Sample Policy and Procedure for Providing Mini BAL Medical
advertisement
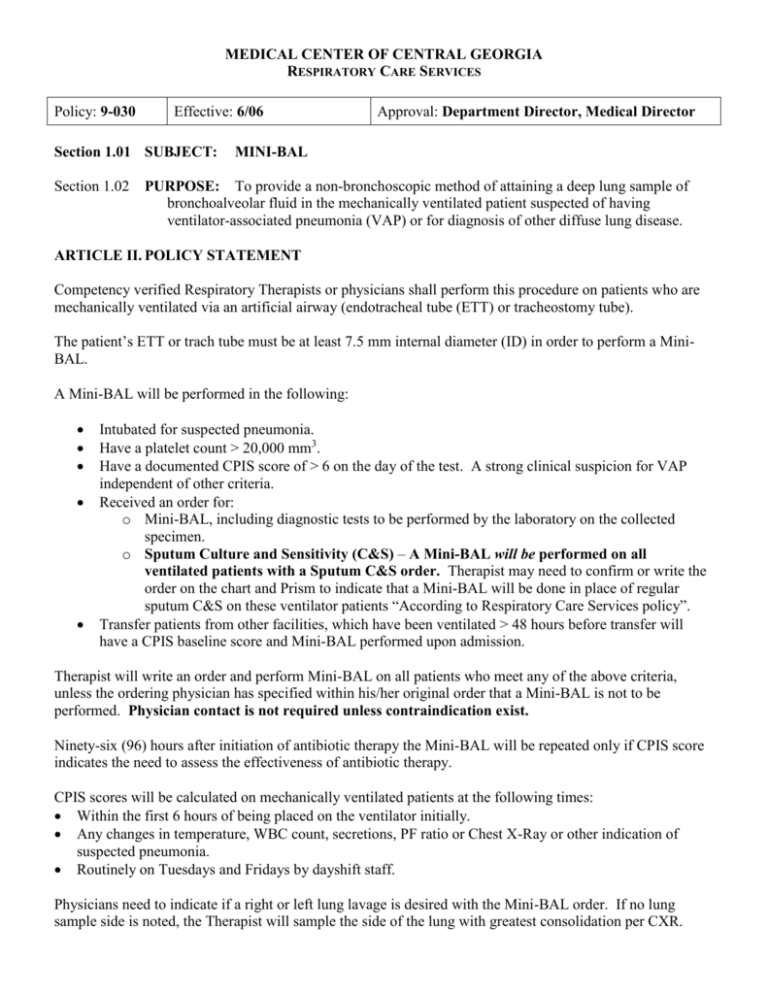
MEDICAL CENTER OF CENTRAL GEORGIA RESPIRATORY CARE SERVICES Policy: 9-030 Effective: 6/06 Section 1.01 SUBJECT: Section 1.02 Approval: Department Director, Medical Director MINI-BAL PURPOSE: To provide a non-bronchoscopic method of attaining a deep lung sample of bronchoalveolar fluid in the mechanically ventilated patient suspected of having ventilator-associated pneumonia (VAP) or for diagnosis of other diffuse lung disease. ARTICLE II. POLICY STATEMENT Competency verified Respiratory Therapists or physicians shall perform this procedure on patients who are mechanically ventilated via an artificial airway (endotracheal tube (ETT) or tracheostomy tube). The patient’s ETT or trach tube must be at least 7.5 mm internal diameter (ID) in order to perform a MiniBAL. A Mini-BAL will be performed in the following: Intubated for suspected pneumonia. Have a platelet count > 20,000 mm3. Have a documented CPIS score of > 6 on the day of the test. A strong clinical suspicion for VAP independent of other criteria. Received an order for: o Mini-BAL, including diagnostic tests to be performed by the laboratory on the collected specimen. o Sputum Culture and Sensitivity (C&S) – A Mini-BAL will be performed on all ventilated patients with a Sputum C&S order. Therapist may need to confirm or write the order on the chart and Prism to indicate that a Mini-BAL will be done in place of regular sputum C&S on these ventilator patients “According to Respiratory Care Services policy”. Transfer patients from other facilities, which have been ventilated > 48 hours before transfer will have a CPIS baseline score and Mini-BAL performed upon admission. Therapist will write an order and perform Mini-BAL on all patients who meet any of the above criteria, unless the ordering physician has specified within his/her original order that a Mini-BAL is not to be performed. Physician contact is not required unless contraindication exist. Ninety-six (96) hours after initiation of antibiotic therapy the Mini-BAL will be repeated only if CPIS score indicates the need to assess the effectiveness of antibiotic therapy. CPIS scores will be calculated on mechanically ventilated patients at the following times: Within the first 6 hours of being placed on the ventilator initially. Any changes in temperature, WBC count, secretions, PF ratio or Chest X-Ray or other indication of suspected pneumonia. Routinely on Tuesdays and Fridays by dayshift staff. Physicians need to indicate if a right or left lung lavage is desired with the Mini-BAL order. If no lung sample side is noted, the Therapist will sample the side of the lung with greatest consolidation per CXR. Policy # Page 2 of 7 Physician must be present if radiologic assisted or fluro assisted Mini-BAL is to be performed. Tube feedings should be turned off 30 minutes to 1 hour prior to procedure. For VAP analysis, the laboratory requisition should specify and be ordered as Bronchoalveolar Lavage Culture, Quantitative or Culture, Bronchoalveolar Lavage and marked stat or priority. Additional lab orders for specific cytology or histology tests must be ordered in Prism and sent on a separate request with the Mini-BAL culture to the lab. For example, if a gram stain is needed, the physician must specify this on the order and it must be entered into Prism separately. All samples are to be labeled with the patient ID label and "BAL" written in bold letters on the label that is included in the specimen trap. The procedure will utilize 60 – 120 ml (instilled in two(2), 30 ml