Figure 1
advertisement

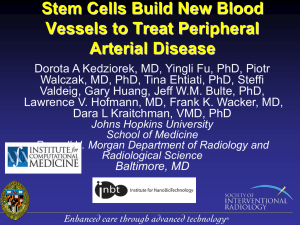
Copyright © 2012 Cognizant Communication Corporation DOI: 10.3727/096368912X655172 CT-2435 Accepted for publication PPSSCR Issue of “Cell Transplantation” Mesenchymal Stem Cell Insights: Prospects in Hematologic Transplantation Shiu-Huey Chou1, Shinn-Zong Lin2, Cecilia Hsuan Day3, Wei-Wen Kuo4, Chia-Yao Shen3, Dennis Jine-Yuan Hsieh5, Jing-Ying Lin6, Fuu-Jen Tsai7, Chang-Hai Tsai8, Chih-Yang Huang7,9,10,* 1 Department of Life Science, Fu-Jen Catholic University, Xinzhuang Dist., New Taipei City, Taiwan, 2Graduate Institute of Immunology, China Medical University, 3 Taichung, Taiwan, Department of Nursing, MeiHo University, Pingtung, Taiwan, 4 Department of Biological Science and Technology, China Medical College, Taichung, Taiwan, 5 School of Medical Technology, Chung Shan Medical University, Taichung, Taiwan, 6Department of Nursing, Central Taiwan University of Science and Technology, Taichung, Taiwan, 7Graduate Institute of Chinese Medical Science, China Medical University, Taichung, Taiwan, 8 Department of Healthcare 9 Administration, Asia University, Taichung, Taiwan. Graduate Institute of Basic Medical Science, China Medical University, Taichung, Taiwan, 10 Department of Health and Nutrition Biotechnology, Asia University, Taichung, Taiwan Running head: Mesenchymal stem cell insights *Corresponding author Chih-Yang Huang, PhD Graduate Institute of Basic Medical Science China Medical University and Hospital No.91 Hsueh-Shih Rd., Taichung, Taiwan 40402, R.O.C Tel:+886-4-22053366ext3313, Fax:+886-4-22333641 Email: cyhuang@mail.cmu.edu.tw Conflict of interest statement: The authors declare not to have any conflict of interest related to the work presented in this publication. CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation Abstract Adult stem cells have been proven to possess tremendous potential in the treatment of hematological disorders, possibly in transplantation. Mesenchymal stem cells (MSCs) are a heterogeneous group of cells in culture, with hypo-immunogenic character to avoid alloreactive T cell recognition as well as inhibition of T cell proliferation. Numerous experimental findings have shown that MSCs also possess the ability to promote engraftment of donor cells and to accelerate the speed of hematological recovery. Despite that the exact mechanism remains unclear, the therapeutic ability of MSCs on hematologic transplantation have been tested in pre-clinical trials. Based on encouraging preliminary findings, MSCs might become a potentially efficacious tool in the therapeutic options available to treat and cure hematological malignancies and non-malignant disorders. The molecular mechanisms behind the real efficacy of MSCs on promoting engraftment and accelerating hematological recovery are awaiting clarification. It is hypothesized that direct cell-to-cell contact, paracrine factors, extracellular matrix scaffold, BM homing capability, and endogenous metabolites of immunologic and non-immunologic elements are involved in the interactions between MSCs and HSCs. This review focuses on recent experimental and clinical findings related to MSCs, highlighting their roles in promoting engraftment, hematopoietic recovery, and GvHD/graft rejection prevention after HSCT, discussing the potential clinical applications of MSC-based treatment strategies in the context of hematologic transplantation. Key words: mesenchymal stem cells, hematopoietic niche, hematopoiesis, hematopoietic stem cells, bone marrow CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation INTRODUCTION Hematopoiesis is a physiological activity maintained by hematopoietic stem cells (HSCs) and hematopoietic progenitors (HPs) which possess the ability to self-renew and sustain long-term generations of all lineages of blood cells (45,50). The use of stem cells in hematologic therapeutic areas has gathered tremendous momentum over the last two to three decades. The development of hematologic malignant and nonmalignant disorders is frequently accompanied by various hematopoietic lineage failures. Therefore, hematopoietic stem cell transplantation (HSCT) has become a well established treatment for hematological malignancies and non-malignant disorders. Despite advances in human leukocyte antigen (HLA) typing, supportive care, and treatment of graft versus host disease (GvHD), the transplant related mortality and long-term morbidity from allogeneic hematopoietic stem cell transplantation (ASCT) remains significant for non-malignant diseases. The damaged microenvironment after myeloablative therapy and rejection associated with autologous recovery are two major causes for the delay in engraftment, limited number of grafts, or failure of allogeneic transplantation for many of the hematologic disorders. Therefore, ways to improve clinical outcome of autologous and allogeneic HSC transplantation have become a crucial issue in current hematologic transplantation. Currently, it is a well-accepted concept that the developmental potential of HSCs is greatly affected by stromal microenvironments, termed niches, and the development of HSCs could be reprogrammed by changing their niche. In adults, HSC and HP niches are located in the bone marrow; however, how HSCs interact with their niche cells, and the identity of the niche cells for hematopoietic maintenance, remains unclear. Numerous reports have demonstrated the role of bone marrow stromal cells (BMSCs) acting as niche cells for maintenance of hematopoietic development (14,17,72,80). In 1968, a non-hematopoietic stem cell with multiple mesoderm differentiation potential within the bone marrow (BM) was first described by Friendensten and his colleagues (16). Mesenchymal stem cells (MSCs) are a rare but unique population which have self-renewal and differentiation abilities and are able to replenish a variety of specific cell types. Evidence is emerging that MSCs can CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation escape recognition by alloreactive T cells and exert hypo-immunogenic characters (5,15,36,66). In addition, MSCs may act as the precursor cells for stromal tissues supporting hematopoiesis (25). For many years, MSCs have been considered as merely a component of