Med Surg Neuro Study Stack
advertisement

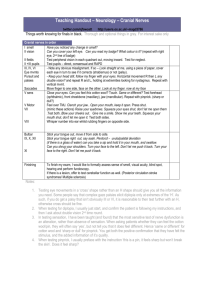
MedSurg NCTC Neuro Question Two divisions of the nervous systerm Answer Central (CNS) Peripheral (PNS) Sensory Neurons Transmit impulses to the CNS Motor Neurons Transmit impulses from the CNS Three parts of the Brain Cerebrum cerebebellum brain stem Cranial Nerve I Olfactory nerve: sense of smell Cranial Nerve II Optic nerve: sight Cranial Nerve III Oculomotor nerve: Contraction of iris and eye muscles Cranial Nerve IV Trochlear nerve: eye movement Cranial Nerve V Trigeminal nerve: sensory nerve to face, chewing Cranial Nerve VI Abducens nerve: eye movement Cranial Nerve VII Facial nerve: facial expression, taste, secretions of salivary and lacrimal glands Cranial Nerve VIII Vestibulocochlear (or auditory) nerve: hearing, balance Cranial Nerve IX Glossopharyngeal nerve: taste, sensory fibers of the pharynx and tongue, swallowing, secretions of parotid gland Cranial Nerve X Vagus nerve: Motor fibers to glands producing digestive enzymes, heart rate, muscles of speech, gastrointestinal motility, respiration, swallowing, coughing, vomiting reflex. Cranial Nerve XI Accessory (or spinal accessory) nerve: head and shoulder movement. Cranial Nerve XII Hypoglossal nerve: movement of the tongue Cranial Contents: 84% brain, blood 4% CSF 12% Decorticate posturing one or both arms are fully flexed on the chest Decerebrate posturing one or both arms are stiffly extended. Conscious the client responds immediately, fully, and appropriately to visual, auditory, and other stimulation. Somnolent or lethargic The client is drowsy or sleepy at inappropriate times but can be aroused, only to fall asleep again. Response to questions are delayed or inappropriate. Speech in incoherent. The client responds slowly to verbal commands, responds to painful stimuli Stuporous The client is aroused only by vigorous and continuous stimulation usually by manipulation or strong auditiory or visual stimuli...one or two word answers, or motor activity or purposeful behavior directed toward avoiding further stimulation. Semicomatose The client is unresponsive except to superficial, relatively mild painful stimuli to which the client makes some purposeful motor response to evade stimulation. Comatose The client responds only to very painful stimuli by fragmentary , delayed reflex withdrawl; in deeper stages, he or she loses all responsiveness. There is no spontaneous movement and the respiratory rate is irregular. Glasgow Coma Scale a tool for assessing a client's response to stimuli. A score of 10 or less indicates a need for emergency attention. A score of 7 is generally interpreted as coma. 3 categories eye opening, verbal response, and motor response gives points from 1-4 C.T Scan - Computer Tomography uses x-rays and computer analysis to produce three dimensional views of thin cross sections of the body * if using contrast requires consent MRI - Magnetic Resonance Imaging Is based on the magnetic behavior of protons in body tissues. it uses radio frequency waves to produce images of tissues of hight fat and water content such a soft tissue, veins, arteries and the brain and spinal cord no radiation. Positron Emission Tomography uses radioactive substances to examine metabolic activity of body structures. Single Photon Emission Computed Tomography Lumbar Pucture provides information about the brain's function, cerebral blood flow and status of receptors for neurotransmitters. Early identification on lesions Examination of CSF for pressure, pathogenic microorganisms and blood cells Contrast Studies -cerebral angiography - detects distortion of cerebral angiography Electroencephalogram records the electrical impulses generated by the brain. Increased Intracranial pressure Brain 84% Blood 4% CSF 12% Foramen magnum - the opening in the lower part of the skull through which the upper part of the spinal cord connects with the brain. The only hole in the brain. ...too much pressure the brain with herniate ....DRT dead right there. IICP - signs and symptoms Decreasing LOC Confusion, restlessness Headache - especially one that is more severe in the morning, increases with activities that elevate ICP such as coughing sneezing or straining at stool. vomiting with no nausea Cushings Triad pulse rises then falls widening pulse pressure irregular respiratory rate Cheyne-Stokes respirations - shallow rapid breathing