Figure 7 demonstrates that PAX9 expression falls in all grades of
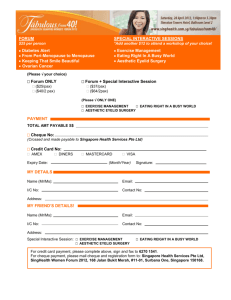
advertisement

Evaluation of PAX9 as a Novel Biomarker in Oral Carcinogenesis Renna Mahsoub Supervisors: Dr Max Robinson, Dr Ralf Kist Centre for Oral Health Research, School of Dental Sciences Masters by Research 2011-2012 Introduction Oral cancer is a lethal disease and a global health care problem. Within the UK, over 6000 new cases were detected in 2009 and the current statistics suggest that there has been minimal improvement in the survival rates over the past 50 years (Cancer Research, 2009). Oral cancer encompasses several different histological types, but the most common is squamous cell carcinoma (OSCC), which accounts for 90% of all oral cancers (Kujan et al., 2006a). The oral cavity can be divided into sub-sites; the most commonly affected by OSCC are the lateral border of the tongue (Figure 1) and the floor of the mouth (Werning, 2007). Other sub-sites; including the buccal mucosa, hard palate, and gingivae, are less commonly affected. Figure 1. OSCC on lateral tongue. Image courtesy of Max Robinson. The majority of OSCC patients are aged 65 years or older however, there has been a recent increase in incidence in middle aged men for unknown reasons (Cancer Research, 2009). The disease is twice as common in males compared to females (Petersen, 2009). There are several environmental risk factors for oral cancer but it is thought that tobacco and alcohol abuse are the most common in the UK (Cancer Research, 2009) Survival rates from oral cancer are poor with only 50% survival at 5 years (Baykul et al., 2010). This figure had not improved despite great advances in medical knowledge and technology. The reason for this is still unknown but many speculate it is down to factors such as late presentation of patients with advanced disease, high loco-regional recurrence rates, distant metastasis and the development of second primary tumours (SPTs) within the upper-aerodigestive tract. (Baykul et al., 2010; OCIU, 2010). Loco-regional recurrence i.e. near the original site of the cancer occurs in around 10-30% of patients and SPTs occur in 3-4% of patients (Braakhuis et al., 2005). It was proposed that this is due to a concept known as field cancerisation. This theory was devised by Slaughter et al in 1953 in an article investigating changes in head and neck epithelium in oral cancer patients. It begins with normal epithelium developing one or more genetic mutations and changing into a patch of abnormal tissue. This accumulates more mutations and becomes a field of atypical epithelium which subsequently progresses into carcinoma (Tabor et al., 2001). As the model progresses, the surface area affected by mutations is increasing resulting in a greater risk of local recurrence or SPTs within the upper aero-digestive tract. Potentially Malignant Disorders Many OSCCs are preceded by a potentially malignant disorder (PMD) (Reibel, 2003) which may be noticed by the patient or detected by a professional. These lesions vary clinically in terms of size, shape and colour (Mehrotra and Gupta, 2011). These lesions are usually pain-free and can go unnoticed by the patient thus making late presentation of disease a common feature in oral cancer patients (van der Waal, 2009). The progression of a PMD to cancer is unpredictable, it may remain as a non-invasive patch, it may regress or it may progress to a malignant neoplasm (Mishra, 2012). There is a lack of evidence of how each individual lesion should be treated: it can be monitored or removed using a laser (termed laser excision) depending on patient and doctor preference. Unknown progression poses a variety of risks and problems for both the patient and doctor. For a disorder which is destined to become invasive, early knowledge of this progression would help deliver a more targeted approach to treatment and as explained previously, early diagnosis decreases morbidity and mortality from cancer (Mishra, 2012). Biomarkers and Genetic Changes in Oral Cancer A