marrow stroma without specific functions. Recently, it was shown that MSCs provide an enabling environment for HSC-mediated hematopoiesis, and have a crucial role in the development and differentiation of various hematopoietic lineages through cell-to-cell interactions and by producing a number of growth factors and regulatory cytokines (69,71). However, the molecular mechanism of HSC-MSC interaction has been barely unraveled and requires so further research. More recently, experimental findings and clinical trials have focused on the therapeutic ability of MSCs on cellular therapy, transplantation, and regenerative medicine. The immunomodulatory activity and engraftment-promoting properties of MSCs have been tested in a variety of animal models and human clinical trials. Based on the encouraging preliminary findings, MSCs might become a potentially efficacious tool as a therapeutic option available to treat and cure serious illnesses. This review focuses on recent experimental and clinical findings related to MSCs, highlighting their roles in promoting engraftment, hematopoietic recovery, and GvHD/graft rejection prevention after HSCT, discussing the potential clinical applications of MSC-based treatment strategies in the context of hematologic transplantation. CHARACTERISTICS OF MSCs MSCs are stromal cells that have been isolated from most species so far investigated including mice, rat, human, cat, dog, rabbit, pig, and baboons.. The sources for isolation of MSCs include adult bone marrow, adipose tissue, cord blood, umbilical cord, amniotic fluid, placenta, fetal liver, and other fetal tissues. It is well accepted that morphologic, phenotypic, and in vitro tri-differentiation potential and expansion capacity are the major criteria to be used for identification of MSCs. The physical property of MSCs is plastic adherence and its presence in low numbers in the bone marrow (1 of 104-105 mononuclear cells) (53). MSCs in culture are morphologically CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation heterogeneous, containing cells ranging from narrow spindle shaped to large polygonal and slightly cuboidal cells (16,53). Figure 1A shows the morphology of MSCs derived from mouse placenta decidua in a phase contrast image. Phenotypically, there are no specific markers for MSCs individually or in combination. It is generally accepted that human MSCs do not express markers of hematopoietic lineages such as cluster of differentiation 34 (CD34), CD45, glycophorin A, T cell, B cell, HLA-DR, CD11a, CD14, and markers of endothelial including CD11b and CD31. MSCs often express CD44, CD49e, CD62, CD73, CD90, CD105 (endoglin), CD117, CD140b, CD271, and STRO-1 (for general review see ref. (7)). It is important to emphasize that the MSC population in culture conditions is heterogeneous. Hence, morphologic or phenotypic criteria cannot be used for the unique identification of MSCs. Perhaps evaluating the function of MSCs is therefore the most useful approach for MSC identification. It is broadly accepted that the capacity for induced in vitro differentiation of MSCs to bone, fat, and cartilage is the major critical requirement to identify putative MSC populations (53). There are also generally only a few clones capable of extensive expansion. Thus, a hierarchical model is applied on MSC cultures in which multi-potency is lost following repeated passaging, with the majority of cells being transitional cells with specified lineage potential. According to data, the International Society for Cellular Therapy has provided the minimum criteria for defining multipotent human MSCs (25). The in vitro characterization morphology, characteristics, of MSCs includes colony-forming and unit-fibroblast tri-differentiation plastic adherence, (CFU-F) potential under fibroblast-like content, appropriate phenotypic inductive conditions. The expression of marker genes and surface antigens of lineage differentiation in culture does not fully represent the functionality of these cells. Furthermore, in vitro differentiation of MSCs is highly influenced by culture conditions. Hence, the physiological roles of MSCs need to be determined by in vivo assay systems. However, there is little information on the in vivo behavior of MSCs (37). Clinical studies indicated that site-directed administration of MSCs can result in successful engraftment under injury conditions, such as brain ischemia, brain injury, CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation lung fibrosis, and osteogenesis imperfect. Furthermore, the evidence indicated that the number of MSCs in engraftment areas is very small in various tissues (49,51,79). IMMUNOMODULATORY PROPERTIES OF MSCs There is an emerging amount of data to suggest that autologous or allogeneic MSCs possess broad immunomodulatory properties that make MSCs influence the activities of all cells involved in the immune responses. This makes them potentially useful for various transplantation and immune-related disease treatment purposes. In more than 95% of MSCs, the immune phenotypes are expressed at low levels of major histocompatibility complex (MHC) class I, but no MHC class II. MSCs lack surface expression of Fas-ligand or costimulatory molecules, such as B7-1 (CD80), B7-2 (CD86), CD40 or CD40L. In addition, they do express adhesion molecules involved in T cell interaction, including vascular cell adhesion molecule-1 (VCAM-1), intracellular adhesion molecule (ICAM), and lymphocyte function-associated antigen 3 (LFA-3; CD58) (41). In the absence of costimulation, T-cell and MSC engagement can result in anergy. In vitro studies have shown that MSCs suppress lymphocyte proliferation in mixed lymphocyte culture, induced by alloantigens or mitogens such as Phytohemagglutinin (PHA), Concanavalin A (Con A), tuberculin, as well as activation of T cell by CD3 and CD28 antibodies (5,15,36,40,66). The degree of MSC suppression is dosedependent and T cells do not become apoptotic or anergic, because they can be restimulated by MSC removal (15,40). It seems that MSCs inhibit T cell proliferation by mechanisms which do not require antigen presenting cells (APCs). However, MSCs did affect the maturation or functional operation of APCs. Zhang et al. (78) showed that MSCs inhibit