Core N Objective (m)
advertisement

CORE N
(m) Describe the cellular structure of an islet of Langerhans from the pancreas and
outline the role of the pancreas as an endocrine gland.
{main textbook, p271, Fig 19.17}
PANCREAS
Large, pale-coloured gland situated in upper abdomen, behind stomach.
It is both an exocrine and endocrine gland.
Exocrine: produces digestive secretion called pancreatic juice that passes along
pancreatic duct into small intestine/duodenum. The juice contains lipase,
amylase and protease enzymes.
Endocrine: produces hormones insulin and glucagon, which are secreted
into blood capillaries.
{main textbook, p272. Fig 19.18}
in the sea of exocrine cells in the pancreas lie a small groups of endocrine cells
scattered throughout the pancreas. The small groups are known as islets of
Langerhans. There are two types of cells within each islet. They are:
(a) αcells that produce and secrete glucagon
(b) β cells that produce and secrete insulin
Both cell types are rich in secretory vesicles and are involved in detection and
regulation of blood glucose level.
Carbohydrate is transported as glucose in human blood stream. Liver and muscle
cells store carbohydrate/glucose as glycogen, a large insoluble molecule.
(n) Explain how the blood glucose concentration is regulated by negative feedback
control mechanisms, with reference to insulin and glucagon.
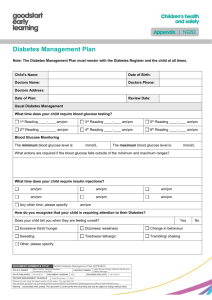
Normal healthy human: 80-120mg glucose per 100cm3 blood. Blood glucose
level fluctuates around an average of 90mg per 100cm3. The level is regulated
and is in dynamic equilibrium.
If blood glucose level is too low: there will be a lack of respiratory substrate,
therefore cells cannot make ATP for normal cellular activities. This is especially
important for cells that can only use glucose as respiratory substrate, e.g. brain
cells!
If blood glucose level is too high: water potential will be affected and this can
cause water to move out of cells, into tissue fluid and into blood. This causes cells
to shrink and cellular processes to stop.
Hence, there is a need to regulate blood glucose levels. This is done via a negative
feedback system… HOMEOSTASIS OF BLOOD GLUCOSE LEVEL.
Three sources of blood glucose:
(1) directly from diet – break down of carbohydrates such as starch, lactose,
sucrose
(2) breakdown of glycogen stores in liver and muscle cells in a process called
glycogenolysis (glycogen was made from excess glucose in the diet, in a
process called glycogenesis)
(3) gluconeogenesis – production of new glucose from other sources (other
than carbohydrate) such as glycerol and amino acids
On the other hand, low blood glucose level arises when:
(a) person is starving/fasting
(b) person undergoes vigorous exercise
When blood glucose level rises above normal…
1. β cells of the islet of Langerhans in the pancreas detect this change from
normal.
2. They respond by secreting hormone insulin directly into the blood.
3. Almost all body cells (except RBCs) have receptors for insulin embedded
in their cell surface membrane. Insulin can affect these target cells.
4. Insulin causes target cells to have increased membrane permeability to
glucose.
5. This causes increased uptake of glucose by target cells.
a. Liver and muscle cells: increased conversion rate of glucose to
glycogen
b. Adipose tissue: increased conversion rate of glucose to fats
c. Other body cells: cellular respiratory rate increases, as more
glucose available for respiration.
6. The processes in (5) return blood glucose level in blood back to normal as
excess glucose is removed from the blood.
7. β cells of the islet of Langerhans in the pancreas now detect this change
back to normal and reduce their secretion of insulin.
8. This is the negative feedback mechanism involved in restoring the normal
level of blood glucose.
When blood glucose level falls below normal…
1. αcells of the islet of Langerhans in the pancreas detect this deviation
from normal.
2. This stimulates them to produce and secrete glucagon into the blood.
3. Liver cells have receptors on their cell surface membrane that bind to
glucagon.
4. Liver cells respond by activating their phosphorylase enzyme, which
converts glycogen to glucose, as well as increases conversion of amino
acids and glycerol to glucose (gluconeogenesis).
5. Glucose is released from the liver cells into the blood.
6. This increases blood glucose level to normal.
7. This is detected again by αcells of the islet of Langerhans in the pancreas
and they reduce their secretion of glucagon.
8. This is the negative feedback system in the regulation of blood glucose
level.
When blood glucose regulation goes wrong/is not functioning… Patient suffers
from diabetes mellitus. There are two types:
(a) Type 1 diabetes mellitus / juvenile-onset diabetes / insulin-dependent
diabetes
Pancreas cannot secrete enough insulin, perhaps due to defect in
insulin gene, or due to attack on β cells by patient’s own immune
system.
Control is by diet, exercise and also regular insulin injections.
(b) Type 11 diabetes mellitus / mature-onset diabetes / non insulindependent diabetes
Pancreas secretes normal amounts of insulin but insulin receptors
may be fewer or less sensitive to the insulin than normal.
Control is by diet and exercise.
{main textbook, p275, copy and answer SAQ19.8 and SAQ 19.9}
Advantages of industrial production of human insulin by genetic engineering:
(a) more rapid response so blood glucose level brought to normal level
quickly
(b) shorter duration of response so insulin effect will wear off quickly once
normal blood glucose level restored
(c) less chance of an immune response developing towards the insulin as
exact copy of human insulin is made, while animal insulin has slight
differences
(d) effective in people who have developed tolerance for animal-derived
insulin (meaning a larger dose of animal-derived insulin is needed to
produce the same effect)
(e) more acceptable to people who feel it is unethical to use pig or cattle
insulin
(f) cheaper than extracting and purifying animal insulin