biomarker identified in the initial biopsy of a PMD which predicts the succession of the lesion, could revolutionise management of these areas (Arellano-Garcia et al., 2010). Currently, there is no robust biomarker of this description for OSCC but many possibilities have been documented and tested, the most prominent being EGFR overexpression (Grandis and Tweardy, 1993). Dyplasia grade can give an indication of progression to malignancy but is far from accurate (Kujan et al., 2006b; Kujan et al., 2007). The characteristics of a model biomarker are described in Table 1. Attributes of an Ideal Biomarker Measured objectively Measured in small samples Altered in high-risk tissues compared to normal tissues Altered in early carcinogenesis Table 1. Features required for the ideal biomarker. Adapted from (Wu et al., 2010) Molecular changes in the tissue, for example, loss of heterozygosity (LOH) have been suggested as possible biomarkers for OSCC (Zhang and Rosin, 2001). LOH describes a loss of DNA from a chromosome and can be used to detect areas at risk of cancerous changes. It has been used previously in head and neck cancers to show that the chromosomes coding for the tumour suppressor genes p53 and p16 are affected (Forastiere et al., 2001). These genes are known to be heavily implicated in head and neck tumorigenesis. Another potential novel biomarker for OSCC is a key transcriptional regulator called PAX9. PAX The PAired-boX (PAX) family of genes are essential transcription factors for controlling tissue differentiation and organogenesis during development in embryos (Li and Eccles, 2012). They control these pathways by encoding for transcription factors which will influence the expression of downstream developmental genes (Muratovska et al., 2003). PAX genes are also necessary for mediating cell proliferation, preventing apoptosis and stem-cell self-renewal (Robson et al., 2006). Therefore it is conceivable that dysregulation of the PAX family may be a key step in carcinogenesis (Li and Eccles, 2012). The PAX family consists of 9 different genes (PAX1-PAX9) divided into 4 subgroups according to their structure as shown in Figure 2. The structure of the gene directly relates to the tissues they influence during embryonic differentiation and their effect on cancer development (Muratovska et al., 2003). Paired Box Octapeptide Homeodomain PAX1 Group I PAX9 Improved Prognosis PAX4 Group IV PAX6 PAX2 Group II PAX5 PAX8 Poor Prognosis PAX3 Group III PAX7 Figure 2. Basic structure and sub-classifications of the PAX gene family. The octapeptide may be present or absent and the homeodomain may be present, absent or truncated as seen in group II. Subgroups I and IV are associated with a more positive outcome and decreased malignancy of the cancer whereas groups II and III are the opposite and associated with a worse outcome. (Adapted from (Muratovska et al., 2003; Robson et al., 2006)) PAX9 PAX9 is the main PAX gene responsible for differentiation of the oral structures. Expression of Pax9 (mouse orthologue of PAX9) in the mouse embryo has been studied in depth and shows it is involved in endodermal epithelium formation including oral, tongue and oesophageal stratified squamous epithelium and mesenchymal craniofacial and tooth development (Chi and Epstein, 2006). Genetic defects in PAX9 in humans leads to non- syndromic congenitally missing teeth and in mice will also lead to craniofacial and skeletal abnormalities (Lee et al., 2008). PAX genes are involved in formation of a wide variety of cancers and PAX9 is implicated in oral and oesophageal cancer although the details of this process are unclear (Gerber et al., 2002). PAX9 is associated with a more positive prognosis for cancer and the loss of expression may suggest an increased risk of malignancy compared to a lesion expressing PAX9 (Robson et al., 2006). This theory is supported by Gerber et al when in 2002 they demonstrated that PAX9 expression is reduced in dysplasia and absent in a number of oesophageal cancer specimens. They included at least one area