up-regulation of CD1a, CD40, B7-1, B7-2, and HLA-DR during dendritic cell (DC) maturation. In addition, MSCs decrease the interferon (IFN)-γ, interleukin (IL)-12 and tumor necrosis factor (TNF)-α production after being co-cultured with monocytes (8). Several studies have shown a suppressive effect of MSCs on immune cytotoxicity. MSCs can function as “veto cells” to inhibit lysis when MSCs are added to the lysis assay (54). MSCs inhibited the formation of cytotoxic T lymphocytes (CTLs) but did not abrogate cytotoxic T lymphocyte- or CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation natural killer cell-induced lysis. This effect appears to be mediated by soluble factors (59). MSCs can also modulate B cell proliferation and antibody production (2,11). The immunomodulatory effects of MSCs may make them useful for immunotherapy. However, the exact mechanisms involved in the immunomodulatory effects of MSCs remain unclear. Several mechanisms have been proposed. First, regulatory T cells are thought to have a critical role in the suppression of immune responses. Recent data suggests that MSCs increased the number of regulatory CD4+CD25+ T cells in mixed lymphocyte culture or IL-2 stimulated peripheral blood mononuclear cells (PBMCs) cocultured with MSCs (1,38). Second, cell-to-cell contact molecules are considered to be involved in MSC-mediated immune suppression. However, the immunomodulatory molecules are limited in their expression on the MSC surface except for MHC I molecules. MSCs can express certain immune regulatory molecules on the surface under certain conditions or following differentiation. After differentiation of MSCs into bone, cartilage, or adipose tissues, MSCs continue to express MHC class I, but not class II (36). Furthermore, up-regulation of HLA class II by IFN-γ still did not elicit a proliferative response (29,31,54). In addition, it has been recently reported that lack of costimulation is not the reason for MSC-induced T cell unresponsiveness because retroviral transduction of MSCs with B7 molecules did not result in increased T cell proliferation (29). This suggests that deficiency in MHC expression and costimulation by MSCs are not major reasons for immune escape and immune suppression. In contrast, MSCs did down-regulate the costimulatory molecule expressing profiles on APCs (78). Furthermore, programmed cell death-1 PD1/Programmed cell death ligand 1,2 (PD-L1,2) pathway may be responsible for MSCinduced suppression via cell-cell contact (3). Third, suppression seems to be mediated by a soluble factor or factors produced by MSCs, because suppression still occurs if MSCs and lymphocytes are separated in a transwell system (66). It has reported that nitric oxide (NO), prostaglandin E2 (PGE2), IL-10, transforming growth factor-β1 (TGF-β1), hepatocyte growth factor (HGF), indoleamine 2,3-doxygenase (IDO), parathyroid hormone (PTH), bone morphogenetic protein (BMP), and IFN-γmay be involved (for reviews see refs. (61,67)). CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation MSCs are also sensitive to inflammatory signals such as microbial compounds. Recently, receptors to innate immune cells on MSCs were intensive studied. Toll-like receptor (TLR) is a family of germ line-encoded pattern-recognition receptors (PRRs) that have evolved to detect different components of foreign pathogens. It has been reported that TLR2, TLR3, TLR4, TLR7, and TLR9 are expressed by MSCs and may play a deleterious role in MSC-mediated protection (52,58). In addition, a family of β-galactoside binding proteins, galectin, was discovered in MSCs. MSCs constitutively express galectins-1, -3 and -8 at both the mRNA and protein levels. In contrast to galectin-8, galectins-1 and -3 are secreted and found on the cell surface. The single or double knockdown of galectin-1 or/and galectin-3 almost abolished the immunosuppressive capacity of MSCs (19,62). However, the data available are largely restricted to in vitro studies. In vivo biological evidence still needs to be clearly elucidated. MSCs ACT AS HSC NICHE CELLS In adults, HSCs are located mainly in the bone marrow where HSCs interact within a specific microenvironment, called the stem cell niche. Within these niches, self-renewal, proliferation, and differentiation of HSCs are sophisticatedly regulated by various intrinsic programs and an orchestral pathway. The nature and function of these niches remains unclear. The HSCs located in bone marrow are previously thought to reside in the trabecular endostream (also called the osteoblastic niche) (64). However, recent studies indicated that HSCs also favor residence in the vascular niche, reticular niche, or nestin expressing niche, depending on the state of proliferation and undifferentiated state of the HSCs. The bone marrow vascular niche is contributed to by endothelial cells (27). The reticular niche is created by a small + population of VCAM-1 reticular cells, termed chemokine (C-X-C motif) ligand 12 (CXCL12; stromal cell derived factor-1 [SDF-1])-abundant reticular (CAR) cells (63). The nestin expressing niche is created by a population of cells which positively express nestin, the endothelial and neural specific regulatory element, on the surface of membranes (44). Within these niches, various niche cells act as supportive feeder layers to attract and to anchor HSCs and HPs. In addition, niche cells also mediate CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation HSC differentiation via secretion of various soluble factors and extracellular matrix interactions. MSCs resemble plastic-adherent cell preparations isolated from bone marrow or other tissues that are very heterogeneous, comprising of only a small subset of stem cells. Since MSCs can generate several types of stromal cells that constitute the marrow niche, MSCs are considered as a niche feeder layer for hematopoiesis supportive function. By using a HSC-MSC co-culture system, hematopoietic cells were found in the supernatant and primary cobblestones areas have been formed (Figure 1B). Interaction of HSCs and MSCs provides contact signals to trigger hematopoiesis. Moreover, MSCs have been examined to generate several cytokines in cultures, such as fetal liver tyrosine kinase-3 ligand (FLT3-L), stem