Link to NCIIA Grant Proposal
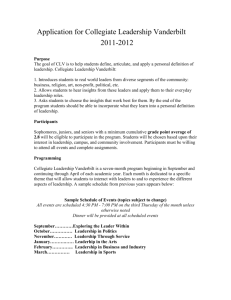
advertisement

Vanderbilt University Department of Biomedical Engineering Senior Design Project NCIIA Grant Proposal for a Pacemaker Detection Protocol for MR Suites 6 December 2012 “The Coil Kids” Zach Eagleton Josh Shannon Michael Shannon Josh Stewart Sam Walling Abstract: The radio frequency currents produced by MR scanners pose a serious risk for patients with implantable metallic objects, especially pacemakers. Many of the adverse events that result from inadvertent scans of patients with pacemakers could be avoided by proper screening protocol. In response to this need, the aim of this project is provide a protocol to reliably detect the presence of a pacemaker implanted in the patient before beginning the MR scan. The most important objectives of this project are: To develop a detection device sensitive to implanted pacemakers that can be used to screen patients prior to a scan To develop a tissue phantom to evaluate the accuracy and efficiency of this detector To create a protocol to be utilized by radiology technicians that employs the aforementioned detector and reliably ensures that no patient with a pacemaker undergoes an MR scan Introduction While artificial cardiac pacemakers have certainly enhanced the quality of life of millions of individuals, they also subject these individuals to certain adverse effects. MR scanners pose a serious risk for this population because the strong electromagnetic fields associated with the radio frequency currents produced by the scanner disrupt the pacemaker’s electric impulses and render it ineffective or detrimental to the health of the patient. According to the FDA’s Manufacturer and User Facility Device Experience (MAUDE) Database, the magnetic gradients of the scan in one case undesirably caused a pacemaker to reduce its pacing rate from 75 to 35 beats per minute and in another, the gradients caused a pacemaker to reset completely and stop pacing the patient’s heart. These adverse events are caused by the induction of current in the circuitry of the pacemaker, which alters the device’s function. Additionally, patients have been internally burned by the induction of electrical current in the pacemaker’s metallic leads. In response to these life-threatening implications, hospitals have devised individual protocols to prevent patients with pacemakers from undergoing MR scans. These safety protocols, however, are highly subject to human error. In most hospitals, including the Vanderbilt University Medical Center, screening is accomplished solely by a paper questionnaire, which relies on patients to self-report that they have an implanted pacemaker. Additionally, a small number of independent companies have developed a market in ferromagnetic detectors specifically for MR suites. However, these detectors are not sensitive enough to reliably detect pacemakers and other implantations. As is evident from the incident reports present in the MAUDE Database, in many cases, the present protocols have not prevented affected patients from being scanned. It is obvious that more stringent safety protocols are necessary to prevent these harmful events. This need to reliably detect pacemakers could be met with many distinct solutions, including a detailed pre-scan review of the patient’s medical history to crosscheck for history of a pacemaker implantation or a pre-scan physical exam of the patient’s chest to check for the presence of a pacemaker. More technologically advanced solutions could also include sensing the pacemaker’s integrated radio frequency signals, which are used for programming, or using an electrocardiogram to identify the distinct patterns of a pacemaker in the electrical potential of the heart. While each of these solutions could be used to meet the present need, we propose that the most efficacious and promising method involves the development of a metal detection system capable of detecting a pacemaker implanted inside a human body and a systematic protocol that employs this detector to ensure no patients with pacemakers are unknowingly scanned. This detector would be a handheld device that uses alternating magnetic fields to detect the presence of metal. It would be utilized by the radiology staff during the pre-scan procedure, and if a pacemaker was detected, the staff would report the finding to a radiologist for