of histologically normal appearing epithelium in every biopsy to act as an internal control. This ‘normal’ tissue retained PAX9 expression. Gerber et al concluded that the PAX9 gene plays a role in the malignant transformation of cells. PAX9 expression is found in the epithelium of oral mucosa biopsies and can be assessed using immunohistochemistry (IHC). Aims and Objectives Aim Assess the efficacy of PAX9 gene expression in predicting the malignant transformation of potentially malignant disorders (PMD) into oral squamous cell carcinoma (OSCC). Objectives Qualitatively determine the PAX9 expression pattern in normal oral tissue, dysplasia and OSCCs Quantitatively determine the PAX9 expression pattern in normal oral tissue and dysplasia Correlate PAX9 expression with patient demographics, dysplasia grade and clinical outcome Methods and Materials Case Selection In total, 199 normal, dysplastic and cancerous oral biopsies were identified and subdivided by clinical outcome as shown in Table 2. Group Name Number Normal Tissue 24 cases No Adverse Outcome 30 cases Recurrence 15 cases New Lesion 11 cases Malignant Transformation 22 cases OSCC 97 cases Table 2. Final groups and case numbers Each biopsy section was stained for PAX9 expression using immunohistochemistry. Controls The normal tissue sections were used as controls for IHC staining. Once batches of PMD slides were stained, they could be compared to normal sections to check that the protocol had worked. If staining was weak or the pattern unexpected, there was often histologically normal appearing epithelium adjacent to a PMD which could be used as an internal control. This epithelium appears disease-free when examined under a microscope. Image Analysis The PMD and normal tissue sections were subject to computer image analysis for positively stained nuclei and strongly positively stained nuclei. A standardised protocol for computer analysis is not currently available; consequently a novel method was developed. Previous investigations suggest that the cancer specimens do not exhibit high PAX9 expression and areas of epithelium can be difficult to isolate thus computer analysis was not carried out for the OSCCs, these were analysed descriptively. This was completed using the Allred scoring system already in use for IHC EGFR staining in breast cancer (Allred et al., 1998). The normal and dysplastic biopsies were also analysed descriptively. Ethical approval was obtained from the National Research Ethics Service (NRES) Committee North East - Sunderland (REC reference: 11/NE/0118). Results PAX9 Staining Examples of the PAX9 staining after computer analysis are shown in Figure 3, 4, 5 and 6. PAX9-positive nuclei are stained brown and the remaining tissue is counterstained blue. The Aperio immunohistochemistry image analysis system highlights strongly stained cells in red, followed by orange then yellow for decreasing intensity. Negative nuclei are highlighted in blue. Figure 3. Aperio screenshot of normal tissue Figure 4. Aperio screenshot of histologically normal tissue Figure 1. Aperio screenshot of histologically normal tissue Figure 1. Aperio screenshot of normal tissue Figure 5. Aperio screenshot of low grade dysplasia Figure 6. Aperio screenshot of high grade dysplasia PAX9 Expression Analysis For the computer analysis, expression was defined by two parameters: percentage positive stained nuclei (PN) and percentage strongly positive stained nuclei (PN+). For the Allred analysis, expression was defined by a combined score for intensity and proportion of nuclei stained. No significant relationship was found between PAX9 expression and patient age, sex or lesion sub-site for both PN and PN+. Significance was found between dysplasia grade and clinical outcome. Figure 7 demonstrates that PAX9 expression falls in all grades of dysplasia including histologically normal appearing epithelium adjacent to PMD. Figure 7. PN and PN+ means for WHO dysplasia grading system 80 70 62.6 PN PN+ 60 50 36.7 31.2 % 40 30 23.6 25.8 22.2 20 6.3 10 4.1 2.8 3.8 2.8 0.0 0 