cell factor (SCF), IL-3 and thrombopoietin (TPO) which are essential cytokines for hematopoiesis (22,68). Results from an in vitro MSC-HSC co-culture study indicated that MSCs could provide an excellent surrogate in vitro model to understand the relative roles of various homing and adhesion pathways in hematopoiesis (21,71). MSCs IN EXPERIMENTAL AND CLINICAL HSCT Promising therapeutic effect(s) of stem cell transplantation is(are) dependent on their capacity to engraft and survive in the target tissue. However, transplantation of large amounts of donor cells into chemo-radiotherapy recipients yielded only marginal improvement in bone marrow transplantation. This is possibly in part due to poor donor-cell engraftment, loss of engraftment or increased immunogenicity of the transplanted cells in an unhealthy marrow environment. Therefore, strategies to enhance repair cells implanted into the bone marrow and to decrease immune rejection of transplanted cells by the recipients‟ immune system are key to successful HSCT treatment. Several animal studies have demonstrated that administration of donor MSCs can prolong allograft or xenograft survival after HSCT in fetal sheep, mouse, and monkey. The outcome of graft enhancement and graft rejection or GvHD prevention are summarized in Table 1 (43). In our studies, human bone marrow derived mesenchymal stem cells have been transplanted into fetal mouse and showed persistence for at least 4 months with multi-lineage differentiation potential (10). CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation However, in several murine bone marrow transplant (BMT) studies, MSCs coinfusion has failed to suppress donor anti-host allo-responses in vivo or reduce GvHD. Possible mechanisms were associated with homing failure of MSCs to secondary lymphoid tissues or the generation of memory T cells after a repeated challenge experiment (23,76). Thus, anti-GvHD potency or hematopoietic support of MSCs may be critically determined by several factors including timing of MSC infusion, context of the MSC‟s residing microenvironment, location of MSCs, and persistence in the site of GvHD. There is an urgent need for a better treatment and prevention of GvHD after ASCT. Therefore, the clinical experience and safety of MSCs arouse great interest. The immuno-modulatory effects of MSCs have offered greater possibilities of MSCs in the management of GvHD, and protective effect of MSCs on GvHD is being tested in a prospective, randomized trial. Several clinical experiences with MSC infusion on HSCT are summarized in Table 2. The first clinical trial using MSCs was a safety trial in which autologous mesenchymal progenitor cells were given (33). Subsequent trials on the use of autologous MSCs for accelerating hematological recovery were performed in breast cancer patients given autologous transplantation of peripheral blood hematopoietic cells. Rapid hematopoietic recovery was noted (30). Afterwards, several phase I/II trials aimed at evaluating the safety of MSC infusion was conducted in hematological malignant patients receiving allogeneic HCT from an human leukocyte antigen-identical sibling or haploidentical peripheral blood (PB). HC-MSC co-infusion was not associated with adverse events, GvHD was prevented, and hematopoietic recovery was prompt for most patients (4,34). One successful treatment case of severe acute GvHD with third party haploidentical MSCs has been reported by the Le Blanc group (35). MSCs have been employed in patients transplanted with umbilical cord blood (UCB) cells. In these patients, MSCs were administered without clinical adverse effects (28). Later, with MSCs used in pediatric patients including phase I–II clinical trial, infusion of MSCs was proven to be safe, prevented GvHD, and with prompt hematopoietic recovery (6,39). In one of the cases of adult patients receiving UCB transplantation with co-infusion of third-party donormobilized HSCs, MSC administration at the time of transplantation had no effect on CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation the kinetics of UCB cell engraftment, or on GvHD prevention (20). Altogether, these data indicated that co-transplantation of HSCs and MSCs is safe. MSCs are believed to modulate the immune system and may have application in the induction of tolerance in transplantation. However, concerns over the MSCs‟ usefulness in human subjects is still open to debate (65). THE MECHANISMS OF ACTION FOR MSCs TO PROMOTE HEMATOPOIETIC ENGRAFTMENT Owing to their property of immune-modulation, MSCs are being considered as a double-edged sword which can not only bring about tissue repair but also alleviate adverse inflammatory reactions such as those seen in autoimmune disorders and after allogeneic haematopoietic stem cell transplantation. There is considerable evidence that MSCs exert a hypo-immunogenic character. Experimental findings and clinical trials have demonstrated that MSCs maintain the stem cell function of HSCs, but there is still uncertainty about the real efficacy of MSCs on promoting the engraftment of donor cells and accelerating the speed of hematological recovery. However, the molecular mechanism of this interaction in vivo is hardly certified. Two possible mechanisms are contributed by HSCT failure: immune rejection and damaged hematopoiesis niche. In order to avoid tissue damage, the recipient usually receives minimal toxic condition therapy before HSCT. However, the frequency of rejection is associated with improved autologous recovery, causing allogeneic transplantation failure. Therefore, host and graft alloreactivity mediated immunological responses is usually a major cause of graft failure. To this end, with hypo-immunogenic character, MSC co-infusion may attenuate host alloreactivity and promote graft residence time in the host. However, it cannot be excluded that MSCs favor the donor HSC engraftment through non-immunological mechanisms. Damage to the recipient‟s marrow microenvironment by chemo-radiotherapy before HSCT is usually unavoidable, which might contribute to the delay in engraftment or limited numbers of grafts. MSCs may create and support a better engraftment environment for donor hematopoiesis. In hypothesis, five potential mechanisms might