aliquots) of saline to ensure an adequate sample size. No more than a total of 4 separate (30 ml) aliquots shall be instilled during this procedure. Sample size for VAP analysis should be at least 5 ml. Larger sample size will be required for additional testing. In general, approximately 40% of the instilled saline should be returned during suctioning. Coordinate with the lab on how large a sample will be required depending on the tests ordered. Closely monitor patient prior to and throughout the procedure. Immediately terminate the procedure with any evidence of desaturation, arrhythmias, hemodynamic instability, or patient intolerance to procedure. Notify the physician and document the results. This policy and procedure has been written specifically for the BAL Cath from Kimberly-Clark. BAL Cath kits, 120 ml cups of Normal Saline (NS) and large leuki traps will be stocked in the Respiratory Care Services (RCS) supply room. ARTICLE III. DEFINITION(S) BAL: Bronchoalveolar Lavage BAL Cath: Is a catheter within a catheter (figure 1). The 12 Fr inner catheter is covered by a 16 Fr outer sheath. The design permits the advancement of the inner catheter into the distal bronchial segments while reducing exposure to upper airway microorganisms. The inner catheter tip is radiopaque. CPIS: Clinical Pulmonary Infection Score is performed by using the scoring the following parameters: CPIS Parameter Temperature (oC) < 36.5 ≥ 36.5 and ≤ 38.4 ≥ 38.5 and ≤ 38.9 ≥ 39.0 CPIS Score 2 0 1 2 WBC Count < 4,000 & band forms ≥50% 2 Policy # Page 3 of 7 ≥ 4,000 and ≤ 11, 000 < 4,000 > 11,000 > 11,000 & band forms ≥50% 0 1 1 2 Tracheal Secretions: None or Scant Non-Purulent Purulent 0 1 2 PaO2/FIO2: > 240, ARDS* or Pulmonary Contusion 0 ≤ 240 and no ARDS* 2 * ARDS is defined as P/F ≤200, PAWP ≤ 18 mmHg and acute bilateral infiltrates Chest X-Ray No infiltrate 0 Diffuse (or patchy) infiltrate 1 Localized Infiltrate 2 CPIS TOTAL ACTION Evaluate for other potential ≤ 6 and low suspicion for VAP sources of infection ≤ 6 and high suspicion for VAP Evaluate as if CPIS > 6 Order & perform a Mini>6 BAL (A) ROLES AND RESPONSIBILITIES RRT/RCP W/O Team Members Performing Procedure (W= with supervision, W/O = without supervision) CRT/RCP RCP Student Education/Competency If no, still responsible for knowing P&P! Yes/No Type a. Ventilator associated pneumonia (VAP) in-service with post test. b. Mini-BAL procedure in-service Yes c. Mini-BAL procedure direct observation. Therapist will perform 3 observed procedures with a supervisor or RCS Education Staff. A Mini-BAL Competency Evaluation sheet will be completed on each review. d. A peer will observe Supervisors and Education Staff. A Mini-BAL Competency Evaluation Sheet will be completed. e. Mini-BAL procedure direct observation. Therapist will perform observed procedure with a supervisor or RCS Education Staff. A Mini-BAL Competency Evaluation sheet will be completed. Frequency Initial service implementation Department orientation. Initial service implementation ICU department orientation Initial service implementation ICU department orientation Every three years Every three years Policy # Page 4 of 7 Applicable Areas All Patient Areas or Department Operations (DO) Adult Areas Pediatric Areas All Adult ICUs Only if the artificial airway size is at least 7.5 mm ID! Specific Units: List (B) CONTRA-INDICATIONS There are no absolute contra-indications for Mini-BAL, however, if the patient has any of following the Therapist must discuss and document with the Ordering Physician before performing the procedure! Asthma with moderate airway obstruction Hypercapnia Hypoxemia that