File - Shabeer Dawar
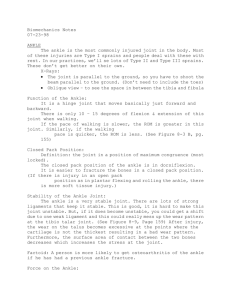
advertisement

Lecture-1 BIO-MECHANICS OF ANKLE-FOOT JOINT objectives An over view of Foot Ankle joint general consideration Proximal joint surface of ankle joint Distal joint surface of ankle joint Capsular support of ankle joint Ligamentous support of ankle joint Osteo kinematics of ankle Arthro kinematics of ankle joint Introduction The ankle/foot complex is structurally analogous to the wrist-hand complex of the upper extremity but has a number of distinct differences to optimize its primary role to bear weight. The complementing structures of the foot allow the foot to sustain large weight-bearing stresses under a variety of surfaces and activities that maximize stability and mobility. The ankle/foot complex must meet the stability demands of: – (1) providing a stable base of support for the body in a variety of weight-bearing postures without excessive muscular activity and energy expenditure and – (2) acting as a rigid lever for effective push-off during gait. The stability requirements can be contrasted to the mobility demands of: – (1) dampening rotations imposed by the more proximal joints of the lower limbs, – (2) being flexible enough to absorb the shock of the superimposed body weight as the foot hits the ground, and – (3) permitting the foot to conform to a wide range of changing and varied terrain. The ankle/foot complex meets these diverse requirements through the integrated movements of its 28 bones that form 25 component joints. These joints include: – – – – – – – the proximal and distal tibiofibular joints; the talocrural, or ankle, joint; the talocalcaneal, or subtalar, joint; the talonavicular and the calcaneocuboid joints (transverse tarsal joints); the five tarsometatarsal joints; five metatarsophalangeal joints; and nine interphalangeal joints. To facilitate description and understanding of the ankle/foot complex, the bones of the foot are traditionally divided into three functional segments. These are: – the hindfoot (posterior segment), composed of the talus and calcaneus; – the midfoot (middle segment), composed of the navicular, cuboid, and three cuneiform bones; and – the forefoot (anterior segment), composed of the metatarsals and the phalanges These terms are commonly used in descriptions of ankle or foot dysfunction or deformity and are similarly useful in understanding normal ankle and foot function. Kinematics of Foot Gross motion occurs in three planes – Flexion/extension – sagittal plane – Abduction/adduction – transverse plane – Inversion/eversion – frontal plane Supination –inversion/flexion/adduction Pronation- eversion/extension/abduction WB range differs from NWB ER/IR of leg affects arch of foot valgus (or calcaneo valgus ) – increase in medial angle b/w calcaneus and posterior leg. varus (or calcaneovarus) – decrease in medial angle b/w calcaneus and posterior leg Proximal Articular Surfaces The proximal segment of the ankle is composed of the concave surface of the distal tibia and of the tibial and fibular malleoli. These three facets form an almost continuous concave joint surface that extends more distally on the fibular (lateral) side than on the tibial (medial) side and more distally on the posterior margin of the tibia than on the anterior margin. The structure of the distal tibia and the malleoli resembles and is referred to as a mortise. Distal Tibiofibular Joint The distal tibiofibular joint is a syndesmosis, or fibrous union, between the concave facet of the tibia and the convex facet of the fibula. The distal tibia and fibula do not actually come into contact with each other but are separated by fibroadipose tissue. Although there is no joint capsule, there are several associated ligaments at the distal tibiofibular joint. Because the proximal and distal joints are linked (the tibia, fibular, and tibiofibular joints are part of a closed chain), all the ligaments that lie between the tibia and fibular contribute to stability at both joints. Distal Articular Surface The body of the talus forms the distal articulation of the ankle joint. The body of the talus has three articular surfaces: a large lateral (fibular) facet, a smaller medial (tibial) facet, and a trochlear (superior) facet. The large, convex trochlear surface has a central groove that runs at a slight angle to the head and neck of the talus. The body of the talus also appears wider anteriorly than posteriorly, which gives it a wedge shape. The degree of wedging may vary among individuals, with no wedging at all in some and a 25% decrease in width anteriorly to posteriorly in others. The articular cartilage covering the trochlea is continuous with the cartilage covering the more extensive lateral facet and the smaller medial facet. The structural integrity of the ankle joint is maintained throughout the ROM of the joint by a number