be involved in the hematopoietic promoting function: (1) direct cell-to-cell contact can be CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation established between MSCs and HSCs; (2) paracrine factors are secreted by MSCs; (3) extracellular matrix components secreted by MSCs build a scaffold for HSCs; (4) BM homing activity; (5) small molecules and metabolites. Most likely, all of these mechanisms work together in an orchestra of factors to regulate stem cell function (Figure 2). Cell-cell interaction MSCs exert supportive activity for hematopoiesis. In order to lead to efficient hematopoiesis, a specific junctional complex has to be formed between HSCs and MSCs. HSCs with higher self-renewal capacity demonstrated significantly higher adhesion to human MSCs (70). Studies on interactions between human HSCs and the niche of the same species are rare. Human MSCs provide a suitable model system for such studies. The globule gene expression profiles of HSCs as well as MSCs have been analyzed. Several genes and molecules up-regulated on both sides of the HSC/MSC interaction included cadherin-11, N-cadherin, integrin alpha-1 (ITGA1), alpha-5 (ITGA5, CD49e) and beta-1 (ITGB1, CD29), VCAM1, neural cell adhesion molecule 1 (NCAM1), and thrombospondin 1 (THBS1) (69,70). These results imply that molecular mechanisms essential in the maintenance of „stemness‟ are mediated by a combination of cell-cell junction proteins. However, further studies are necessary to determine the relative significance of these cell adhesion proteins. Paracrine soluble factors To date, various growth factor combinations for HSC cultures have been analyzed. SCF, Flt-3 ligand (FL), and TPO seem to play a central role, and are often added to co-cultures with stromal cells (75). MSCs secrete a variety of cytokines and growth factors that have both paracrine and autocrine activities (9). Secreted molecules might act via direct effects on the MSCs themselves, or indirectly by inducing other cells nearby, followed by alteration in their biological properties and functions. Chemokine secretion of the stromal feeder layer cells might also account for the hematopoiesis supportive effect of MSCs. The Wagner group (69) have reported that IL-6, IL-8, monocyte chemotactic protein 1 (MCP1), granulocyteCT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation colony stimulating factor (GCSF), melanoma growth-stimulating activity protein (GRO; CXCL1), Tissue inhibitor of metalloproteinase-1 (TIMP-1), and TIMP-2 were highly expressed in MSCs from bone marrow, cord blood, and adipose tissue. They also found that neither insulin-like growth factor binding protein-1 (IGFBP-1), IGFBP-2, nor IGFBP-3 had an effect on the proliferation or maintenance of a primitive immunophenotype of HPs. Many groups have demonstrated that HSCs cannot be maintained in conditioned culture medium of feeder layer cells under noncontact conditions (21,42,57). There is evidence that soluble molecules alone are not enough to maintain long-term repopulating potential. However, a reliable culture platform for maintenance or expansion of HSCs without stromal cell support still needs to be well defined. Extracellular matrix scaffold and bone marrow homing MSCs secrete extracellular matrix proteins that form a scaffold with a potential pivotal role in HSC differentiation. Fibronectin (12), Laminin (60), sulfate glycosaminoglycans (56) and various proteoglycans which reside in the bone marrow have been demonstrated to support maintenance of primitive HPs. These extracellular matrix components are also secreted by MSC feeder layer cells. It has been demonstrated that blocking of binding function of extracellular matrix proteins between HSCs and MSCs induce a significant hematopoietic supportive function impairment (70,71). Metabolites and Small molecules It has been reported that serotonin, glucose and its metabolite concentrations have been implicated in maintenance and regulation of HSC function (74). Furthermore, low oxygen partial pressure within the bone marrow has been demonstrated to enhance HP colony-forming cell expansion and maintenance of hematopoietic repopulating cells (26). However, the influence of MSCs on the composition of metabolites in their local microenvironment remains unclear. Further research is necessary to elucidate the role of hormones, small molecules, or metabolites in the regulation of stem cell function. CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation Bone marrow homing capability Despite scientific evidence indicating that MSCs possess the ability to promote engraftment, homing of MSCs to the BM and sustained engraftment also play a key role. Studies from functional experiments have been described for adhesion proteins such as N-cadherin and extracellular matrix proteins such as collagen types I, IV, and fibronectin play a potential pivotal role in homing of HSCs to the bone marrow niche in animal models (47,55,77). Gene marking or radiolabeling animal experiments have shown that MSCs are capable of homing to the BM following systemic administration. In addition, most MSCs favor the lung and secondarily the liver and other organs (13,18). Other authors have shown that active homing of MSCs into the BM depends on SDF-1, which interacts with CXCR4 on the MSC surface (73). Conversely, it cannot be excluded that the engraftmentpromoting effect is obtained by the secretion of paracrine growth factors from MSCs to promote the creation of a favorable microenvironment for the survival, proliferation and engraftment of HPs. CONCLUSIONS To date, little is known about the anatomical location, architecture and cellular composition of the hematopoietic niche. It is well accepted that self-renewal and differentiation of HSCs have to be tightly regulated by the appropriate stem cell niche via cell-to-cell contact or paracrine growth factors secreted by niche cells. Within the bone marrow, HSCs lie in close proximity to the bone endosteal surface directly in contact with endothelial cells, osteoblasts, CAR cells, nestin positive cells, and other stromal cells. Experimental findings and clinical trials have proved that MSCs maintain stem cell function of HSCs, but there is still uncertainty about a real efficacy of MSCs