cannot be corrected to saturation greater than 90% Serious cardiac arrhythmias Myocardial infarction (MI) within the previous 6 weeks Uncorrected bleeding susceptibility Hemodynamic instability Severe bleeding of unknown origin Elevated intercranial pressure (ICP) PEEP > 15 cmH2O (C) PRECAUTIONS/SIDE EFFECTS Bronchospasm Pneumonitis Bleeding Hypoxemia Hypercapnia Arrhythmias Pneumothorax Airway trauma Vomiting/Aspiration Post procedure fever (D) EQUIPMENT BAL Cath Kit 120 ml cup of Normal Saline (NS) – RCS supply room. 2 - 60 ml syringes Large Leuki or sputum trap Suction tubing Gloves, gown and eye protection or other Personal Protective Equipment (PPE). 4% Lidocaine (optional) (E) INFECTION CONTROL Procedure equipment and gloves need not be maintained as sterile, but aseptic technique should be used. (F) Policy # Page 5 of 7 (G) IMPLEMENTING PROCEDURES 1. Refer to policy and procedure “Tasks Common to All Clinical Activities”. 2. Make sure tube feedings have been off 30 minutes to 1 hour prior to procedure. 3. Confirm that a CPIS of > 6 exists on the day of the order or that the procedure is ordered based on suspicion of VAP. 4. Confirm order for BAL with “quantitative cultures”. Note if specific right or left lung lavage is ordered. 5. Review latest CXR. 6. If Lidocaine is going to be administered verify any medication allergies. 7. Suction patient with regular in-line catheter before procedure. 8. Pre-oxygenate the patient at 100% FIO2 via the ventilator for at least 5 - 10 minutes before the procedure and throughout the procedure. 9. Administer 2 ml of 4% Lidocaine down the ETT or trach. (optional) 10. Draw up 60 ml of normal saline from the bottle into 2 different 60 cc syringes and set aside in a clean field for installation later in the procedure. 11. Connect the suction and set your vacuum pressure to 80 mmHg for the procedure. Be sure to place the leuki trap in-line between the suction adapter and sterile suction tubing provided. 12. Attach the graduated suction adapter to three-way stopcock on the inner catheter and close the stopcock to the suction (figure 1e). 13. Remove sterile protective cover from tip of BAL catheter. 14. Pass the BAL Cath through the access port elbow about 1.5 cm (figure 3). Do not contaminate the BAL Cath tip prior to insertion. 15. Remove the in-line suction device and attach the BAL Cath adapter to the ETT or trach tube while guiding the catheter tip into the ETT or trach tube lumen. 16. Reconnect and maintain mechanical ventilation. 17. Rotate oxygen adapter port (figure 1d) to either the 3:00 (right) or 9:00 (left) position for left or right lung sample specificity. 18. Advance the outer catheter into the ETT until the numbers on the catheter and the ETT match. This will place the end of the catheter at the end of the ETT. 19. Flush the tip of the BAL Cath by instilling 2 ml of saline through the inner catheter via the three-way stopcock. 20. Once the ETT and catheter numbers match advance the outer catheter 3 - 5 cm further into the right or left mainstem bronchus. Distance depends on ETT placement and/or patient size. . Re-check that the right or left lung position is still correct after advancement by looking at the oxygen adapter port position. 21. On inspiration, advance the inner catheter 2 – 3 cm or until you feel resistance. This should place the inner catheter in a wedge position (figure 2). 22. Lock the catheter in place with the blue slide lock (figure 3c). 