Normal Histologically Normal Mild Moderate Severe CIS All groups for PN (p<0.03) and PN+ (p<0.045) are significantly lowered compared to normal tissue. Histologically normal tissue was significantly higher in PN for mild dysplasia (p=0.048), moderate dysplasia (p=0.06) and CIS (p=0.042) No other realtionships were found. Figure 8 shows the relationship between PAX9 expression and clinical outcome. Figure 8. PN and PN+ means for all clinical outcome groups 80 62.6 PN 70 60 PN+ 45.8 50 % 40 30 25.7 23.3 14.8 14.3 20 10 1.2 3.3 0.1 9.1 0 Normal No Adverse Outcome Recurrence New Lesion Transformed PN (p<0.025) and PN+ (p<0.001) are significantly lowered in disease compared to normal tissue. The transformed group expression was also statistically elevated compared to all the other outcome groups in PN (p<0.02) and all groups apart from new lesion in PN+ (p<0.01). Using the Allred scores to include the T1 and T2 cancers, expression follows the pattern as shown in Figure 9. Figure 9. Allred score means for all clinical outcome groups including OSCC 8 7.2 7 5.7 Allred Score 6 4.7 5 4.0 4.1 3.3 4 3 2 1 0 Normal No Adverse Outcome Recurrence New Lesion Transformed T1, T2 OSCC All groups including the OSCC group have a significantly decreased PAX9 expression compared to normal tissue (p<). All groups apart from new lesion display a significantly lowered PAX9 expression compared to the transformed group (p<). Kaplan-Meier survival curves were created from the above data. Interestingly, they demonstrate that 90% of dysplasias with a relatively higher proportion of PAX9-positive nuclei transformed into oral cancer within 80 months of diagnosis (Figure 10). Figure 20. Kaplan-Meier Curve for Malignant Transformation in Dysplasia Patients: Aperio PN in Thirds. The curve shows 90% of dysplastic lesions with PN values of >40% transformed into cancer compared to 41% of lesions with PN values of 21-40% and 37% of patients with 0-20% expression up to 76 months after diagnosis Discussion There have been some interesting results produced by this investigation. A new quantitative method for IHC image analysis has been very successful. With optimisation of the protocol, this could prove to be a very powerful analysis tool. The PAX9 expression throughout cancer formation is not as straight-forward as expected. Within this patient cohort, PAX9 expression is decreased in dysplastic potentially malignant disorders compared to disease-free tissue including in histologically normal appearing epithelium. This implies PAX9 expression may be used as a screening tool to identify epithelium in very early stages of ‘invisible’ carcinogenesis. In a clinical setting, the PAX9 expression pattern could be used by the pathologist to determine if a clear margin has been left by the surgeon after laser excision of the lesion. Alternatively, if a patient presents with a PMD, biopsies from nearby sub-sites can be taken to determine the spread of disease. From here, the relatively higher PAX9 expression biopsies were more likely to transform into cancer suggesting PAX9 moves from a potential tumour-suppressor role as previously suggested to a tumour-promoter role. A transient upregulation of PAX9 may be causally involved in the transformation to cancer. If this is the case, patients may need to have the PAX9 expression in their dysplastic lesion reviewed on a regular basis to identify this increase before expression falls again in cancer. Conclusion In conclusion, PAX9 is a promising prognostic marker which meets all of the criteria for an ideal biomarker. At present PAX9 expression can act as an aid to current prognostic tests but cannot replace these until more is known about the mechanisms of action. Further investigations using a larger patient cohort with standardised treatments will be required. WORDS: 1946 Bibliography Allred DC, Harvey JM, Berardo M, Clark GM (1998). Prognostic and predictive factors in breast cancer by immunohistochemical analysis. Mod Pathol 11:155-168. Arellano-Garcia ME, Li R, Liu X, Xie Y, Yan X, Loo JA, et