followed by periods of apnea. head injury compresses the brain - big changes quickly the pop off valve is the foramen magnum (big hole at the bottom of the skull) Brain stem - heart rate, respirations, LOC - no going back ○ Glasgow Coma scale § 3-15 § 7 is comatose □ Eye opening □ Speak □ Move independently □ response to pain Vomiting especially without nausea is a neurological issue Papilledema § optic nerve swollen □ vision change □ pupil response □ fixed and dilated □ unequal pupils □ check for prosthetic eyes if no pupillary response * Tests that determine underlying cause of IICP: ○ CT scan 10-15 min ○ MRI ○ Lumbar puncture ○ Intracranial pressure monitor ○ Do a good assessment -can tell how they are doing by a good neuro assessment * Meningitis: ○ headache --light sensitive (photophobia) quiet cool dark area ○ stiff neck - nucle rigidity ○ fever ○ rash on trunk ○ mental alterations - can be wild Seizures Meningococcal: faster onset; diagnosed by spinal tap cloudy fluid make sure we do a CT before the spinal tap, antibiotics, anticonvulsants, pain, low stimulus environment. Spinal tap roll into a ball shoulder and hips inline so the vertebre make more space. Check fluid then send to the lab numbered tubes first one they disregard RBS from the tap, usually to a head ct first before the tap in case of a bleed in the brain. Cerebral Vasculitis: Inflammation of the blood vessels in the brain can result in irreversible coma, long lasting neurological problems hearing and vision. Can be fatal Encephalitis Patho & Etio many different causes usually vector borne. Most common is west nile. find source; mosquito control. Gillian Barre Syndrome Patho & Etio Auto immune - commonly follows a viral infection usually a respiratory or vaccines effects the myelin sheet weakness numbness tingling effects the arms and legs. Starts at the bottom and works their Assessment: Gillian Barre Syndrome way up. Gradual onset with a slow and recovery will be the reverse. Can take up to a year depending on the severity of the problem. Brain Abscess Patho & Etio: Infections; caused sinus, teeth ear, surgery, tongue piercing, Assessment: Brain Abscess headaches, vomiting, fever, seizures, LOC, difficulty walking, pt may be compensating for some time if the abscess is severe. Medical Mgmt: Brain Abscess Antibiotics, surgery, may need life support * Nursing Mgmt: measure I &O, LOC, Monitor for intracranial pressure, Multiple Sclerosis Patho & Etio: Destruction of the myelin sheath chronic and progressive with exacerbations and remissions but keep getting worse. Onset 20 to 40 years affects men and women approximately equally in more northern climates. * Capizole - new drug foe MS ○ flushing ○ heart palpitations ○ anxiety ○ dyspnea ○ raised burning welt possible ○ lasts 15 min or less * Nursing Mgmt: MS Keep immune system up, supportive care for pt and family, many different drugs for symptoms, no cure but meds to help with lessening exacerbations. Myasthenia Gravis Patho & Etio: thymus gland issues - drooping of eyelids, difficulty chewing and swallowing, different muscle groups effected. May see improvement with rest *Myasthenia Gravis Medical & Surgical Mgmt: diagnostic Tensilon will see improvement for 5 min. * Nursing Mgmt: Monitor respiratory, allow for periods of rest, Amyotrophic Lateral Sclerosis Lou Gerick's disease Patho & Etio: lack of muscle control degeneration of the myelin sheath, degeneration of muscle neurons and spinal cord. Potentially fatal, can be very aware that their mind is here but their body is failing. Amyotrophic Lateral Sclerosis Lou Gerick's disease** Assessment: progressive wasting of extremities, then respiratory, swallowing, speech, emotional inability to appropriately respond, watch for respiratory issues and failure. Cranial Nerve Disorders Trigeminal Neuralgia Patho & Etio: affects the 5th cranial nerve pain with chewing might be from compression from the nerve, will be reoccurring, sudden severe burning pain. can think of nothing but pain. May not be able to communicate effectively until their pain is treated. Treated with narcotics, watch for respiratory depression. may take lots of meds to get their Trigeminal Neuralgia * Medical Mgmt: pain under control but may not be able to make it go away completely. Anticonvulsants seem to help settle down the nerves some. Trigeminal Neuralgia * Surgical Mgmt: Sever the sensory route, may lose control