Fundus photo showing ROP Fundus photo showing large ridge and
advertisement
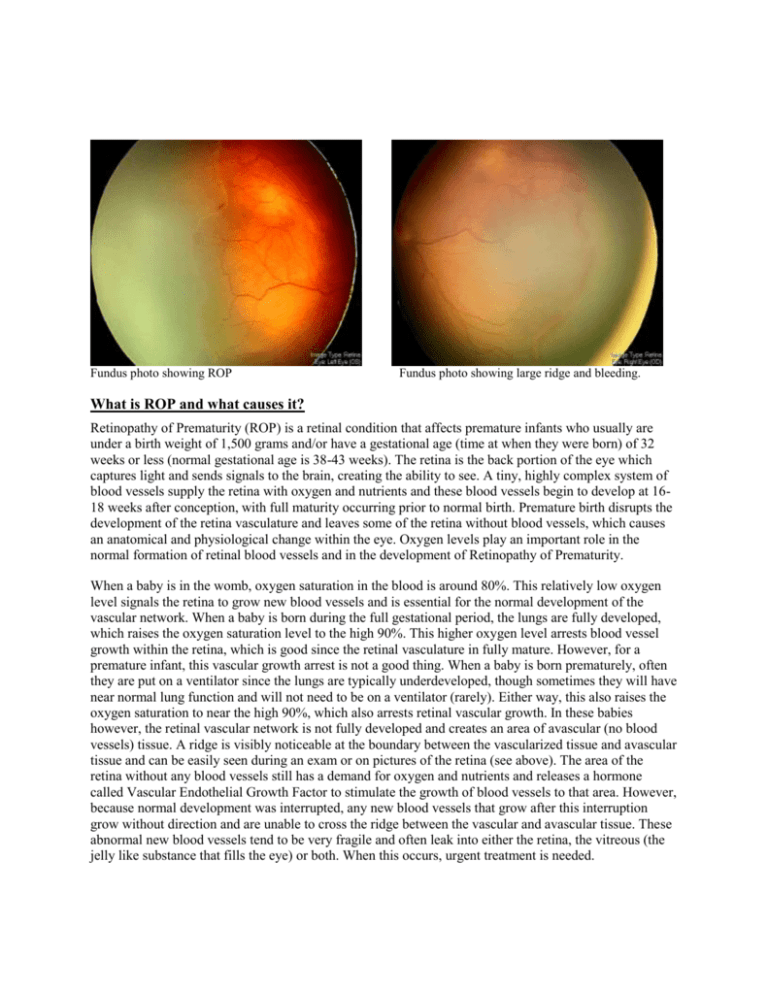
Fundus photo showing ROP Fundus photo showing large ridge and bleeding. What is ROP and what causes it? Retinopathy of Prematurity (ROP) is a retinal condition that affects premature infants who usually are under a birth weight of 1,500 grams and/or have a gestational age (time at when they were born) of 32 weeks or less (normal gestational age is 38-43 weeks). The retina is the back portion of the eye which captures light and sends signals to the brain, creating the ability to see. A tiny, highly complex system of blood vessels supply the retina with oxygen and nutrients and these blood vessels begin to develop at 1618 weeks after conception, with full maturity occurring prior to normal birth. Premature birth disrupts the development of the retina vasculature and leaves some of the retina without blood vessels, which causes an anatomical and physiological change within the eye. Oxygen levels play an important role in the normal formation of retinal blood vessels and in the development of Retinopathy of Prematurity. When a baby is in the womb, oxygen saturation in the blood is around 80%. This relatively low oxygen level signals the retina to grow new blood vessels and is essential for the normal development of the vascular network. When a baby is born during the full gestational period, the lungs are fully developed, which raises the oxygen saturation level to the high 90%. This higher oxygen level arrests blood vessel growth within the retina, which is good since the retinal vasculature in fully mature. However, for a premature infant, this vascular growth arrest is not a good thing. When a baby is born prematurely, often they are put on a ventilator since the lungs are typically underdeveloped, though sometimes they will have near normal lung function and will not need to be on a ventilator (rarely). Either way, this also raises the oxygen saturation to near the high 90%, which also arrests retinal vascular growth. In these babies however, the retinal vascular network is not fully developed and creates an area of avascular (no blood vessels) tissue. A ridge is visibly noticeable at the boundary between the vascularized tissue and avascular tissue and can be easily seen during an exam or on pictures of the retina (see above). The area of the retina without any blood vessels still has a demand for oxygen and nutrients and releases a hormone called Vascular Endothelial Growth Factor to stimulate the growth of blood vessels to that area. However, because normal development was interrupted, any new blood vessels that grow after this interruption grow without direction and are unable to cross the ridge between the vascular and avascular tissue. These abnormal new blood vessels tend to be very fragile and often leak into either the retina, the vitreous (the jelly like substance that fills the eye) or both. When this occurs, urgent treatment is needed. How common is ROP and who should be screened? Since ROP only affects premature infants, it is a fairly uncommon disease within the population of the United States. However, of all the infants born prematurely, around 17% of them will develop ROP to some extent. It is important to note that the lower the birth weight and/or gestational age, the higher the risk of ROP forming. According to statistics from 2009 released by the National Eye Institute, around 16,000 premature infants develop ROP each year. Within the United States, ROP is the second leading cause of blindness in infants, with 600 becoming blind each year. It is the standard of care to screen all premature infants who: 1. Are less than or equal to 1,500 grams, and/or 2. Have a gestational age of less than or equal to 32 weeks, and/or 3. Have had an unstable clinical course. What are the risk factors for the development of ROP? The two biggest risk factors for the development of ROP are birth weight and gestational age. Though over-all around 17% of premature infants develop ROP, around 70% of infants weighing under 750 grams and 67% of infants with a gestational age of 26 weeks develop ROP. The graphs below show the relation between these two risk factors and the development of ROP. Other risk factors for ROP include intraventricular hemorrhage, respiratory distress syndrome, bronchopulmonary dysplasia, or patent ductus arteriosus. Graph showing association between birth weight and incidence of ROP Graph showing association between gestational age and incidence of ROP How is ROP diagnosed? The doctor will perform a dilated exam with