December 04, 2012 TO: Dr. Emily Crow Journal Editorial Office BMC
advertisement

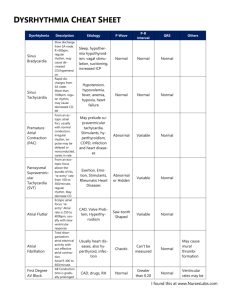
December 04, 2012 TO: Dr. Emily Crow Journal Editorial Office BMC Pediatrics Re: MS: 6692370087612996: “Persistent Wandering Pacemaker after Epinephrine Overdosing - A Case Report” Dear Dr. Crow, Thank you for considering this revision. The peer reviews are excellent and certainly improved the clarity of the manuscript. We made the requested changes as detailed below. Reviewer: Francisco J Morales-Olivas Major Compulsory Revisions 1. The authors attribute the electrocardiographic trouble to overdose of epinephrine, but do not provide arguments to explain the persistence of the effect. There is no ECG prior to the episode, therefore, the fact that the alteration already existed before the administration of epinephrine cannot be excluded. Response: This possibility is now included in the text. “There is no ECG prior to the episode; therefore, the finding may have been existed before the administration of epinephrine. Nevertheless, we speculate here that the multifocal atrial tachycardia at the episode never disappeared and lead to a wandering pacemaker instead of returning to normal. This sequela could result from a significant damage to the SA-node or atrial tissue, which persisted for at least 18 months.” 2. The authors did not include references to support causal relationship between epinephrine and ECG abnormality. Response: The new references (#2 and 6) describe multifocal atrial tachycardia and wandering pacemaker in association with sympathomimetic drug overdosing. 3. The paper should be revised to provide more information about the relationship between epinephrine and wandering pacemaker. Response: The new references 2-4 and the following paragraph are added to Text. “Sympathomimetic drugs are known to induce arrhythmias, including multifocal atrial tachycardia, re-entry tachycardia, atrial fibrillation and wandering atrial pacemaker. The mechanisms involve autonomic transmitters and changes in impulse formation, conduction and refractoriness”. 1 Minor Essential Revisions 1. The case description does not include information on the treatment administered. Response: This paragraph is now included in the text. “The patient was treated with furosemide, oxygen and fluid. He was also closely monitored.” Discretionary Revisions 1. The authors used indistinctly adrenalin and epinephrine. It would be more appropriate to use only epinephrine. Done 2. Because the symptoms are related to intravenous administration, references to "over-thecounter cold remedies" do not seem appropriate. Overdosing also occurs with inappropriate use of over-the-counter cold remedies. Therefore, we prefer to keep the sentence for this purpose. Reviewer's report: Ricardo Fernandes While description of adverse drug events is paramount to continuous monitoring of drug safety, particularly in populations such as a children, a rigorous diagnostic and causality assessment is needed, even for partially known adverse effects such as in this case. MAJOR COMPULSORY REVISIONS 1. Case presentation, 1st paragraph: The child is described as being previously healthy, yet weighing 10 kg. This weight is below the 3rd percentile of WHO weight-for-age charts. Had this failure to thrive been previously addressed or investigated? Was there any sign of underlying systemic disease? Are you aware of any later diagnosis that may be associated with the described arrythmia? Response: We are sorry. This was a “typo”; his weight was 17.5 kg and height 102.5 cm. 2. Case presentation, 2nd paragraph, first sentence: The authors describe ECG findings as both “sinus tachycardia” and “wandering pacemaker” - these are mutually exclusive. Please explain. Response: We agree. The term “sinus tachycardia” is replaced by “wandering atrial pacemaker”. 3. There is no clear separation between case presentation and discussion. Pending editor’s advice, I suggest moving the discussion to the conclusion section. Response: We agree; discussion paragraphs are moved to the conclusion section. 2 4. The authors insist in using the diagnostic term “wandering pacemaker” to describe this tachycardia. Many classifications distinguish wandering pacemaker from multifocal atrial tachycardia (MAT, often called chaotic atrial tachycardia in pediatrics) based on heart rate, the latter being used for rates >100 bpm such as here. Wandering pacemaker is therefore a better description for the later condition, and MAT should be mentioned. Response: We agree. The term “wandering atrial pacemaker” is now used. The possibility of “multifocal atrial tachycardia” is discussed in the differential diagnoses (“This could be started as multifocal atrial tachycardia and ended as wandering atrial pacemaker, as the heart rate returned to normal.”) 5. MAT has been described in association with many respiratory viruses. While the event described in this case report does suggest a causal association with adrenaline infusion, this should be mentioned as a relevant co-morbidity when considering both acute tachycardia and later findings. Response: We agree. This possibility is now discussed in Text and reference #7 is added. 6. Case presentation, 8th paragraph, “Children with marked...” The authors suggest an approach for children with inappropriate sinus tachycardia. But this wasn’t the case here! How does this relate to this case report? Is this their suggested approach for sinus tachycardia independent of doing a differential between sinus and non-sinus atrial tachycardia? Or is it for non-sinus tachycardia? If so, which references support this? Response: We agree. The approach should address sinus tachycardia vs. non-sinus (atrial) tachycardia. We show here non-sinus (atrial) tachycardia as an adverse effect of sympathomimetic overdose. This paragraph is revised as recommended. 7. The authors extrapolate from this case report to possible toxicities from OTCs. While decongestant OTC sympathomimetics’ safety profile has been a hot topic in pediatrics, this is clearly an overstatement, given this case described an IV over dosage. Response: Overdosing occurs with inappropriate use of over-the-counter cold remedies. Therefore, we prefer to keep the sentence for this purpose. 8. Figure 1: Please indicate what are the arrows pointing to? (P waves?). Further, on “Case presentation”, 2nd paragraph, QRS complexes are described as being wide (>100ms); this doesn’t seem to be the case after visual inspection of Figure 1 and considering usual ECG paper speeds - please explain or add information on this. Response: Thank you. The QRS complexes are <100ms. The arrows are pointing to the P waves. This clarification is added to the legend. 3 MINOR COMPULSORY REVISIONS 1. Background, 2nd paragraph, “Sympatomimetics;” . Done Correct both typos (needs “h” and “,”). 2. Case presentation, 1st paragraph, last sentence, “frusomide” Correct “furosemide”. Done 3. Case presentation, 1st paragraph, last sentence, Spell out BP - blood pressure. Done Respectfully, Elhadi H. Aburawi 4