further instruction. History and Context Accidents related to MR scanners and pacemakers have been on the rise in recent years as a result of the increasing prevalence of pacemakers in the general population, but still, many incidents go unreported. According to one study, as of 2004, ten deaths had occurred as a result of adverse effects of MR scanning on patients with pacemakers (Martin et al, 2004). While there is little reliable data concerning the incidence of non-mortal consequences, much concern has been raised in the medical community. Regardless, much of this problem is due to discrepancies in hospital protocol on screening, as current laws do not require a metal detector test for patients. This leaves many patients with pacemakers unscreened before entering the machine which poses severe harm to their health. In our efforts to address this problem, we have discussed possible solutions with radiologists and biomedical engineers and as a group, have decided to focus on the device and protocols that we propose here. Attached is a sketch of the device that we currently envision. Upon completion of a prototype, we hope to form a relationship with the Vanderbilt University Medical Center to test our protocol in a clinical setting. Our Team Our team was created with the goal of taking five intelligent, but different individuals, and putting them in an environment where their strengths could be maximized. For example, Zach has had over two years of hands on experience working in a hospital. His understanding of hospital dynamics will prove vital in creating a device that will be well managed and properly used in a hospital setting. Mike’s experience with programming will provide technical support to a team in need of programming savvy engineers. Josh Shannon has great technical skill having worked in a research lab for over two years. The analytical thinking often employed in such research will help nail down specific functionalities of our device. Good communication skills will likely play a role in facilitating progress. Josh Stewart has held positions in the past where his success was dependent on his ability to communicate effectively. Lastly, Sam’s leadership has been noted on this project guiding the innovation and brainstorming process. Furthermore, he has gone through the patenting process multiple times having a greater understanding of the cost-benefit analysis examined when looking at new devices. Dr. Will Grissom is our primary advisor and with his expertise in MRI and electromagnetics, he will be able to guide us through the entire design process. While Dr. Grissom is our advisor, it will be important in the ensuing months to speak with radiologists and radiology technicians to give us further insight into the problem. Work Plan In order to attain a solution to the needs of this project within the present time constraints, it is necessary to establish an overall work plan to ensure that progress is being made at an appropriate pace. As is seen in the Gantt chart in Appendix A, the initial two months of the project will be spent on the ideation and planning stages of the project. In October and November 2012, the problem will be identified and the needs declared, which will allow us to brainstorm possible solutions. In November and early December 2012, these solutions will be narrowed down to a single design approach. With this design in mind, the appropriate parts and supplies will be ordered and procured. Once the necessary components are in place, an initial prototype will be produced by the end of January 2013, which will be modified as necessary until a final product is developed by the beginning of April 2013. Simultaneously, a tissue phantom will be produced for testing purposes under the same timeline as above. With this work plan, milestones will be reached when the ideation process brings us to a single solution (December 2012), a prototype is developed for both the detector and phantom (January 2013), and the final design of the detector is implemented (April 2013). By the end of this period, we expect to have a commercially marketable product that could be used in any radiology clinic to detect the presence of metal. Because this system approaches the problem at hand in a novel fashion, its commercial implications could allow the project to continue if MR manufacturers express interest in incorporating this technology