23. Special Note for ventilated trach tubes: a) Shiley # 8 i) Insert outer catheter to 16cm at the flange. Check directional port to ensure insertion into either the right or left lung. ii) Insert outer catheter and additional 3 – 5 cm. iii) Insert inner catheter 2 – 3 cm or until resistance is met. iv) Lock the catheter in place with the blue slide lock (figure 3c). b) Shiley # 6 i) Insert outer catheter to a total depth of 16cm. Be sure to check directional port while inserting, to ensure insertion into either the right or left lung. ii) Insert inner catheter 2 – 3 cm or until resistance is met. iii) Lock the catheter in place with the blue slide lock (figure 3c). Do not force the catheter further. Policy # Page 6 of 7 24. Turn the 3-way stopcock off to suction and gently instill 30 ml aliquots of saline and then turn the stopcock off to the saline syringe and suction the specimen into the leuki trap that was placed in-line. 25. Turn the 3-way stopcock off to suction and gently instill another 30 ml aliquot of saline. Then turn the stopcock off to the saline syringe and suction the specimen into the leuki trap. Additional aliquots of saline may be used to obtain a larger sample, if need, per policy. 26. Remove the leuki trap from the suction line after collection to protect the sample. 27. Unlock the blue lock device and completely withdraw the inter catheter until the black dot (figure 1f) is past the oxygen port. 28. Withdrawal the outer catheter until approximately 1.5 cm is remaining beyond the access port elbow (figure 3). 29. Remove the BAL Cath adapter from the ETT or trach tube. 30. Reconnect the patient to the ventilator. 31. Mini-BAL sample must be labeled with patient ID sticker and use the sticker in with the trap to record; “Mini-BAL” date, time and initials. 32. The Mini-BAL sample must be placed in biohazard bag and bubble wrap in order to be “tubed” to the Central Processing lab. 33. Immediately after the procedure is completed, send Mini-BAL specimen to Central Processing Lab. The specimen must be in the lab with-in 30 minutes after being collected. 34. Document the procedure and patient response. 35. Notify the nurse and physician of any and all complications. Special Procedure Note – Non Ventilated Trach Patients (ICU – TCU areas ONLY!) 1. 2. 3. 4. 5. 6. 7. Work with nursing to obtain & provide sedation medications prior to starting the procedure. Place patient on 100% FIO2 Assess the patient’s pre procedure SpO2 level. Bag patient for three (3) minutes prior to starting the procedure on, 100% FIO2. Bag the patient during the procedure Follow the procedures steps identified above to perform the procedure. Post collection procedure: a) Bag the patient for 3 -5 minutes 100% FIO2. b) Observe and assess the patient for any signs of desaturation. c) Increase FIO2 as necessary to maintain the patient’s pre procedure SpO2 levels. Documentation & Forms Required Paper Properly label the sample sent to Documentation: lab as noted above. Billing: New: Revised: Supersedes: 7/05 Date: 3/06, 6/06 Date: 3/06 Electronic Prism – Complete the on-line documentation that is associated with the Mini-BAL task/order. Mini-BAL is charged in Prism after the documentation is completed. The procedure can also be billed using the Ad Hoc charging function. Policy # Page 7 of 7 References: Kimberly-Clark BAL Cath instruction sheet (R8629A 12/02), company representative inservices, BAL Cath PowerPoint in-service (2/05), BAL Cath Group Meeting PowerPoint Presentation (2/05) and BAL Cath Procedure Video (12/04). Figures: Figure 1 a. Inner Catheter b. Outer Catheter c. Directional tip d. Oxygen port e. 3-way stopcock f. Inner catheter withdrawal mark Figure 2 – Inner catheter in the “wedge” sample position Figure 3 ETT or trach tube connection Access port elbow Blue slide lock