on promoting engraftment of donor cells and accelerating the speed of hematological recovery. The mechanisms and molecules involved in MSC functions is still remain unconfirmed. Current data suggest that MSCs exhibit two key features that could have a profound impact on their clinical use. First, MSCs can maintain immune cells in an "anergy" state through immune-related mechanisms to allogeneic CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation antigen challenge. Second, MSCs could create an accessible microenvironment to repair the damaged marrow and provide trophic factors to support the survival of donor HSCs and HPs, and this largely recapitulates their physiological effect in the niche. Thus, MSCs have been employed in the clinical setting in phase I/II clinical trials. Indeed, to date no adverse effects have been reported after MSC administration. However, longer follow-up is necessary to draw definitive conclusions on potential late adverse events. ACKNOWLEDGEMENTS The authors acknowledge financial support from Taiwan Department of Health Clinical Trial and Research Center of Excellence (DOH100-TD-B-111-004), National Science Council (NSC 98-2314-B-030-003) and Fu-Jen Catholic University [109(57)31040990-1]. CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation REFERENCES 1. Aggarwal, S.; Pittenger, M. Human mesenchymal stem cells modulate allogeneic immune cell responses. Blood 105:1815-1822; 2005. 2. Asari, S.; Itakura, S.; Ferreri, K.; Liu C. P.; Kuroda, Y.; Kandeel, F.; Mullen, Y. Mesenchymal stem cells suppress B-cell terminal differentiation. Exp. Hematol. 37(5):604-615; 2009. 3. Augello, A.; Tasso R.; Negrini S. M.; Amateis A.; Indiveri F.; Cancedda R.; Pennesi G. Bone marrow mesenchymal progenitor cells inhibit lymphocyte proliferation by activation of the programmed death 1 pathway. Eur. J. Immunol. 35:1482-1490; 2005. 4. Ball, L. M.; Bernardo, M. E.; Roelofs, H.; Lankester, A.; Cometa, A.; Egeler, R. M.; Locatelli, F.; Fibbe, W. E. Co-transplantation of ex vivo-expanded mesenchymal stem cells accelerates lymphocyte recovery and may reduce the risk of graft failure in haploidentical hematopoietic stem-cell transplantation. Blood 110:2764–2767; 2007. 5. Bartholomew, A.; Sturgeon, C.; Siatskas, M.; Ferrer, K.; McIntosh, K.; Patil, S.; Hardy, W.; Devine, S.; Ucker, D.; Deans, R.; Moseley, A.; Hoffman, R. Mesenchymal stem cells suppress lymphocyte proliferation in vitro and prolong skin graft survival in vivo. Exp. Hematol. 30:42-48; 2002. 6. Bernardo, M. E.; Ball, L. M.; Cometa, A. M.; Roelofs, H.; Zecca, M.; Avanzini, M. A.; Bertaina, A.; Vinti, L.; Lankester, A.; Maccario, R.; Ringden, O.; Le Blanc, K.; Egeler, R. M.; Fibbe, W. E.; Locatelli, F. Co-infusion of ex vivo-expanded, parental MSCs prevents life-threatening acute GvHD, but does not reduce the risk of graft failure in pediatric patients undergoing allogeneic umbilical cord blood transplantation. Bone Marrow Transplant. 46:200–207; 2011. 7. Bernardo, M. E.; Locatelli, F.; Fibbe, W. E. Mesenchymal Stromal Cells: A Novel Treatment Modality for Tissue Repair. Ann. N.Y. Acad. Sci. 1176:101–117; 2009. 8. Beyth, S.; Borovsky, Z.; Mevorach, D.; Liebergall, M.; Gazit, Z.; Aslan, H.; Galun, E.; Rachmilewitz, J. Human mesenchymal stem cells alter antigenpresenting cell maturation and induce T-cell unresponsiveness. Blood 105:22142219; 2005. 9. Caplan, A. I.; Dennis, J. E.: Mesenchymal stem cells as trophic mediators. J. Cell. Biochem. 98:1076–1084; 2006. 10. Chou, S. H.; Kuo, T. K.; Liu, M.; Lee, O. K. In utero transplantation of human bone marrow-derived multipotent mesenchymal stem cells in mice. J. Orthop. Res. CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation 24(3):301-312; 2006. 11. Corcione, A.; Benvenuto, F.; Ferretti, E.; Giunti, D.; Cappiello, V.; Cazzanti, F.; Risso, M.; Gualandi, F.; Mancardi, G.; Pistoia, V.; Uccelli, A. Human mesenchymal stem cells modulate B-cell functions. Blood 107(1):367-372; 2006. 12. Dao, M.; Hashino, K.; Kato, I.; Nolta, J. Adhesion to fibronectin maintains regenerative capacity during ex vivo culture and transduction of human hematopoietic stem and progenitor cells. Blood 92:4612–4621; 1998. 13. Devine, S.; Bartholomew, A.; Mahmud, N.; Nelson, M.; Patil, S.; Hardy, W.; Sturgeon, C.; Hewett T.; Chung T.; Stock W.; Sher D.; Weissman S.; Ferrer K.; Mosca J.; Deans, R.; Moseley, A.; Hoffman, R. Mesenchymal stem cells are capable of homing to the bone marrow of non-human primates following systemic infusion. Exp. Hematol. 29:244–255; 2001. 14. Dexter, T. M.; Allen, T. D.; Lajtha, L. G. Conditions controlling the proliferation of haemopoietic stem cells in vitro. J. Cell. Physiol. 91:335–344; 1977. 15. Di Nicola, M.; Carlo-Stella, C.; Magni, M.; Milanesi, M.; Longoni, P. D.; Matteucci, P.; Grisanti, S.; Gianni, A. Human bone marrow stromal cells suppress T-lymphocyte proliferation induced by cellular or nonspecific mitogenic stimuli. Blood 99:3838-3843; 2002. 16. Friedenstein, A.; Petrakova, K.; Kurolesova, A.; Frolova, G. Heterotopic Transplants of Bone Marrow. Transplantation 6:230–247; 1968. 17. Galotto, M.; Berisso, G.; Delfino, L.; Podesta, M.; Ottaggio, L.; Dallorso, S.; Dufour, C.; Ferrara, G. B.; Abbondandolo, A.; Dini, G.; Bacigalupo, A.; Cancedda, R.; Quarto, R. Stromal damage as consequence of high-dose chemo/radiotherapy in bone marrow transplant recipients. Exp. Hematol. 27:1460–1466; 1999. 18. Gao, J.; Dennis, J. E.; Muzic, R.; Lundberg, M.; Caplan, A. The dynamic in vivo distribution of bone marrow-derived mesenchymal stem cells after infusion. Cells Tissues Organs 169:12–20; 2001. 19. Gieseke, F.; Böhringer, J.; Bussolari, R.; Dominici, M.; Handgretinger, R.; Müller, I. Human multipotent mesenchymal stromal cells use galectin-1 to inhibit immune effector cells. Blood 116(19):3770-3779; 2010. CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation 20. Gonzalo-Daganzo, R.; Regidor, C.; Martín-Donaire, T.; Rico, M.; Bautista, G.; Krsnik, I.; Forés, R.; Ojeda, E.; Sanjuán, I.; García-Marco, J.; Navarro, B.; Gil, S.; Sánchez, R.; Panadero, N.; Gutiérrez, Y.; García-Berciano, M.; Pérez, N.; Millán, I.; Cabrera, R.; Fernández, M. Results of a pilot study on the use of thirdparty donor mesenchymal stromal cells in cord blood transplantation in adults. Cytotherapy 11:278–288; 2009. 