of important ligaments. Prox TF jt – – – – Flat facet Incline Sup / inf sliding Fibular rotation Ant post Tibiofibular lig (At proximal n distal both) TF Syndesmosis Ant /post TF lig Interosius membrane Crural tibio fibular inter lig Fibula non wt bearing ANKLE JOINT: Synovial hinge jt Oblique axis One degree freedom DF/PF (movt) Ligamentous support of ankle joint Two other major ligaments maintain contact and congruence of the mortise and talus and control medial-lateral joint stability. These are the medial collateral ligament (MCL) and the lateral collateral ligament (LCL). Deltoid ligament Tibialis Posterior Tendon Navicular --- medial collateral ligament (MCL) The MCL is most commonly called the deltoid ligament cx fan shaped Origion and insertion: Arise 4m tibial malleolus and insert in a continuous line on the navicular bone anteriorly and on the talus and calcaneus distally and posteriorly. Mcl control and limits…. control medial distraction stresses on the ankle joint limits motion at the extremes of joint range, particularly with calcaneal eversion. Valgus force fracture displace tibial melloli before ligament tears. lateral collateral ligament (LCL). The LCL is composed of three separate bands that are commonly referred to as separate ligaments. These are the anterior and posterior talofibular ligaments and the calcaneofibular ligament, LCL control and limits: The LCL helps control varus stresses that result in lateral distraction of the joint check extremes of joint ROM, particularly calcaneal inversion. Ligaments Ant Talo Fibular weakest and most commonly torn ligament is most easily stressed when ankle is in a plantarflexed and inverted position Rupture of the anterior talofibular ligament often results in anterolateral rotatory instability posterior talofibular ligament is the strongest of collateral ligaments and is rarely torn in isolation. dorsiflexion of head of talus dorsally (or upward) Body of talus moves posteriorly in mortise. Plantar flexion is the opposite motion talus may rotate slightly within the mortise in both transverse plane around a vertical axis (talar rotation or talar abduction/adduction) and in the frontal plane around an A-P axis (talar tilt or talar inversion/eversion) 7 of medial rotation and 10 of lateral rotation in the transverse plane. Talar tilt (A-P axis) averages 5 or less Ext rotation of 9 degrees from neutral to 30 degrees of dorsiflexion 0-10 degrees of plantar flexion, talus internally rotate 1.4 degrees At 30 degree of plantar flexion, talus ext rotate to 0.6 degrees. Osteokinematics of ankle joint range of motion (ROM) 0-20º for ankle dorsiflexion 0-55º for ankle plantar flexion Joints of mid foot contribute 10-41% of plantarflexion from neutral to 30 degrees of plantarflexion. Gait: Heel strike: slight plantar flexion Increases till flat foot Mid stance dorsiflexion starts. Toe off : plantar flexion Middle of swing phase: dorsiflexion Slight plantar flexion at heel strike. Max dorsiflexion at 70 % of stance Max plantar flexion at toe off. arthrokinematic movements (convex on concave) posterior glide of the talus on the ankle mortise with ankle dorsiflexion anterior glide of the talus on the ankle mortice with ankle plantarflexion Regarding peripheral jt mob resting position: slight ankle plantarflexion (10º) closed packed position: full ankle dorsiflexion Foot Positions Subtalar or talocalcaneal joint – Inversion & eversion Pronation = ankle dorsiflexion + subtalar (calcaneal) eversion + forefoot abduction (external rotation) Supination = ankle plantarflexion + subtalar (calcaneal) inversion + forefoot adduction (internal rotation) Foot Positions Transverse tarsal joints Talonavicular joint Calcaneocuboid joint – compound joint known as the transverse tarsal joint line – that transects the foot head of talus “ball” anteriorly concavity of navicular “socket” inferiorly concavities of anterior and medial calcaneal facets and by the plantar calcaneonavicular ligament; medially by deltoid ligament laterally by the bifurcate ligament (“socket”) by navicular bone anteriorly, deltoid ligament medially medial band of bifurcate lig laterally spring (plantar calcaneonavicular) lig inferiorly Role of spring ligament support for the medial longitudinal arch little or no elasticity. Keystone Arches of the Foot Medial Longitudinal Arch Lateral Longitudinal Arch Transverse Arch Medial Longitudinal Arch – – – – – – Calcaneus Talus Navicular 1-3 cuneiforms 1-3 MT’s Function Arches of the Foot Medial Longitudinal Arch continued – Ligament Support • Plantar Calcaneonavicular (spring) • Long Plantar Lig • Deltoid • Plantar fascia Arches of the Foot Medial Longitudinal Arch continued – Muscular Support • Intrinsic – Abductor Hallucis – Flexor Digitorum Brevis • Extrinsic – Tibialis Posterior – Flexor Hallucis Longus – Flexor Digitorum Longus – Tibialis Anterior Arches of