of that side of their face, really look carefully before taking this step Trigeminal Neuralgia * Nursing Process: any little thing can set off a reaction, protect this person's face from cool breezes, fans, washing their face, eating cold things, cold drinks, any stimulation may set off this reaction. Sometimes it may resolve as quickly as it started. Bell’s Palsy Patho & Etio: 7th nerve * drooping of the face and eyelid, usually see more of the eye than a stroke ( with stroke you will see more lip ), Decreased sensation, usually not a headache, limited to the face (stroke is the whole body) Bell’s Palsy * Assessment: symptoms develop in a few hours to one or two days. Most cases recover but if still have symptoms after three months it may be permanent. eye damage, trouble swallowing, need ointment on the eye at night and tape close. Temporomandibular Disorder Patho & Etio: The meniscus of cartilaginous disk between the condyle and the temporal bone becomes displaced. Temporomandibular Disorder * Assessment: pain, headache, muscle spasm, clicking, lock jaw, chewing and talking problems, could be swallowing problems. Nutrition, cold or hot food may be irritating. Patho: affects the dopamine receptors stiffness, Extrapyramidal Disorders tremors, rigidity, hips and knees slightly flexed, Huntington's and Parkinson's disease short shuffling steps, stooped posture, arms most common Parkinson's flexed at elbows and wrists. Progressive disorder, watch for falls, pill rolling( early sign) Parkinson's Medical Management: prolong their independence for as long as possible. Rehab: maintain the highest level of function available train them and their caregivers for their needs and care. Huntington's Disease Patho - hereditary disorder, genetically passed symptoms usually show up when the pt is in their 40-50's hallucinations, emotional disturbances, impaired judgment, fast changes, speech and swallowing S/S no early symptoms - Huntington's difficulty, twisting of the body, bowel and Disease bladder control depletes, people wither down to almost nothing, contortions odd body positioning, Nursing mgnt: Huntington's Disease try to prevent complications, support them nutritionally , try to keep safe, emotional support try to maintain the highest level of functioning. Seizures - Partial won't lose consciousness, may have some uncontrolled jerking movement of a body part usually last lest than a minute. May have sensory manifestations. Generalized - Grand Mal Tonic clonic movements, whole body involved, may have sensation before called an aura. Sudden excessive jerking, may have a preictal phase vague emotional stage, after may have post ictal phase, pt very tired needs to sleep, Status Epilepticus - Series of tonic clonic seizures blood to brain, breathing, must be stopped, valium, may have to paralyze them and put on a vent, Cerebyx or dilantin to keep from seizing. Tergitol, Zarontin, Depakene, often seen if they don't take their meds Brain Tumors, - some more common in children, some more common in adults, about 50% of all tumors are malignant what causes? abnormal growth of cells, viral immunosuppression, infection, trauma, genetic, radiation, Brain Tumors Assessment headache worse in morning, vomiting without nausea, LOC, speech, paralysis, double vision, seizures, Central Nervous System * consists of the Brain and Spinal Cord * Peripheral nervous system * consists of the 12 pairs of cranial nerves & 31 pairs of spinal nerves * Brain stem * Controls awareness/alertness through reticular activating system * made up of medulla, pons & midbrain: * -* Medula anterior to cerebellum * regulates HR, resps, BP, coughing, sneezing and swallowing Pons - anterior to medulla, relays messages to upper brain centers Midbrain * extends from pons to hypothalamus * regulates movement of eyes, auditory reflexes, righting reflexes-to keep head upright * Cerebellum * posterior to medulla and pons * Coordinates involuntary aspects of voluntary movement, maintains balance, posture, spatial orientation * Cerebrum * Controls higher functions and activities, conscious mental processes, sensations, emotions, and voluntary movements Forebrain Includes the frontal, parietal, occipital, & temporal lobes & central portion of brain sympathetic division: Fight or flight * bronchodilator * increased HR and Resp * decreased gastric motility * run by neurotransmitters called catecholamines: epi & nor-epi parasympathetic division: Rest & Digest * opposite of fight or flight-dominant during nonstressful times * Bronchi-constricted or normal * decreased HR and resp, or normal * increased gastric motility * Stroke lateral side of the bottom of foot-if How do you perform a Babinski positive-great toe pulls towards nose and other reflex, also known as a plantar reflex, toes flare * normal response is for toes to curl and what does it indicate? when foot stroked * positive response indicates abnormalities * What is an EEG and what prep is necessary? * A graphic representation of electrical activity of brain cells * shampoo hair thoroughly so that electrodes will adhere to scalp * withhold seizure meds, anticonvulsants, sedatives and tranquilizers for 24-48 hours prior to EEG * restrict caffeine * assess LOC: is pt somnolent, lethargic, stuperous, semi-comatose, comatose * assess How would you do Neuro checks on a mental status: ask them to say their name, date head trauma pt? and place, include a question with a commonly known answer- * assess pupil response: * assess extremity strengt subarachnoid bleed * S/S-sudden onset, severe HA, stiff neck, decreased LOC, photophobia * What is a coup and contrecoup injury? * Coup injury is a closed head injury caused by hitting an unmoving object-the brain hits on the inside of the skull * Contrecoup injury is when an object hits the head and the brain bounces off the opposite side of the skull. What is ICP, and how important is this? * Intracranial pressure-components that exert pressure in the cranium-normal 0-15 mm Hg * anything above 15 mm Hg creates potential life threatening problems * 3 things control ICP: brain, blood & CSF The Monroe Kellie hypothesi states that in order for ICP to remain normal one must decrease if one increases. * Twisting the spinal column in the presence of Why did you take care not to twist an injury can decrease the blood supply to the mva pts back during transfer? spinal column changing the components that control ICP, this leads to increased ICP Glasgow Coma Scale what is normal? * Measures eye opening, best motor and best verbal response * each assessment receives a score * normal score: 15 * ask open ended questions What S/S occur with increased ICP? * LOC-most reliable indicator of mental status - earliest changes seen * pupillary changes are second * altered motor function * Posturing * change in temp * as pressure on hypothalamus increases body unable to control temp Biots respiration 2 shallow breaths followed by a period of apnea * What are some of the effects of spinal cord injury? * Damage can be complete or incomplete * above C4 interrupts respirations-can be fatal * C5 and below spares diaphragm so able to maintain respirations but still have respiratory compromise spinal shock reflexes below level of injury temporarily stopsextremities are flaccid-becomes spastic as shock resolves (pg. 439) loss of sensation below the level of injury increases the risk of other injuries * autonomic dysreflexia * most dangerous problem, may occur as spinal shock subsides * exaggerated response to painful or noxious stimuli, distended bladder, constipation, renal calculi, ejaculation or uterine contractions, enemas, position change * autonomic dysreflexia S/S * severe vasoconstriction leads to severe hypertension * vasodilation occurs above injury: flushing, sweating * vagus nerve stimulated causing bradycardia * Treat cause to correct Contact lenses and a head injury patient You remove them and place them in a safe container. What would you do if the pt did not have an intact corneal reflex? Lubricate eyes regularly with saline * Why would you space out the care for a spinal cord pt instead of doing his bath, PROM, oral care and dressing changes all at one time? * you want to prevent autonomic dysreflexia Decadron a corticosteroid- decreases brain swelling Dilantin decreases possibility of sezures Mannitol IV used to decrease intracranial pressure * Patient’s with neurological impairment often become easily agitated and combative. What medication can be given to help with this problem? * Haldol * Can cause extrapyramidal symptoms such as * What problems are associated with Tardive dyskinesia and Dystonia * Give Haldol? Cogentin to control this problem Kernig’s sign- flex leg at hip then extend knee * may cause pain in hamstring Brudzinski’s sign when neck flexed, hip flexion