Assignment 2 – Modifiers
advertisement

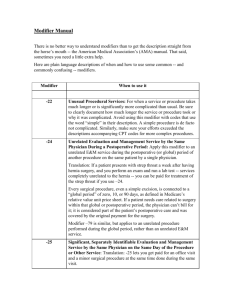
Assignment 2 – Modifiers 1. Find Definition of each modifier 2. Describe how each modifier is to be used(explain situation) 3. Write each answer in paragraph form 22: This modifier is for increased procedural services. It is for when the services provided by a physician is substantially greater than typically required. Modifier 22 tends to be used when a procedure takes an “unusual” amount of time or effort to perform. 23: Modifier 23 is when there is an unusual case of anesthesia needed. Usually this occurs when a normal procedure that either needs no anesthesia or just local anesthesia turns into needed something more. So, if you went for a normal clean at the dentist’s office and you are in so much pain he must use anesthesia to make the procedure easier, this would be a case you could use this modifier 24: This modifier is for unrelated evaluation and management service with the same physician during a postoperative period. This can be used to indicate the service was exclusively for treatment of the underlying condition and not for post-operative care. Also this can be used when the same physician provides unrelated critical care during the post-operative period. For example, if you have a surgery done, but get the flu later after the surgery is done, this would be a time you could use this code. 25: This modifier is used for a significant, separately identifiable E/M service by the same physician on the same day of the procedure or other service. There are many special circumstances that this comes in to play. This could possibly be used if you have had a surgery and the doctor wants to evaluate you after this surgery is complete. 26: Modifier 26 is a professional component that refers to certain procedures that are a combination of a physician component and a technical component. Using modifier 26 will identify the physician’s component. I believe that this could be used during a normal doctor visit when you also have to have lab work done. 32: Modifier 32 indicates mandated services. Providers are only supposed to use this modifier when reporting a service mandated by an outside entity, such as an insurance company. So, I believe this code could be used if the insurance company demands a full evaluation on a patient before a certain procedure is done. 47: This is used when a regional or general anesthesia provided by the attending or assistant surgeon. This would be used when an anesthesiologist cannot be presented so the attending or assistant surgeon would have to perform this duty. Of course the attending or assisting surgeon would have to be certified to be able to administer the regional or general anesthesia. 50: Modifier 50 is used when a procedure is done bilaterally. Bilaterally means that this procedure is done on both sides. For example, there could be a procedure where some had both legs amputated and this could be where a 50 modifier is used. 51: This modifier can be used when multiple surgeries performed on the same day, during the same surgical session. Also this can be used when diagnostic imaging services subject to the multiple procedure reduction that are provided on the same day, during the same session by the same provider. This could be used when you go in for a regular doctor’s visit and you get x-rays done and a pap-smear and blood tests done all at once. 52: This modifier is used for a reduced service. This is reported as a reduced or eliminated service or procedure. If a doctor plans on during a full blood panel, but instead only does the necessary this modifier could possibly be used because it is not a full service. 53: This modifier indicates that the physician elected to terminate a surgical or diagnostic procedure due to the patient’s well-being. When there is something that is threatening the well-being of the patient, the physician may make the decision to discontinue a procedure (even if it has been started). This could possibly be used in a surgery when the risk becomes too high to continue on with the rest of the operation. 54: Modifier 54 indicates that the surgeon is billing for the surgical care only. This could be used when a doctor is working with a surgeon on the same patient. The surgeon may have only been involved in the surgery part. So, when the surgeon puts in the bill for his work he would use this modifier to bill for just the surgery alone. 55: This modifier is used to indicate a physician, other than the surgeon, is billing for part of the outpatient postoperative care. This can also be used by the surgeon when he/she is providing only a portion of the post discharge post-operative care. This could be used, when after a surgery, the patient returns to the doctor for a check up on how things are healing. 56: Modifier 56 is used when on physician performs the preoperative care and evaluation while another physician performs the actual surgery. I feel that is occurs more often that I truly realize. Some patients will have their normal physician, or specialist, do a preoperative evaluation and then have a completely different doctor to perform their surgery. 57: This modifier indicates an E/M service resulted in the initial decision to perform surgery either the day before a major surgery or the day of a major surgery. This to me is just a reevaluation that this surgery is the right thing to do for the patient. The E/M service could be the big determining factor on whether or not they even go through with the surgery because something could have come up to make this surgery dangerous for the patient. 