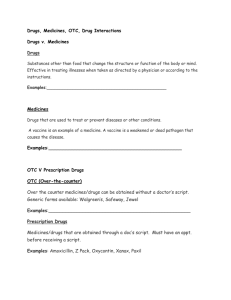
Practicum Summary Report - Institute for Healthcare Improvement
advertisement

PRACTICUM SUMMARY REPORT Name: Ellie Salter Team Members: Ellie Salter, Eilidh Gunn, Jennifer Gray Project Title: Improving Medicines Reconciliation on Acute Surgical Receiving Unit University/Organization Name: The University of Dundee, Scotland Health System Sponsor Name: NHS Tayside Aim of project That more than 50% of all medicines reconciliation documents will be fully completed and 100% accurate on admission to ASRU (Acute Surgical Receiving Unit), Ninewells Hospital, Dundee, Scotland by April 2013. This aim is built upon the foundations of an ongoing quality improvement project surrounding medicines reconciliation initiated in August 2012; this project has a working target of 95% of all medicines reconciliations performed being 100% accurate. Planned changes tested (2-3 sentences) Completion and accuracy data (11 data items) was collected for 13 patients on the Acute Surgical Receiving Unit, following two changes to the medicines reconciliation form (v1). Data analysis occurred following which further changes to the form were made (v2). This was tested on a sample of 37 patients, collecting 10 data items. To gauge patient experience of medicines reconciliations a questionnaire was distributed to 19 patients who had been admitted to ASRU. Predictions (2-3 sentences) It is predicted that the form will result in more accurate completion of medicines reconciliation with >50% fully completed and 100% accuracy. This will improve the quality of med rec completion in a unit where reliance on the pharmacy team to complete medicines reconciliation has developed. Individual ability to complete the documentation may cause variation. Results Present your results with a graph(s). Graph Displaying Number of Medicines Reconciliations: 100% Complete 100% Accurate Run Chart The graph below clearly describes that there was a very poor level of full completion and 100% accuracy of medicines reconciliation in the forms collected on the unit. Only 2 forms from the 50 collected were both fully completed and 100% accurate. Both of these medicines reconciliations were collected in the early cycles of the project. This level of completeness and accuracy fell far below the target established at the onset of this quality improvement project. The plausible reasons for this are described further in the remainder of this practicum report. Graph Displaying Number of Medicines Reconciliations: 100% Complete 100% Accurate Run Chart 100 % Medicines Reconciliation %100 Complete and 100% Accurate 90 80 %: 100% Complete 100% Accurate 70 60 Target: 50% 50 40 Early Cycles: n= 2/13 Later Cycles: n= 0/37 Total n=50 30 20 10 0 Early Cycles Later Cycles Stage of Project Graph Displaying Number of Medicines Reconciliations: 100% Complete 100% Accurate Run Chart The graph below displays the findings of the patient questionnaire that was distributed to 19 patients to explore their experience of medicines reconciliation on the unit. It shows that 100% of patients were asked for an allergy check and that they are a reliable source of information regarding their medications. 100% of patients believed that they were taking all necessary and required medications. Graph Displaying Patient Experience of Medicines Reconciliation 100 80 Yes 60 40 No YesN/A 20 No 0 N/A Summary of results (3-4 sentences): The early cycles showed that there was better completion and accuracy than the later cycles. In later cycles with the implementation of v2 forms no complete and accurately filled mec rec forms were retrieved. An improvement in the accuracy and completion was not observed during the four week project. Learning (4-5 sentences) Comparison of questions, predictions, and analysis of data: From the results, it can be seen that there was better completion and accuracy than during the early cycles compared to the later cycles. Following the early cycles (using form v1), the data collection technique and time management was improved by the team members with data being collected on 37 patients. Individual variation can impact a great deal on results; in this project there was a junior doctor who failed to perform any medicines reconciliation due to lack of education surrounding its importance. Communicating with the unit staff and explaining the improvement project that was occurring over the 4 week period was vital in ensuring that the project ran smoothly and that data collection was successful. Changing the prerequisite minimum number of sources required to complete medicines reconciliation from 2 to 3, resulted in decreased compliance in completion of forms. Basing the outcome measure on both full completeness and 100% accuracy proved too ambitious. This resulted in the outcome measure not being met. When performing any future quality improvement projects a greater level on consideration will be taken when determining outcome measures. Patients are a reliable source of information when performing medicines reconciliation. Impact on systems (3-4 sentences) Discuss the project’s significance on the local system and any findings that may be generalizable to other systems: It is clear that there is an unreliable system for medical staff completing medicines reconciliation in the unit which results in poor completion and accuracy. Changing the requirement from 2 to 3 sources consulted during medicines reconciliation was too much without implementing staff education and was therefore poorly performed by medical staff (see PDSA cycle 2 document). Foundation doctors may be difficult to engage. They are often on the unit for only a short amount of time, don’t have clinical support for the improvement and may not have essential undergraduate training and understanding of their responsibility as part of medicines reconciliation. Changing med rec forms will have an impact on all who use them, so ensuring that they are aware of the changes implemented and rationale behind them is vital in ensuring improvement prior to expanding such changes to other units. Conclusions (3-5 sentences) Summarize the outcome of the project. Is this project sustainable? What are the requirements for sustainability? Disappointingly, no improvement was seen during the project. The project is sustainable, however if continued, the measures should be modified. Potential outcome measures include an improvement of 50% from the baseline level of 100% accuracy with the level of completeness becoming a process measure. Using patients as a source of information is a sustainable part of the system. Overall the project has highlighted the requirement for adequate staff training and education to enable them to perform adequate med rec when working in such a unit. Such education would be required for sustainability, reminding medical staff of their roles and responsibility regarding med rec. Some of the education surrounding medicines reconciliation could form part of the undergraduate medicine curriculum. Reflections/Discussions (5-7 sentences) Discuss the factors that promoted the success of the project and that were barriers to success. What did you learn from doing this project? What are your reflections on the role of the team? Despite being the responsibility of the medical team there has become a reliance on the pharmacy team to complete med rec. The whole culture of the unit combined with the perceived lack of time proved to barrier to success. With regards to leadership there is no consultant (attending) driving the improvement work resulting in a lack of motivation within the medical team to engage with the pharmacy staff in this area of quality improvement. Through undertaking this quality improvement project, the team members have gained an insight into the organisation and the considerations and skills required to implement future projects. In particular, ensuring that measures are easy to define and outcome measures are achievable. Education of staff and team members is essential for further improvement. By signing this document (electronic signature is acceptable), I attest that the information provided by the learners in this project is accurate. LEARNER(S): Signature: Signature: Printed Name: Eilidh Gunn Printed Name: Ellie Salter Area of Study: ARSU, Ninewells, Dundee Area of Study: ASRU, Ninewells, Dundee FACULTY SPONSOR: HEALTH SYSTEM SPONSOR (if different from faculty sponsor): Signature: Signature: Printed Name: Vicki Tully Printed Name: Jennifer Gray Institution: Institution: University of Dundee NHS Tayside AUTHORIZATION Do the learners, faculty sponsor, and health system sponsor authorize this project for publication at www.ihi.org? ☒ Yes ☐ No