into their scanning systems. Because of the novelty of our approach and its simplicity in implementation and use, its prospect of attaining commercial success seems very high. Evaluation and Sustainability Plan The first step in developing a device to detect the presence of a pacemaker would be to first design it so that it would be sensitive enough to detect some aspect of the pacemaker, whether it be the wires or the main body of the pacemaker. The pacemaker has to be able to be accurately detected by the device. The ability to develop a prototype that is sensitive enough to accomplish this is an optimal first measure of the initial success of the device. After this is done, the next step would be to implant a pacemaker or an object that adequately mimics a pacemaker into an anthropomorphic tissue phantom to test the ability of the device to detect a pacemaker while it is implanted. The development of a tissue phantom that sufficiently mimics the area that the pacemaker will be implanted is the next criteria for success since a well-made phantom will ensure that the device can accurately detect the pacemaker under the skin. At this point, the device may have to undergo several iterations of prototyping to reach the desired level of accuracy. The next measure of success would be when the device reaches the necessary sensitivity level to detect the pacemaker inside the phantom. After this is accomplished, the device could then be used on actual people to see how well it can detect the presence of pacemakers. When the device reaches the capability to detect pacemakers in people at sufficient accuracy, then this will be the point at which we know that we have succeeded in the design of the device. Appendix A. Works Cited Martin, Edward T., James A. Coman, Frank G. Shellock, Christopher C. Pulling, Robert Fair, and Kim Jenkins. "Magnetic Resonance Imaging and Cardiac Pacemaker Safety at 1.5Tesla." Journal of the American College of Cardiology 43.7 (2004): 1315-324. ZACHARY EAGLETON Current Address 444 Elmington Avenue Apt. 536 Nashville, TN 37205 zachary.e.eagleton@vanderbilt.edu 217-494-7097 Permanent Address 1605 Claude Drive Springfield, IL 62704 EDUCATION Vanderbilt University, School of Engineering Nashville, TN Bachelor of Engineering May 2013 Major: Biomedical Engineering GPA: 3.10/4.00 Dean’s List: Spring 2012 EXPERIENCE Vanderbilt School of Engineering Nashville, TN May, 2012 - Present Research Assistant • Contribute to development of low-resource diagnostic assay for malaria. • Apply Optimal Coherence Tomography to characterize flow profiles in colloids. • Model evaporation of water droplet using COMSOL. • Acquire lab techniques and characterization skills such as fluorescence microscopy, macro writing, and Dynamic Light Scattering. Memorial Medical Center Springfield, IL May - August, 2010-2011 Emergency Room Unit Support Assistant • Performed EKGs, collected specimens, obtained vital signs, stocked rooms, transported patients, and carried out a variety of necessary ER tasks. • Assisted nurses with patient care and completed regular rounding on rooms to ensure quality patient experience. • Communicated patient needs effectively and accurately to 20 nurses and 5 physicians in a 50 bed, level 1 trauma center. Franklin Middle School Springfield, IL August, 2010-2012 Basketball Camp Coach Led teams of 15 middle school students in exercises which taught fundamental basketball skills and teamwork. Southern Illinois University School of Medicine Springfield, IL May - August, 2008-2009 Research Assistant • Assisted with study that sought to determine correlation between REM sleep and chronic obstructive pulmonary disease in patients with sleep apnea. • Collected and analyzed data from polysomnographs and spirometry tests. VOLUNTEER SERVICE Vanderbilt Student Volunteers for Science Nashville, TN September - April, 2010-Present Team Leader • Organize a small group of volunteers to teach a weekly science lesson to students in Nashville area middle schools. PROFESSIONAL SKILLS • Proficient in MATLAB, PowerPoint, Excel, Mathematica, ImageJ, ImagePro, and COMSOL. Joshua Shannon Current Address: Vanderbilt University, PMB 343924 Nashville, TN 37235 joshua.m.shannon@vanderbilt.edu (352)410-1741 Permanent Address: 5092 Mentmore Ave. Spring Hill, FL 34606 Education Vanderbilt University, Nashville, TN Major: Bachelor of Engineering in Biomedical