an indirect ophthalmoscope to determine the stage and what part of the retina is affected by ROP. To minimize discomfort, several numbing drops will be placed in the eye immediately before the exam. If there are any suspicious looking vessels or leakage within the retina, the doctor will perform a Fluorescein Angiogram to determine the extent of the ROP. Fluorescein Angiography is a test that documents blood circulation in the retina using fluorescein dye which luminesces under blue light. Fluorescein is injected into a vein using an IV line and digital fundus pictures are taken afterwards for around 5 minutes. These pictures show the exact location and extent of leakage and if there are any abnormal blood vessels present. The doctor will explain these pictures to you in more detail. Fluorescein angiography showing abnormal blood vessels Fluorescein angiography showing leakage at ridge How is ROP classified? ROP is classified along three catagories: zone, stage, and presence of plus disease. Zone: Stage: Refers to the clinical appearance at the vascular/avascular junction. There are 5 stages: • Stage 1: A small demarcation line is present indicating the vascular/avascular junction. No new, abnormal blood vessels are present. • Stage 2: A definite ridge is present. New, abnormal blood vessels may either be present or absent. • Stage 3: New, abnormal blood vessels are growing from the ridge into the vitreous. Intraretinal and/or vitreous bleeding is frequently present • Stage 4: The presence of partial retinal detachment. • Stage 4a- A partial retinal detachment is present which does not involve the macula. • Stage 4b- A partial retinal detachment is present which does involve the macula. • Stage 5- The presence of total retinal detachment. • Stage 5 open- retina is not adherent to itself. • Stage 5 closed- retina is adherent to itself. Stage 1 ROP Stage 2 ROP with visible ridge Plus disease: Plus disease describes the presence of venous dilation and arteriolar tortuosity within the retina. Plus disease can occur at any stage and usually indicates that the ROP is increasing in severity. The presence of plus disease is usually associated with generally poorer outcomes. Fundus photo showing plus disease (white arrow) Fundus photo showing large amounts of plus disease How is ROP treated? The best treatment is prevention. A growing body of evidence is showing that in low gestational aged infants, the use of low oxygen levels (82-92%) during the first several weeks after birth decreases the risk of ROP. The cut-off for what gestational age low oxygen levels should be used is still being debated, however around 32 weeks seems to the most accepted age as of now. Some studies have reported that increasing the oxygen saturation after the first several weeks also helps reduce the risk of ROP, though these studies are less conclusive. The use of low oxygen saturation early after birth and higher oxygen saturation later, and when exactly they should be used requires more study. If ROP progresses to the point of requiring treatment, several options are available. 1. Laser therapy using Pan-Retinal Photocoagulation (PRP) is the standard treatment for ROP and multiple studies have shown laser to be a very effective treatment for preventing the progression of ROP. The laser is used to destroy the avascular retinal tissue, stopping it from releasing Vascular Endothelial Growth Factor (VEGF-the hormone responsible for growing new blood vessels). However, if a large amount of VEGF is already present in the eye, or if there is a large amount of avascular retina, laser may not be completely effective. 2. Intravitreal injection of Avastin is used in patients who are non-responsive to laser treatment alone. Avastin is a medication that irreversibly binds with Vascular Endothelial Growth Factor (VEGF), preventing it from signaling the growth of new blood vessels. Studies have shown it to be very effective, however since the cells that produce VEGF are not destroyed with this treatment, VEGF is continuously produced by the eye. More than one injections may be necessary to reduce the amount of VEGF in the eye to normal levels. 3. Pars Plana Vitrectomy is used to remove the vitreous from the eye, completely eliminating all the VEGF in the eye. Vitreous hemorrhage and fibrovascular membranes pulling on the retina causing a tractional retinal detachment are also removed during the surgery. Pars Plana Vitrectomy is the only treatment for infants with stage 4 or stage 5 (retinal detachment is present) ROP. Fundus photo showing PRP spots (top of picture) Intravitreal injection of Avastin