occurs What medical treatment is used for bacterial meningitis? * Antimicrobials for bacterial meningitis * anticonvulsants for seizure activity * What medical treatment is used for Viral meningitis? requires supportive care What causes Parkinson’s? * idiopathic-no known cause * What are the early s/s of Parkinson's disease? * Tremor, rigidity * bradykinesia-extremely slow movements * loss of dexterity & power in affected limbs, aching, handwriting changes, drooling, lack of facial expression, rhythmic head nodding, pill rolling * Why would physical therapy be used for Parkinson's? * To help control symptoms of disease * PT includes massage, heat, exercise and gait retraining Levodopa * crosses the blood brain barrier-converted to dopamine to supplement the levels of dopamine in the brain to improve motor movement What medication is used in * Sinemet- converts dopamine in the brain and combination with Levodopa and why? is used in combo so that lower dosages can be used to achieve therapeutic levels * hemorrhage * blood vessel ruptures causing bleeding into brain leading to increased What are the 2 major causes of CVA? intracranial pressure * ischemia * embolic & thrombotic strokes-obstructs blood flow to brain cells and they become ischemic and die * What part of the brain are often affected by CVA? * cerebrum * right hemisphere controls left side * left hemisphere controls right side * brain stem * controls vital functions-resp, HR, LOC What s/s might a person with CVA experience? * Depends on type, location, and extent of injury * Hemorrhagic * Sudden onset * Severe HAdescribed as the “worst HA of my life” * Photophobia * Stiff neck * Loss of consciousness * Vomiting * Seizures * Embolic CVA S/S * Depends on the area of the brain that becomes ischemic * Unilateral numbness, weakness or paralysis * Visual problems * Confusion or memory loss * HA * Dysphagia * Memory loss * Thrombotic S/S same, but more gradual What is affected by left brain damage? * Right sided paralysis * Aphasia * Slow cautious behavior * Memory deficits * Reasoning * Logic * Ability to analyze What is affected by right brain damage? * Left sided paralysis * Spatial-perceptual deficits * Quick impulsive behavior * Memory deficits * Emotions * Loss of creativity * Imagination What is a TIA? * Transient Ischemic Attack * Temporary blockage of a cerebral vessel * 85% blockage causes symptoms of a TIA * TIA’s are warning signs of an impending stroke What tests are done to determine if * CT scan * MRI * Cardiac ultrasound * Cerebral the CVA is caused by a clot or bleed? and carotid angiogram * EKG * PET scan clot busters * Streptokinase * tPA * Activase “clot busters” what makes a candidate You must start this medication within three hours of the onset of symptoms. Stroke must be from a clot, no recent surgeries, no medications that contraindicate it. Mannitol for cerebral edema Corticosteroids for increased ICP reduce inflammation, suppresses immune system, monitor glucose levels. watch for GI bleeds. Nimodipine or Nimotop a CCB used to decrease cerebral spasm (for hemorrhagic stroke) Dilantin decrease the incidence of seizures makes birth control pills inactive, and causes birth defects. Heparin anticoagulation What drugs are used to prevent TIA or CVA’s? * ASA * Ticlid * Warfarin Sodium * Lovenoxmust inject in the “love handles” **using a 25 g, 5/8” needle What options are available for patients who are S/P stroke? * Physical Therapy * Occupational Therapy * Speech Therapy * Home Health * Rehab hospitals Hemianopsia loss of vision Agnosia inability to recognize objects Aphasia inability to speak, read, write, use language, or comprehend words Dysphagia difficulty swallowing Dyspraxia difficulty initiating voluntary movements Hemiplegia half of the body is paralyzed What can the nurse do to help communicate to either type of aphasia? * speak slowly & clearly * use gestures * listen attentively when pt tries to speak * use alphabet board or pictures * use simple questions that require only yes or no answers PT is going to assist your patient with * With the left hand, 6” lateral to the left foot right sided weakness. How does the **Opposite the side of weakness!! patient need to hold the cane? What is Guillain-Barre’ Syndrome? * rapid progression (1-3 weeks)-myelin sheath destroyed along peripheral nervous system * an autoimmune response to a viral infection What lab tests might