Engineering May 2013 Current GPA: 3.4/4.0 Honors/Activities - Dean’s List - Alpha Lamba Delta Honor Society, Phi Eta Sigma Honor Society, National Society of Collegiate Scholars, Biomedical Engineering Society, Lotus Eaters Research - Vanderbilt University, Advanced Therapeutics Laboratory Use RAFT polymerization to synthesize stimuli sensitive polymers for intracellular delivery of biomacromolecular drugs. Apply several methods to purify polymers including precipitation, dialyzing, and lyophilization Characterize polymers using GPC, TEM, DLS and by analyzing GPC and NMR graphs Applied cell culture techniques to grow fibroblast and stem cells Presented and discussed selected research journals and collaborated across engineering disciplines - Dr. Pintauro’s Lab: The Development of New Proton Exchange Membranes for Fuel Cells Characterized polymers using a Differential Scanning Calorimeter machine and x-ray diffraction Learned the processes of annealing and testing the solubility of polymer membranes - Nelson CE, Gupta MK, Adolph EJ, Shannon JM, Guelcher SA, Duvall CL. Sustained local delivery of siRNA from an injectable scaffold. Biomaterials, 33 (2012), pp. 1154-1161 - "Biodegradable Tissue Scaffolds for Cell and siRNA Delivery" BMES Conference poster presentation, Hartford, Connecticut, October 2011. - Vanderbilt University, Vanderbilt Students Volunteering for Science Leader Lead a team of five undergraduates in weekly visits to local middle schools to promote an early interest in science careers through an expanded curriculum and unique learning experiences Create age appropriate experiments to teach hands-on learning and science fundamentals - Vanderbilt University, V-Squared Mentor Publications Leadership - Vanderbilt University, Biomedical Engineering Society Community Service Committee - Mentor five first year undergraduate engineers Help acclimate mentees to university life, aid in coursework selection, and provide other guidance Organize and manage several engineering related community service events involving 20-30 volunteers Research, make initial contacts, and coordinate volunteer events with non-profit organizations BMEpulse Journalist Write several articles for the BMEpulse, an engineering newsletter read by hundreds of undergraduates, professors, and alumni Made contacts, performed interviews, and summarized seminars with professors and alumni Michael Shannon Current Address: Vanderbilt University, PMB 355011 Nashville, TN 37235 michael.j.shannon@vanderbilt.edu (352)410-1641 Permanent Address: 5092 Mentmore Ave. Spring Hill, FL 34606 Education Vanderbilt University, Nashville, TN Major: Bachelor of Engineering in Biomedical Engineering May 2013 Current GPA: 3.55/4.00 Honors/Activities - Dean’s List - Alpha Lamba Delta Honor Society, Phi Eta Sigma Honor Society, National Society of Collegiate Scholars, Biomedical Engineering Society, Lotus Eaters Honor Society Research - Vanderbilt University, Biomedical Modeling Laboratory Use a biomechanical model to work towards image guidance for breast surgery Acquire data from tissue phantom using such equipment as a laser range scanner (LRS) and a CT scanner Become familiarized with the basics of an image guidance system Use Matlab to analyze data gathered from LRS, CT scan, and a volume mesh to generate a model with boundary conditions that can be used to predict deformation Use a finite element model to simulate a retraction on a tissue phantom Received SPIE Honorable Mention Award for poster presented on research First author on paper published in SPIE Conference proceedings - Vanderbilt University, Baudenbacher Lab: Design of a Nano-Liter Bioreactor for the Detection of Norepinephrine Service - Vanderbilt University, Global Medical Brigades - - Work in a resource poor setting to provide medical relief for impoverished families Shadow local doctors and help provide medications to patients Overcame language barriers to educate patients and children on personal hygiene Vanderbilt University, Engineering World Health Skills Develop a microelectrode and a master of a nano-liter bioreactor on a silicon wafer using standard photolithography devices and techniques Work in ISO5 clean rooms for photolithography and microfabrication of devices Perform cyclic voltammetry measurements of norepinephrine concentrations using an iridium oxide microelectrode Trained student on proper protocol for