tibialis posterior tendon insufficiency
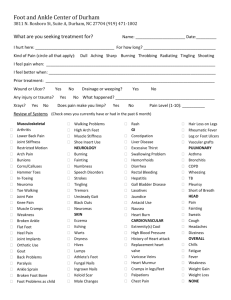
advertisement
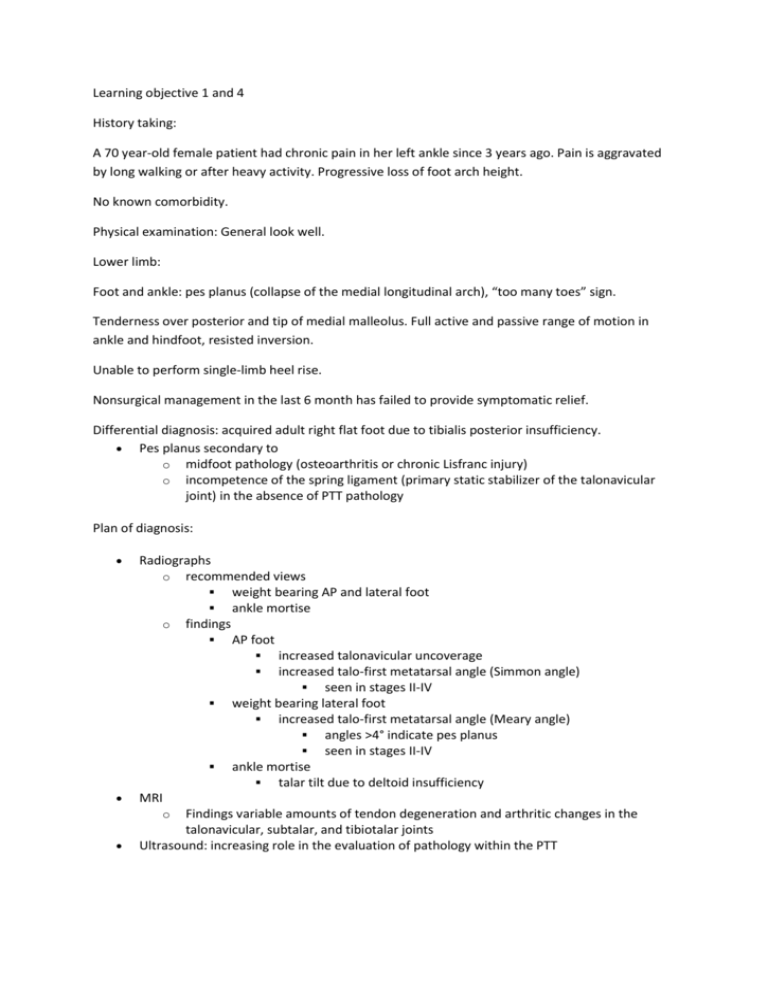
Learning objective 1 and 4 History taking: A 70 year-old female patient had chronic pain in her left ankle since 3 years ago. Pain is aggravated by long walking or after heavy activity. Progressive loss of foot arch height. No known comorbidity. Physical examination: General look well. Lower limb: Foot and ankle: pes planus (collapse of the medial longitudinal arch), “too many toes” sign. Tenderness over posterior and tip of medial malleolus. Full active and passive range of motion in ankle and hindfoot, resisted inversion. Unable to perform single-limb heel rise. Nonsurgical management in the last 6 month has failed to provide symptomatic relief. Differential diagnosis: acquired adult right flat foot due to tibialis posterior insufficiency. Pes planus secondary to o midfoot pathology (osteoarthritis or chronic Lisfranc injury) o incompetence of the spring ligament (primary static stabilizer of the talonavicular joint) in the absence of PTT pathology Plan of diagnosis: Radiographs o recommended views weight bearing AP and lateral foot ankle mortise o findings AP foot increased talonavicular uncoverage increased talo-first metatarsal angle (Simmon angle) seen in stages II-IV weight bearing lateral foot increased talo-first metatarsal angle (Meary angle) angles >4° indicate pes planus seen in stages II-IV ankle mortise talar tilt due to deltoid insufficiency MRI o Findings variable amounts of tendon degeneration and arthritic changes in the talonavicular, subtalar, and tibiotalar joints Ultrasound: increasing role in the evaluation of pathology within the PTT Weight bearing lateral radiograph of the foot shows longitudinal arch collapse MRI: Sagital STIR image shows a tibialis posterior insufficiency and tenosynovitis. Treatment plan: Nonoperative o immobilization in walking cast/boot for 3-4 months indications first line of treatment in stage I disease o custom-molded in-shoe orthosis indications stage I patients after a period of immobilization stage II patients technique medial heel lift and longitudinal arch support medial forefoot post indicated if fixed forefoot varus is present UCBL with medial posting o ankle foot orthosis indications stage II, III, and IV patients who are not operative candidates, are sedentary and low demand (age > 60-70) technique AFO family of braces (Arizona, molded, articulating) AFO found to be most effective want medial orthotic post to support valgus collapse Arizona brace is a molded leather gauntlet that provides stability to the tibiotalar joint, hindfoot, and longitudinal arch Operative o tenosynovectomy indications indicated in stage I disease if immobilization fails o FDL transfer, calcaneal osteotomy, TAL, +/- forefoot correction osteotomy, +/- spring ligament repair, +/- lateral column lengthening, +/- PTT debridement indications stage II disease o o o contraindications hypermobility neuromuscular conditions severe subtalar arthritis obesity (relative) age >60-70 (relative) triple arthrodesis and TAL indications stage III disease stage II disease with severe subtalar arthritis triple arthrodesis and TAL + deltoid ligament reconstruction indications stage IV disease with passively correctable ankle valgus tibiotalocalcaneal arthrodesis indications: stage IV disease with a rigid hindfoot, valgus angulation of the talus, and tibiotalar and subtalar arthritis