be performed for lumbar puncture shows increased protein in Guillain-Barre’ Syndrome? CSF What is Myasthenia Gravis? * A chronic, progressive disease with a defect in the neuromuscular junction (causes electrical impulses to be impaired to muscle) What meds might be used for Myasthenia Gravis? * Anticholinesterase drugs-Neostigmineincreases availability of acetylcholine at the neuromuscular junction * Corticosteroids-used when anticholinesterase drugs don’t work myasthenic crisis? * Myesthenic crisis-sudden exacerbation of myasthenia symptoms-difficulty breathing and swallowing, resp arrest * precipitated by infection * cholinergic crisis- sudden extreme weakness and resp impairment precipitated by overdose of anticholinesterase drugs What is Amyotrophic Lateral Sclerosis? Lou Gehrig’s disease * rapid progression of degeneration of the anterior horn cells and corticospinal tracts of the motor neuron causing spasticity, hyperreflexia , weakness, atrophy, cramps and muscle twitching, * maintains intellectual ability * Describe Post Polio Syndrome. * Pt’s with this syndrome experience progressive muscle weakness years after having Polio * care is supportive-help pt to adapt to symptoms and maintain maximum function * Must maintain strict bed rest while feeling weak What meds are commonly used with MS? prednisone, interferon 1B, baclofen, Tegretol, Symmetrel What are the S/S of MS? * Weakness * Vision changes * Nystagmusinvoluntary eye movements * Tingling in extremities * Difficulty with coordination * Bowel/bladder dysfunction * Spasticity * Depression What can cause an exacerbation of MS? * Illnesses * flu, URI, **UTI Describe the medical treatment for MS. * Treat symptomatically * Supportive care * Solumedrol for exacerbations * Interferon 1B and 1A to prevent progression * Baclofen for spasticity What meds are used for a pt with a seizure disorder? * Dilantin * Cerebrex * Neurontin * Topamax Seizure discharge teaching * Must take meds for the rest of their life * NEVER suddenly stop taking your meds-contact physician first * When taking Phenytoin, you must have good oral hygiene What is the first step you the nurse must do to dislodge a foreign object from the ear? * Gentle flush with sterile NS May need to use mineral oil or alcohol if an insect is present * Pain that increases when auricle pulled * What S/S occurs with external otitis? Dizziness, fever, drainage * Topical ATB, ASA Treatment? or codeine for pain * Also known as “swimmer’s ear” What is otitis media and how is it treated? * Infection of the middle ear * Treated with ATB * If chronic-tubes, myrongotomy What is Meniere’s disease? * Disorder of the labyrinth, possibly caused by fluid in the inner ear What S/S does a pt with Meniere’s disease experience? * Acute attack-unilateral hearing loss, vertigo * Attacks usually become more frequent and closer together as it progresses * Tinnitus is most common c/o associated w/inner ear problems How is Menieres disease treated? * Meds for an acute attack are-atropine, Valium, antihistamines and vasodilators * Surgical txdrain fluid from the inner ear or cut the acoustic nerve that controls balance * Ototoxic ablationinstilling ATB that are toxic to the inner ear battery acid splashed in his right eye. * Flush the eye with saline continuously for 30 He is in severe pain. What is your first minutes or until the burning stops intervention? How will the doctor check for damage * With a Woods Lamp to the cornea? What is the difference between central cataracts and peripheral cataracts? * Central-good peripheral vision * Peripheralgood central vision What medical treatment may be appropriate for a cataract pt in the early stages? Late? * Early-mydriatics * Late-cataract extraction with intraocular lens implant * Mydriatics -dilation Cycloplegics paralyze muscles necessary for accomodation so eye won’t move during surgery * HOB up 45 * Lie on unaffected side * What nursing interventions post-op Antiemetics to prevent or tx N/V * Administer are necessary to keep intraocular eye drops as ordered * Instruct pt no lifting >5pressure in the operative eye normal? 10 lbs * Don’t bend forward until released by Dr. * Report severe pain immed.-usually sign of increased IOP What observations do you need to make if you witness a seizure? * Respiratory * Airway * S/S of hypoxia * Length of time seizure is lasting * What body parts are involved * LOC * Incontinence