the Foot Lateral Longitudinal Arch – Composed of • Calcaneus • Cuboid • 4-5th MT’s – Ligament Support • Long & Short Plantar • Plantar Fascia Arches of the Foot Lateral Longitudinal Arch continued – Muscle Support • Intrinsic – Abductor Digiti Minimi – Flexor Digitorum Brevis • Extrinisic – Peroneus Longus, Brevis & Tertius Arches of the Foot Transverse Arch – Formed By: – Ligament Support • Intermetatarsal Ligaments • Plantar Fascia – Muscle Support function Shock absorber Weight bearing Prevent blood vessels and other soft tissue from being crushed • All intrinsic muscles • Extrinisic – Tibialis Posterior – Tibialis Anterior – Peroneus Longus Medial longitudinal arch It is higher more mobile more resilient Than the lateral arch Absorbs forces of thrust & weight Medial Longitudinal Arch in Gait In normal gait medial longitudinal arch raised during heel strike , providing a rigid foot for weight transmission And during foot flat medial longitudinal arch is depressed providing a flexible support to adapt to uneven ground/surfaces Pathomechanics of Medial Longitudinal Arch Pes Cavus Pes cavus is a high arch that does not flatten with weightbearing. deformity can be located in forefoot, midfoot, or hindfoot or in a combination of these sites. Pathomechanical Causes clawing of toes posterior hindfoot deformity (described as an decreased calcaneal angle), Contracture/tightening of the plantar fascia cock-up deformity of the great toe. This can cause increased weightbearing for the metatarsal heads and associated metatarsalgia and callus formation. Pathomechanics due to Pes Cavus Foot is inverted Calcaneus is inverted/varus Big toe usually plantar flexed and other toes dorsiflexed at metatarsophalangeal joint resulting in claw foot deformity During gait the arch is not depressed even in foot flat phase resulting in loss of adaptation to uneven surfaces lateral foot pain from increased weightbearing on the lateral foot. Metatarsalgia Ankle instability can be a presenting symptom, especially in patients with hindfoot varus and weak peroneus brevis muscle. Patients with neuromuscular disease complain of weakness and fatigue Pes Planus Flatfoot may be classified as congenital or acquired. Congenital flatfoot can be further divided into rigid and flexible. Congenital rigid flatfoot is due to a structural bony abnormality such as vertical talus Congenital flexible flatfoot is mostly physiological, asymptomatic and requires no treatment Pathomechanical Causes Posterior tibial tendon dysfunction (PTTD). This tendon is vital to the maintenance of the medial arch. Attenuation or rupture of the PTTD tendon will cause a flatfoot deformity Tarsal coalition. This is a congenital condition where bones in the midfoot and hindfoot are abnormally joined together. This causes a reduced range of movement and the transfer of mechanical forces to other joints causing pain. Peroneal spastic flatfoot is a name given to flatfoot deformity with increased tone in the peroneal muscles. These muscles evert the foot and disrupt the balance of muscular pull around the ankle Pathomechanics due to Pes Planus Charcot foot. This is flatfoot, sometimes a rocker bottom foot, associated with a peripheral neuropathy. (Lax Plantar Fascia) The heel bone, when viewed from rear is everted or in valgus. Flatfeet may cause, other biomechanical causes of pain for example, genu valgum (knock knees), medial or anterior knee pain, Achilles tendonitis, and low back pain During Heel Srtrike in the gait cycle the longitudinal arch is not present , thus not able to provide a rigid foot for weight transmission Foot is everted, Forte foot is Abducted and pronated This causes the Big toe to abduct and go into a valgus position resulting in Hallux Valgus Deformity weight transmission is displaced from head of 1st metatarsal to head of 2nd and 3rd metatarsal resulting in an abnormal weight bearing Metatarsal head’s lateral surface in Big toe valgus deformity rubs against the shoe and results in callus formation Arches of the Foot Arches of the Foot Arch Positions Normal High arch: Pes cavus Low arch (flat foot): Pes planus Ankle Joint Stability Distal ends of tibia and fibula – like mortise (pinchers) of adjustable wrench Tibia is weight bearing Fibula is considered non-weight bearing – may hold up-to 10% of body weight Multiple ligaments Ligaments and Sprains Ligaments and Sprains Movements & Major Muscles Dorsiflexion: Tibialis anterior Plantar flexion: Gastrocnemius & soleus Inversion: Tibialis anterior, peroneus longus & peroneus brevis Eversion: Peroneus tertius Biomechanics of Gate Stance phase (60-65%) – – – – – Heel contact (heel strike or initial contact) Foot flat (loading response) Mid stance Heel off (terminal stance) Toe off Swing phase (35-40%) – Toe off (acceleration or initial swing) – Mid swing – Heel contact (deceleration or terminal swing) THANK YOU