58: Modifier 58 indicates a staged/related procedure/service by the same physician during the postoperative period. This modifier could be used if someone has had a diagnostic procedure. After this procedure the patient would have to return to the same doctor to review the results and see if there is any further action needed. 59: This modifier identifies procedures/services not normally reported together, but appropriately billable under the circumstances. This is used when there is NO other appropriate modifier available. This could possibly be used when a patient comes in to the office for x-rays and figures while they are there could get their flu shot. 62: This can be used when there are two surgeons (each of a different specialty) are required to perform a specific procedure. I believe that this is done very often because most surgeries include anesthesia. Therefore you must always have an anesthesiologist as well as a general surgeon or a specialist. 63: Modifier 63 is used when a procedure is performed on an infant less than 4kg (or 8.8 pounds). This is another modifier that could be used quite often especially on premature babies. Most premature babies have heart and lung issues. This would require a lot of attention and sometimes even surgery and because it is more difficult than a normal person they would use this modifier to affect how much the procedure would cost. 66: When a team of surgeons (more than two surgeons of different specialties) are required to perform a specific procedure, each surgeon bills for the procedure with a modifier “66”. I assume that this would be used if the surgeons do not get paid through the same bills. So, if two surgeons had to work on the same patient even for different reasons (possibly one had to work on the heart while the other had to work on the lungs) they would use this modifier to indicate they were not the only one on this procedure and they would not be the only ones billing for this procedure. 76: This is used for a repeated procedure by the same physician. Modifier 76 is used to report repeated procedures on the same day, i.e. radiology services. This could be needed if a child broke their arm and got it casted the same day they would need x-rays before the casting as well as after to make sure the break was put back into a proper state. 77: Modifier 77 is used for a repeated procedure or service that is done by another physician or other qualified health care professional. This seems to be used when a patient is looking for a second opinion. If a patient gets evaluated by one doctor and that doctor believes they need to have surgery and the patient does not want surgery, they could potentially go to another doctor for the same evaluation. 78: This modifier is used when there is an unplanned return to the operating room by the same physician following an initial procedure for a related procedure during the postoperative period. Modifier 78 sounds like it would be used if there was a complication after a procedure. So, if there was internal bleeding that was not stopped properly during surgery then they would have an unexpected return to the operating room to help save the patient. Because they cannot bill for the same procedure they would use this modifier to explain why they had to return to the operating room. 79: Modifier 79 is used when an unrelated procedure done by the same physician during the postoperative period is performed. I believe that this could be used when a patient could have symptoms of another illness after a procedure occurred. 80: When there is an assistant surgeon in a surgery they must be identified by adding the modifier 80 to the usual procedure number(s). This could be during almost any surgery. I believe this would most likely occur during a major surgery such as heart surgery. 81: This is used when a surgeon only needs an assistant for a short period of time. The assistant surgeon only gives a minimal amount of service that they can bill for. This could be possibly if the surgeon needed a short break during a long procedure and had the assistant jump in for a short period of time. 82: This is used when the qualified resident surgeon is unavailable and an assistant surgeon must step in. Modifier 82 is one I don’t believe is used very often. My understanding was that there was always supposed to be a resident surgeon on staff available. Although in a situation where the surgeon had a dire emergency with either their health or with family that they could not make it would be a good reason why the assistant surgeon would have to step in. 90: Modifier 90 is used when laboratory procedures are performed by a party other than the treating or reporting physician. I can only imagine that this is used almost all the time. The physician will request certain testing to be done and it is sent off to a different lab to have the tests run. For example, blood tests could be a major one that a doctor would be sending out often. 91: This modifier is used to identify repeated clinical diagnostic laboratory tests. It helps to identify a subsequent medically necessary laboratory test on the same day of the same previous laboratory test. The only time I believe this could be used is if there were a mistake with the tests or that some was contaminated. For example, urine tests must be completed within 2 hours of collection and after would not be able to be tested accurately. 99: Modifier 99 is used to identify when there are multiple modifiers required on one line of service. 22 and 63 I believe are two modifiers that could be used together. 63 is used for procedures done on babies less than 4kg and 22 is for an unusual amount of time on a procedure so these could be used together from my understand. Of course, unless it is otherwise stated in the laws.