21. Gottschling, S.; Saffrich, R.; Seckinger, A.; Krause, U.; Horsch, K.; Miesala, K.; Ho, A. D. Human Mesenchymal Stroma Cells Regulate Initial Self-Renewing Divisions of Hematopoietic Progenitor Cells by a β1-Integrin-Dependent Mechanism. Stem Cells 25:798–806; 2007. 22. Heike, T.; Nakahata, T. Ex vivo expansion of hematopoietic stem cells by cytokines. Biochem. Biophys. Acta 1592(3):313-321; 2002. 23. Highfill, S.; Kelly, R.; O‟Shaughnessy, M.; Zhou, Q.; Xia, L.; PanoskaltsisMortari, A.; Taylor, P.; Tolar, J.; Blazar, B. Multipotent adult progenitor cells can suppress graft-versus-host disease via prostaglandin E2 synthesis and only if localized to sites of allopriming. Blood 114:693–701; 2009. 24. Hiwase, S.; Dyson, P.; To, L.; Lewis, I. Cotransplantation of placental mesenchymal stromal cells enhances single and double cord blood engraftment in nonobese diabetic/severe combined immune deficient mice. Stem Cells 27:2293–2300; 2009. 25. Horwitz, E.; Le Blanc, K.; Dominici, M.; Mueller, I.; Slaper-Cortenbach, I.; Marini, F.; Deans, R.; Krause, D.; Keating, A. Clarification of the nomenclature for MSC: The International Society for Cellular Therapy position statement. Cytotherapy 7:393–395; 2005. 26. Ivanovic, Z.; Hermitte, F.; Brunet, G.; Dazey, B.; Belloc, F.; Lacombe, F.; Vezon, G.; Praloran, V. Simultaneous maintenance of human cord blood SCID repopulating cells and expansion of committed progenitors at low O2 concentration (3%). Stem Cells. 22:716–724; 2004. 27. Kiel, M.; Yilmaz, O.; Iwashita, T.; Yilmaz, O.; Terhorst, C.; Morrison, S. SLAM Family Receptors Distinguish Hematopoietic Stem and Progenitor Cells and Reveal Endothelial Niches for Stem Cells. Cell 121:1109–1121; 2005. 28. Kim, D.; Chung, Y.; Kim, T.; Kim, Y.; Oh, I. Cotransplantation of third-party mesenchymal stromal cells can alleviate single-donor predominance and increase engraftment from double cord transplantation. Blood 103:1941–1948; 2004. CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation 29. Klyushnenkova, E.; Mosca, J. D.; Zernetkina, V.; Majumdar, M.; Beggs, K.; Simonetti, D.; Deans, R.; McIntosh, K. T cell responses to allogeneic human mesenchymal stem cells: immunogenicity, tolerance, and suppression. J. Biomed. Sci. 12:47-57; 2005. 30. Koc, O.; Gerson, S.; Cooper, B.; Dyhouse, S.; Haynesworth, S.; Caplan, A.; Lazarus, H. Rapid hematopoietic recovery after coinfusion of autologous-blood stem cells and culture expanded marrow mesenchymal stem cells in advanced breast cancer patients receiving high-dose chemotherapy. J. Clin. Oncol. 18:307– 316; 2000. 31. Krampera, M.; Glennie, S.; Dyson, J.; Scott, D.; Laylor, R.; Simpson, E.; Dazzi, F. Bone marrow mesenchymal stem cells inhibit the response of naive and memory antigen-specific T cells to their cognate peptide. Blood 101:3722-3729; 2003. 32. Kuçi, S.; Kuçi, Z.; Kreyenberg, H.; Deak, E.; Pütsch, K.; Huenecke, S.; Amara, C.; Koller, S.; Rettinger, E.; Grez, M.; Koehl, U.; Latifi-Pupovci, H.; Henschler, R.; Tonn, T,; von Laer, D.; Klingebiel, T.; Bader, P. CD271 antigen defines a subset of multipotent stromal cells with immunosuppressive and lymphohematopoietic engraftment-promoting properties. Haematologica 95:651– 659; 2010. 33. Lazarus, H.; Haynesworth, S.; Gerson, S.; Rosenthal, N.; Caplan, A. Ex vivo expansion and subsequent infusion of human bone marrow-derived stromal progenitor cells (mesenchymal progenitor cells): Implications for therapeutic use. Bone Marrow Transplant. 16:557–564; 1995. 34. Lazarus H.; Koc O.; Devine S.; Curtin P.; Maziarz R.; Holland H.; Shpall, E.; McCarthy, P.; Atkinson, K.; Cooper, B.; Gerson, S.; Laughlin, M.; Loberiza, F.; Moseley, A.; Bacigalupo, A. Cotransplantation of HLA-Identical Sibling Culture-Expanded Mesenchymal Stem Cells and Hematopoietic Stem Cells in Hematologic Malignancy Patients. Biol. Blood Marrow Transplant. 11:389–398; 2005. 35. Le Blanc, K.; Rasmusson, I.; Sundberg, B.; Götherström, C.; Hassan, M.; Uzunel, M.; Ringdén, O. Treatment of severe acute graft-versus-host disease with third party haploidentical mesenchymal stem cells. Lancet 363:1439-1441; 2004. CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation 36. Le Blanc, K.; Tammik, L.; Sundberg, B.; Haynesworth, S. E.; Ringdén, O. Mesenchymal stem cells inhibit and stimulate mixed lymphocyte cultures and mitogenic responses independently of the major histocompatibility complex. Scand. J. Immunol. 57:11-20; 2003. 37. Liechty, K.; MacKenzie, T.; Shaaban, A.; Radu, A.; Moseley, A.; Deans, R.; Marshak, D.; Flake, A. Human mesenchymal stem cells engraft and demonstrate site-specific differentiation after in utero transplantation in sheep. Nat. Med. 6(11):1282-1286; 2000. 38. Maccario, R.; Podestà, M.; Moretta, A.; Cometa, A.; Comoli, P.; Montagna, D.; Daudt, L.; Ibatici, A.; Piaggio, G.; Pozzi, S.; Frassoni, F.; Locatelli, F. Interaction of human mesenchymal stem cells with cells involved in alloantigen-specific immune response favors the differentiation of CD4+ T-cell subsets expressing a regulatory/suppressive phenotype. Haematologica 90:516-525; 2005. 39. MacMillan, M.; Blazar, B.; DeFor, T.; Wagner, J. Transplantation of ex-vivo culture-expanded parental haploidentical mesenchymal stem cells to promote engraftment in pediatric recipients of unrelated donor umbilical cord blood: results of a phase I-II clinical trial. Bone Marrow Transplant. 43:1–8; 2008. 40. Maitra, B.; Szekely, E.; Gjini, K.; Laughlin, M.; Dennis, J.; Haynesworth, S.; Koç, O. Human mesenchymal stem cells support unrelated donor hematopoietic stem cells and suppress T-cell activation. Bone Marrow Transplant. 33:597-604; 2004. 41. Majumdar, M.; Keane-Moore, M.; Buyaner, D.; Hardy, W.; Moorman, M.; McIntosh, K.; Mosca, J. Charactierization and functionality of cell surface molecules on human mesenchymal stem cells. J. Biomed. Sci. 10:228-241; 2003. 42. Majumdar, M.; Thiede, M.; Haynesworth, S.; Bruder, S.; Gerson, S. Human marrow-derived mesenchymal stem cells (MSCs) express hematopoietic cytokines and support long-term hematopoiesis when differentiated toward stromal and osteogenic lineages. J. Hematother. Stem Cell Res. 9(6):841-848; 2000 43. Masuda, S.; Ageyama, N.; Shibata, H.; Obara, Y.; Ikeda, T,; Takeuchi, K.; Ueda, Y.; Ozawa, K.; Hanazono, Y. Cotransplantation with MSCs improves engraftment of HSCs after autologous intra-bone marrow transplantation in nonhuman primates. Exp. Hematol. 