10 Sub-Total Points Available/Received 8. Population Based Reporting-EMR/Registry for all asthmatics? Yes/No 100 Yes = 10 No = 0 Total points for Population-Based reporting (if applicable) * The points for each category are rounded to the next whole number. ** Best is only achievable for those reporting their total population regardless of the final score. MHMC Rating (Good, Better, Best) Good > 45 Points Better > 65 Points ** Best > 75 Points PTE Asthma Specifications and Targets 1 The PTE Physician Steering Committee recognizes that lung function testing has not been utilized as much as NHLBI guidelines recommend. Therefore, accommodations in scoring were made to allow practices to obtain the best rating in 2013 while working to bring their lung function testing rates up to guidelines. (See Sample Scoring Below) PTE Pediatric Asthma Metrics – Example Asthma Measures from Chart Submission NUMERATOR DENOMINATOR (Note: for practices doing manual chart review, must be > 10 charts for ages 2<5 and > 20 charts for ages 5<19 Practice Rate Max Points for Measure Practice Points Achieved(Practice Rate multiplied by Maximum Points Available)* 40 50 80% 15 12 10 20 50% 15 8 45 50 90% 15 14 38 50 76% 15 11 38 50 76% 15 11 38 50 76% 15 11 45 50 90% 10 9 100 76 Yes = 10 No = 0 0 1. Asthma Assessment 2. Lung Function Testing (Note: Ages 5<19) 3. Medication Therapy 4. Influenza Vaccination 5. Patient Self-Management Plan 6 Documented Tobacco Exposure/Use 7. BMI % Sub-Total Points Available/Received 8. Population Based Reporting-EMR/Registry for all asthmatics? Yes/No Total points for Population-Based reporting (if applicable) 76 * The points for each category are rounded to the next whole number. ** Best is only achievable for those reporting their total population regardless of the final score. MHMC Rating (Good, Better, Best) Good > 45 Points Better > 65 Points ** Best > 75 Points SUBMISSION INSTRUCTIONS: 1. Complete form and have responsible clinician sign. 2. Send to Maine Health Management Coalition either by fax or scan and email: 207-899-3207 Email to pte@mehmc.org a. FAX: b. 3. Responsible clinician signs attestation form (agrees to the validation of results and reporting methodology). PTE Asthma Specifications and Targets 2 4. Practice agrees to participate in an on-site validation of the data, upon MHMC’s request. 5. If possible, practice reports from registry or EMR. If none of these choices are available, then a chart review can be done. Note: There must be a minimum of 10 patient charts reviewed for ages 2<5 and 20 patient charts reviewed for ages 5< 19 (a total of at least 30 charts). 6. Recognition will be effective for 2 years from the date of submission and the practice agrees to be publically reported on the www.getbettermaine.com reporting website. 7. Practices who do not meet the lowest level of scoring criteria (<45 points) will be notified and reported as “Did not Report” on the aforementioned reporting website. These practices can resubmit data 6 months from the date of the initial submission. 8. If desired, practices who currently have the PTE good or better rating may resubmit for a higher rating prior to their expiration date. INCLUSION CRITERIA An eligible asthma patient is one who meets all three of the following criteria: 1. Is between the ages of 2 and <19 years of age on the last day of the reporting period. 2. Has been under the care of the participating practice for at least 24 months. This is defined as at least two face-to-face office visits with a physician, physician's assistant, or nurse practitioner with one visit in each measurement year. (Encounter CPT codes: 99201-99205, 99212-99215, 99241-99245, 99383-99386, and 99393-99396) 3. Patient has a documented diagnosis of asthma (ICD-9 Dx Codes: 493.00-493.02, 493.10-493.12, 493.20493.22, 493.80-493.82, and 493.90-493.92) (Above Criteria is from the American Medical Association Measure Steward guidance on ASTHMA: Algorithm for Measure Calculation-EHRS [Analytic Narrative and Data Elements]) 4. Include all patients regardless of payer (e.g. commercial, Medicare, Medicaid, self-pay, uninsured, etc.). 5. Practices can include patients that are primarily managed by subspecialists for asthma in their data set. 6. Providers should clinically verify that all the patients meet the National Heart, Lung, and Blood Institute (NHLBI) definition for asthma (as defined in "Definitions" in specifications document). 7. Practices are encouraged to submit population based data on all patients that meet criteria in their practice. Only practices that submit population data from EHR, registry or claims can attain a "best" rating. Practices that are doing chart review will be expected to submit data on at least 30 patients. (10 for ages 2 <5 and 20 for ages 5< 19.) If this minimum is not met for your practice, please include an explanation with your submission materials. PTE Asthma Specifications and Targets 3 # Maine Health Management Coalition Pathways to Excellence: Asthma Measure Specifications Revised September 2012 Measure Name PTE Measure Description and Criteria Numerator (N) Denominator (D) Asthma Assessmenti: % of patients with diagnosis of asthma ages 2 and <19, who were evaluated during at least one office visit within 12 mo for daytime and nocturnal asthma symptoms. Lung Function Testingii: % of patients with diagnosis of asthma ages 5 and <19 yo in which one or more spirometry result(s) have been obtained within the past 24 months Numerator: Total number of children 2<19 yo with a diagnosis of asthma who were evaluated within 12 mo for the frequency (numeric) of daytime and nocturnal asthma symptoms. Denominator: Patients between the ages of 2 and <19 years who have been under the care of the participating practice for at least 24 months and have a documented diagnosis of asthma. For asthma control tests, these tools are validated: Test for Respiratory and Asthma Control in Kids TRACK 2 < 4 years of age, and Asthma Control Test ACT ≥ 4 years of age Numerator: Number of patients 5 <19 yo who have had spirometry completed at least once in the last 24 mo. Denominator: Patients between the ages of 5 and <19 years who have been under the care of the participating practice for at least 24 months and have a documented diagnosis of asthma. Will need to document that some children are physically unable to perform test 3 Medication Therapyiii: % of patients ages 2 and <19 yo who were identified as having persistent asthma and were appropriately prescribed controller medication Numerator: Total number of patients age 2<19 identified with persistent asthma who were appropriately prescribed controller medication within the last 12 mo. Denominator: Patients between the ages of 2 and <19 years who have been under the care of the participating practice for at least 24 months and have a documented diagnosis of persistent asthma. 