al. (2010). Identification of tetranectin as a potential biomarker for metastatic oral cancer. Int J Mol Sci 11:3106-3121. Bancroft D, Gamble M (2008). Theory and Practice of Histological Techniques: Elsevier Health Sciences. Baykul T, Yilmaz HH, Aydin U, Aydin MA, Aksoy M, Yildirim D (2010). Early diagnosis of oral cancer. J Int Med Res 38:737-749. Braakhuis BJ, Tabor MP, Kummer JA, Leemans CR, Brakenhoff RH (2003). A genetic explanation of Slaughter's concept of field cancerization: evidence and clinical implications. Cancer Res 63:1727-1730. Cancer Research (2009). Oral cancer - UK incidence statistics. Cancer Research UK. Available at: http://info.cancerresearchuk.org/cancerstats/types/oral/incidence/ (accessed: 30/05/2012). Chi N, Epstein JA (2006). Getting your Pax straight: Pax proteins in development and disease. Trends Genet 18:41-47. Forastiere A, Koch W, Trotti A, Sidransky D (2001). Head and neck cancer. N Engl J Med 345:1890-1900. Gerber JK, Richter T, Kremmer E, Adamski J, Hofler H, Balling R, et al. (2002). Progressive loss of PAX9 expression correlates with increasing malignancy of dysplastic and cancerous epithelium of the human oesophagus. J Pathol 197:293-297. Grandis JR, Tweardy DJ (1993). Elevated levels of transforming growth factor alpha and epidermal growth factor receptor messenger RNA are early markers of carcinogenesis in head and neck cancer. Cancer Res 53:3579-3584. Kujan O, Glenny AM, Oliver RJ, Thakker N, Sloan P (2006a). Screening programmes for the early detection and prevention of oral cancer. Cochrane Database Syst Rev 19:1-28. Kujan O, Oliver RJ, Khattab A, Roberts SA, Thakker N, Sloan P (2006b). Evaluation of a new binary system of grading oral epithelial dysplasia for prediction of malignant transformation. Oral Oncol 42:987-993. Kujan O, Khattab A, Oliver RJ, Roberts SA, Thakker N, Sloan P (2007). Why oral histopathology suffers inter-observer variability on grading oral epithelial dysplasia: an attempt to understand the sources of variation. Oral Oncol 43:224-231. Lee JC, Sharma M, Lee YH, Lee NH, Kim SY, Yun JS, et al. (2008). Pax9 mediated cell survival in oral squamous carcinoma cell enhanced by c-myb. Cell Biochem Funct 26:892-899. Li CG, Eccles MR (2012). PAX Genes in Cancer; Friends or Foes? Front Genet 3:1-7 Mehrotra R, Gupta DK (2011). Exciting new advances in oral cancer diagnosis: avenues to early detection. Head Neck Oncol 3. Mishra R (2012). Biomarkers of oral premalignant epithelial lesions for clinical application. Oral Oncol. Muratovska A, Zhou C, He S, Goodyer P, Eccles MR (2003). Paired-Box genes are frequently expressed in cancer and often required for cancer cell survival. Oncogene 22:7989-7997. OCIU (2010). Profile of Head and Neck Cancers in England: Incidence, Mortality and Survival. Oxford: National Cancer Intelligence Network. Petersen PE (2009). Oral cancer prevention and control--the approach of the World Health Organization. Oral Oncol 45:454-460. Reibel J (2003). Prognosis of oral pre-malignant lesions: significance of clinical, histopathological, and molecular biological characteristics. Crit Rev Oral Biol Med 14:47-62. Robson EJ, He S, Eccles MR (2006). A PANorama of PAX genes in cancer and development. Nat Rev Cancer 6:52-62. Slaughter DP, Southwick HW, Smejkal W (1953). Field cancerization in oral stratified squamous epithelium; clinical implications of multicentric origin. Cancer 6:963-968. Tabor MP, Brakenhoff RH, van Houten VM, Kummer JA, Snel MH, Snijders PJ, et al. (2001). Persistence of genetically altered fields in head and neck cancer patients: biological and clinical implications. Clin Cancer Res 7:1523-1532. van der Waal I (2009). Potentially malignant disorders of the oral and oropharyngeal mucosa; terminology, classification and present concepts of management. Oral Oncol 45:317-323 Werning JW (2007). Oral Cancer: Diagnosis, Management, and Rehabilitation New York: Thieme Medical Publishers. Zhang L, Rosin MP (2001). Loss of heterozygosity: a potential tool in management of oral premalignant lesions? J Oral Pathol Med 30:513-520