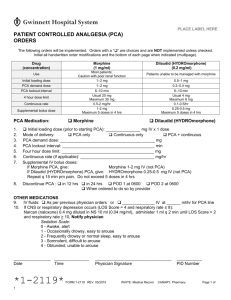
Pain Management Summary
advertisement

Harborview Pain Management Orientation Summary “People will forget what you say and what you did, but people will never forget how you made them feel.” Maya Angelou Pain assessment is an ongoing process. Routinely screen for pain. Pain will be assessed at baseline and at regular intervals after starting the treatment plan, with each new report of pain, at an appropriate interval following pain relief interventions and more frequently as defined in specific pain management procedures. One identified (new pain or significant change), minimum assessment = location, severity, character, goal for pain relief Use a multimodal approach to pain treatment. The relief of pain includes both drug and non-drug interventions. Non-drug interventions include physical modalities (heat/cold, repositioning, massage), cognitive behavioral techniques (relaxation, imagery, distraction, music) and environmental modifications. Administer analgesics in a timely, logical, and coordinated manner tailored to meet individual and changing needs. Engage the patient in realistic goals and the treatment plan. Provide information to the patient and family when possible regarding the importance of effective pain relief, the pain treatment plan, possible risks associated with pain treatment, and how to participate in the pain treatment plan including communicating progress toward the pain management goal. “It is generally not possible or safe to eliminate all pain, but our goal is to reduce your pain to a reasonable level as well as manage any unpleasant side effects of pain medicines and help you recover.” Safety Reminders!! Always routinely perform safety checks: at times of handover trace lines, be sure lines are labeled, tubing is appropriate (yellow striped for Epidurals and PNC; tubing vent open if glass bottle infusing) and pump programming and medication matches current order. Perform sedation and respiratory assessment before rousing the patient. Reinforce teaching; instruct family and visitors to NOT assist patient with IV PCA. Provide extra vigilance with the patient is on other CNS depressants. Don’t chase unrealistic numeric pain intensity ratings with opioids. Use a multimodal approach. 0.2mg of IV hydromorphone is approximately equal to 1.3mg of IV morphine 2.0 mg of IV hydromorphone is approximately equal to 13.3 mg of IV morphine or 40mg PO morphine! Ways to help Improve Patient Satisfaction with pain management o Individualize patient care to partner with patients o Use key words “I want to do everything I can to make you as comfortable as possible. Keeping your pain managed is important. Tell me about your pain right now” o Alleviate anxiety (explain rounding) o Tell the patient when next dose of pain medicine is coming o Use the whiteboard and encourage communication and address pain at handovers o Provide complete explanation for new/modified interventions o Seek alternatives to pain medicine o Reposition the patient (basic comfort measures) • • • • • • • • • • IV PCA Assess/document every 2 hrs for 8 hrs, then Q 4 hrs • Resp rate and depth (full minute before stimulation) • Serial sedation levels • Pain intensity • Side effects Total PCA dose is documented every 8 hrs, pump cleared PCA-by-proxy - instruct family/friends NOT to assist the patient with IV PCA A 2-person (RN) independent double check of PCA settings/medication is required at initiation of PCA therapy and following any changes (and at start of each shift for peds) Epidural Analgesia Assess/document every 2 hrs for 24 hrs, then Q 4 hrs • Resp rate and depth (full minute before stimulation) • Sedation level • Pain intensity • Side effects If Local Anesthetic: Assess/document BP, HR, sensory level and motor strength every 30 minutes for 2 hrs, hourly for 4 hrs, then every 4 hrs Vasodilation common results in orthostatic BP Assess the site/position of the catheter every shift May reinforce the dressing around tegaderm; do NOT replace to avoid dislodgement of catheter Bolus doses via pump only: except (fentanyl) see policy • • Peripheral Nerve Catheters Assess/document every 1 hrs for 4 hrs, then Q 4 hrs (and after an increase in rate or concentration) • BP, HR • Pain intensity • Neuro-vascular check of affected extremity: color, temp, sensation, motion Observe/report signs of systemic local anesthetic toxicity -Very rare rates <20mL/hr – ringing in ears, periorbital paresthesia, nausea Q/Policies Harborview/Orientation Syllabus Summary Sheet_Pain_Gordon