4 Influenza Vaccinationiv: % of patients with diagnosis of asthma ages 2 and <19 yo Numerator: Total number of patients ages 2<19 yo with flu shot documented within the last 12 mo Denominator: Patients between the ages of 2 and <19 years who have been under the 1 2 PTE Asthma Specifications and Targets Moderate or Severe Persistent Asthmatics may need to have lung function testing done more frequently than every 2 years; this metric will capture that all asthmatics should have lung function testing at least every 2 years . Need to document contraindications (included in BTE metric) ACIP: Recommends influenza vaccination for 4 who have a documented flu shot within the past 12 mo care of the participating practice for at least 24 months and have a documented diagnosis of asthma. all >6 months and when supply is limited focus on those with chronic pulmonary disease (including asthma), among others. 5 Patient SelfManagement Planv: % of patients with diagnosis of asthma ages 2 and <19 yo, that have a current written action plan on file updated within the last year Numerator: Number of patients 2<19 yo with a written action plan updated within the last 12 mo. Denominator: Patients between the ages of 2 and <19 years who have been under the care of the participating practice for at least 24 months and have a documented diagnosis of asthma. An asthma action plan (also called a management plan) is a written plan that is developed by a provider with a family that outlines a patient’s medical therapy and asthma symptoms that warrant further treatment or action 6 Tobacco Exposure and Use: % of patients with diagnosis of asthma ages 2 and <19 yo with annual documentation of tobacco exposure/ tobacco use Numerator: Total number of children ages 2 and <19 yo with documentation of tobacco exposure and for children ages 10 and <19 assessed for tobacco use within the last 12 mo. Denominator: Patients between the ages of 2 and <19 years who have been under the care of the participating practice for at least 24 months and have a documented diagnosis of asthma. Tobacco exposure is defined as someone who uses tobacco who lives in the household or is a primary caregiver. 7 BMI %vi: % patients % of patients with diagnosis of asthma ages 2 and <19 yo with BMI% documented Numerator: Patients 2<19yo who have evidence of Body Mass Index (BMI) percentile documentation within the last 12 mo. Denominator: Patients between the ages of 2 and <19 years who have been under the care of the participating practice for at least 24 months and have a documented diagnosis of asthma i Adapt Meaningful use, NQF #001, AMA (Currently ages 5-40) ii Adapt BTE Lung Function and Spirometry Metric (Currently ages 5-75 and yearly evaluation) NHLBI 2007 Guidelines: The Expert Panel recommends the following frequencies for spirometry measurements: PTE Asthma Specifications and Targets 5 (1) at the time of initial assessment (Evidence C); (2) after treatment is initiated and symptoms and PEF have stabilized, to document attainment of (near) “normal” airway function; (3) during a period of progressive or prolonged loss of asthma control; and (4) at least every 1–2 years to assess the maintenance of airway function (Evidence B, extrapolation from clinical trials). Spirometry may be indicated more often than every 1–2 years, depending on the clinical severity and response to management (Evidence D). These spirometry measures should be followed over the patient’s lifetime to detect potential for decline and rate of decline of pulmonary function over time (Evidence C). iii Adapt Meaningful use /NQF #0036 (Currently ages 5-11, 12-50) iv Adapt BTE Influenza Vaccination Metric (Currently ages 5 -75 years) v Adapt BTE Patient Self-Management Plan Metric (Currently ages 5-75 years) vi Adapt BTE Body Mass Index Metric (Currently Percentage of patients ages 18-75) DEFINITIONS Asthma: To establish a diagnosis of asthma, the clinician should: - Use a medical history and exam to determine that symptoms of variable and recurrent episodes of airflow obstruction, airway hyper responsiveness, and underlying inflammation are present. In susceptible individuals, this inflammation causes recurrent episodes of coughing (particularly at night or early in the morning), wheezing, breathlessness, and chest tightness. (Source: p. 9 of Abridged NHLBI Guidelines) - Use spirometry in all patients 5 years or greater to determine the level of airflow obstruction and assess reversibility - Exclude alternative diagnoses (Upper Airway Disease- allergic rhinitis and sinusitis; Obstruction of the large airways: foreign body in trachea or bronchus, vocal cord dysfunction, vascular ring or laryngeal web, laryngotracheomalacia, tracheal stenosis, or broncheostenosis, enlarged lymph node or tumor; Obstructions involving small airways: viral bronchiolitis or obliterative bronchiolitis, cystic fibrosis, bronchopulmonary dysplasia, heart disease; Other causes: recurrent cough not due to asthma, aspiration from swallowing mechanism dysfunction or gastroesophageal reflux) (Source: Differential Diagnosis for Asthma, AH! Program Flipchart, p. 3) Persistent Asthma: - Symptoms >2 days per week OR - Awaken at night from asthma 1-2X per month for children ages 2 <5 years and >2X per month ages 5 <19 years OR - Limitation of activities, despite pretreatment for exercise induced asthma OR - More than 2 steroid bursts in 1 year OR - FEV1 <80% predicted OR low FEV1/FVC ratio PTE Asthma Specifications and Targets 6