working in clean room and performing appropriate photolithography techniques for the design of a nano-liter bioreactor Build and test electrosurgery unit (ESU) testers to give to developing country hospitals and to ensure the functionality of these devices Part of design team to develop a cost effective and reliable infant respiratory monitor to be used in resource-poor hospitals Programming Languages: Matlab (2 years including 1 year of in lab experience), C++, Java Joshua Stewart Home Address: 9 Revolutionary Road Acton, MA 01720 joshua.m.stewart@vanderbilt.edu c: 978-844-4038 School Address: 411 Village at Vanderbilt Nashville, TN 37212 Education Vanderbilt University, Nashville, TN Bachelor of Engineering, Biomedical Engineering Minor: Mathematics GPA: 3.0 Spring 2013 Colby College, Waterville, Maine 2009-2010 Relevant Courses Tissue Engineering, Analysis of Biomedical Data, Computer Programming, Biomechanics, Biomedical Materials, Linear Algebra and Differential Equations, Circuits, Biomedical Instrumentation, Statistics and Probability, Vector Calculus, Systems Physiology, Physical Transport Phenomena Relevant Work Experience Sung Laboratory, Vanderbilt University Research Assistant (Winter 2012-Present) Synthesis and characterization of a vascular patch programmed for shape memory function and reactive oxygen species (ROS) degradation Allen Medical Systems - subsidiary of Hill-Rom, Acton, MA Intern (Summer 2011) Helped design a modern “Jackson” spinal table for surgery Volunteer Experience Alternative Spring Break, Talladega, AL (Spring 2012) James Eldridge, Democrat for Massachusetts State Senate Seat, Acton, MA (Summer 2008) Relief Missions, Compassion for Hope, Jamaica, Gulfport, MS (Summers 2007-2009) Campus Involvement Vice President, Vanderbilt Health and Fitness Club (2011-present) Team Leader, Vanderbilt Student Volunteers for Science (2011-present) Member, Vanderbilt Biomedical Engineering Society (2010-present) Teammate, Colby College Water polo Team (2009-2010) Proficiencies/Skills MATLAB, Mathematica, STATA, Logger Pro, Sage, some Solidworks, Microsoft Office products: Excel, Power Point, and Word Professional Membership Biomedical Engineering Society – Student member SAMUEL CLINTON WALLING Current Address: PMB #355714 2301 Vanderbilt Place Nashville, TN 37235-5714 502.424.0703 (C) 502.897.3040 (H) samuel.c.walling@vanderbilt.edu EDUCATION Vanderbilt University, School of Engineering, Nashville, TN Bachelor of Biomedical Engineering, May 2013 Saint Xavier High School, Louisville, KY High School Diploma, May 2009 GPA: 4.00/4.00 (unweighted) 5.09/4.00 (weighted) Honors: National Merit Scholar, Outstanding Leadership Award, Outstanding Scholarship Award, 2009 Father John Morgan Scholarship, 2009 Benn Family Fund Youth Volunteer Scholarship RELATED EXPERIENCE Vanderbilt Sports Medicine, August 2009 – Present Clinical Intern • Provide medical coverage for Vanderbilt University’s football team’s practices and competitions with a team of certified athletic trainers and physicians accumulating over 2,000 hours of experience • Create and implement individualized rehabilitation programs to treat athletes’ specific injuries and conditions under the supervision of staff clinicians • Observe and assist team physicians in their evaluation and treatment (including surgery) of injuries in order to broaden my understanding of sports medicine and the healthcare industry • Administer therapeutic modalities including electric stimulation, ultrasound, iontophoresis, hydrotherapy, etc. • Maintain medical records and ensure that required insurance, consent, and screening information is obtained SCR Development Group, May 2011 – Present Director, Sports Science Applications • Collaborate with a team of biomedical engineers and physicians to develop novel cryotherapy technologies for athletic muscular recovery • Lead initial design efforts and prototyping of new configurations and improvements on current products • Communicate with collaborative engineers and customers to improve the quality of our product • Awarded United States Patent for “Athletic Cooling and Heating Systems, Devices, and Methods” COMMUNITY INVOLVEMENT Volunteers of America (Kentucky), May 2008 – May 2009 Founder and Director of Service Initiative • Implemented a project involving over 100 volunteers that provided childcare and educational opportunities for impoverished children