37:1250–1257; 2009. CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation 44. Méndez-Ferrer, S.; Michurina, T.; Ferraro, F.; Mazloom, A.; Macarthur, B.; Lira, S.; Scadden, D.; Ma'ayan, A.; Enikolopov, G.; Frenette, P. Mesenchymal and haematopoietic stem cells form a unique bone marrow niche. Nature 466:829– 834; 2010. 45. Metcalf, D. On hematopoietic stem cell fate. Immunity 26(6):669-673; 2007. 46. Nauta, A.; Westerhuis, G.; Kruisselbrink, A.; Lurvink, E.; Willemze, R.; Fibbe, W. Donor-derived mesenchymal stem cells are immunogenic in an allogeneic host and stimulate donor graft rejection in a non-myeloablative setting. Blood 108:2114–2120; 2006. 47. Nilsson, S.; Debatis, M.; Dooner, M.; Madri, J.; Quesenberry, P.; Becker, P. Immunofluorescence characterization of key extracellular matrix proteins in murine bone marrow in situ. J. Histochem. Cytochem. 46:371–377; 1998. 48. Noort, W.; Kruisselbrink, A.; in't Anker, P.; Kruger, M.; van Bezooijen, R.; de Paus, R.; Heemskerk, M.; Löwik, C.; Falkenburg, J.; Willemze, R.; Fibbe, W. Mesenchymal stem cells promote engraftment of human umbilical cord bloodderived CD34+ cells in NOD/SCID mice. Exp. Hematol. 30:870–878; 2002. 49. Ortiz, L.; Gambelli, F.; McBride, C.; Gaupp, D.; Baddoo, M.; Kaminski, N.; Phinney, D. Mesenchymal stem cells engraftment in lung is enhanced in response to bleomycin exposure and ameliorates its fibrotic effects. Proc. Natl. Acad. Sci. USA 100:8407-8411; 2003. 50. Osawa, M.; Hanada, K.; Hamada, H.; Nakauchi, H. Long-term lymphohematopoietic reconstitution by a single CD34-low/negative hematopoietic stem cell. Science 273(5272):242-245; 1996. 51. Pereira, R.; O'Hara, M.; Laptev, A.; Halford, K.; Pollard, M.; Class, R.; Simon, D.; Livezey, K.; Prockop, D. Marrow stroma cells as a source of progenitor cells for nonhematopoietic tissues in transgenic mice with a phenotype of osteogenesis imperfecta. Proc. Natl. Acad. Sci. USA 95:1142-1147; 1998. 52. Pevsner-Fischer, M.; Morad, V.; Cohen-Sfady, M.; Rousso-Noori, L.; ZaninZhorov, A. Toll-like receptors and their ligands control mesenchymal stem cell functions. Blood 109:1422–1432; 2007. 53. Pittenger, M.; Mackay, A.; Beck, S.; Jaiswal, R.; Douglas, R.; Mosca, J.; Moorman, M.; Simonetti, D.; Craig, S.; Marshak, D. Multilineage potential of adult human mesenchymal stem cells. Science. 284:143-147; 1999. 54. Potian, J. A.; Aviv, H.; Ponzio, N. M.; Harrison, J. S.; Rameshwar, P. Veto-like activity of mesenchymal stem cells: functional discrimination between cellular responses to alloantigens and recall antigens. J. Immunol. 171:3426-3434; 2003. CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation 55. Puch, S.; Armeanu, S.; Kibler, C.; Johnson, K. R.; Muller, C. A.; Wheelock, M. J.; Klein, G. N-cadherin is developmentally regulated and functionally involved in early hematopoietic cell differentiation. J. Cell Sci. 114:1567–1577; 2001. 56. Punzel, M.; Gupta, P.; Verfaillie, C. The microenvironment of AFT024 cells maintains primitive human hematopoiesis by counteracting contact mediated inhibition of proliferation. Cell Commun. Adhes. 9:149–159; 2002. 57. Punzel, M.; Liu, D.; Zhang, T.; Eckstein, V.; Miesala, K.; Ho, A. D. The symmetry of initial divisions of human hematopoietic progenitors is altered only by the cellular microenvironment. Exp. Hematol. 31:339–347; 2003. 58. Raicevic, G.; Najar, M.; Stamatopoulos, B.; De Bruyn, C.; Meuleman, N.; Bron, D.; Toungouz, M.; Lagneaux, L. The source of human mesenchymal stromal cells influences their TLR profile as well as their functional properties. Cell. Immunol. 270:207–216; 2011. 59. Rasmusson, I.; Ringdén, O.; Sundberg, B.; Le Blanc, K. Mesenchymal stem cells inhibit the formation of cytotoxic T lymphocytes, but not activated cytotoxic T lymphocytes or natural killer cells. Transplantation 76:1208-1213; 2003. 60. Sagar, B.; Rentala, S.; Gopal, P.; Sharma, S.; Mukhopadhyay, A. Fibronectin and laminin enhance engraftibility of cultured hematopoietic stem cells. Biochem. Biophys. Res. Commun. 350: 1000–1005; 2006. 61. Salem, H. K.; Thiemermann, C. Mesenchymal stromal cells: current understanding and clinical status. Stem Cells 28(3):585-596; 2010. 62. Sioud, M.; Mobergslien, A.; Boudabous, A.; Fløisand, Y. Evidence for the involvement of galectin-3 in mesenchymal stem cell suppression of allogeneic Tcell proliferation. Scan. J. Immunol. 71:267–274; 2010. 63. Sugiyama, T.; Kohara, H.; Noda, M.; Nagasawa, T. Maintenance of the hematopoietic stem cell pool by CXCL12–CXCR4 chemokine signaling in bone marrow stromal cell niches. Immunity 25:977–988; 2006. 64. Taichman, R.; Emerson, S. Human osteoblasts support hematopoiesis through the production of granulocyte colony stimulating factor. J. Exp. Med. 179:1677– 1682; 1994. 65. Tolar, J.; Le Blanc, K.; Keating, A.; Blazar, B. Concise Review: Hitting the Right Spot with Mesenchymal Stromal Cells. Stem Cells 28:1446–1455; 2010. 66. Tse, W.; Pendleton, J.; Beyer, W.; Egalka, M.; Guinan, E. Suppression of allogeneic T-cell proliferation by human marrow stromal cells: implications in transplantation. Transplantation 75:389-397; 2003. CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation 67. Uccelli, A.; Pistoia, V.; Moretta, L. Mesenchymal stem cells: a new strategy for immunosuppression? Trends Immunol. 28(5):219-226; 2007. 68. Ueda, T.; Tsuji, K.; Yoshino, H.; Ebihara, Y.; Yagasaki, H.; Hisakawa, H. Expansion of human NOD/SCID-repopulating cells by stem cell factor, Flk2/Flt3 ligand, thrombopoietin,IL-6, and soluble IL-6 receptor. J. Clin. Invest. 105(7):1013-1021; 2000. 69. Wagner, W.; Roderburg, C.; Wein, F.; Diehlmann, A.; Frankhauser, M.; Schubert, R.; Eckstein, V.; Ho, A. Molecular and secretory profiles of human mesenchymal stromal cells and their abilities to maintain primitive hematopoietic progenitors. Stem Cells 25:2638–2647; 2007. 70. Wagner, W.; Wein, F.; Roderburg, C.; Saffrich, R.; Diehmann, A.; Eckstein, V.; Ho, A. Adhesion of human hematopoietic progenitor cells to mesenchymal stromal cells involves CD44. Cells Tissues Organs. 188(1-2):160-169; 2008. 71. Wagner, W.; Wein, F.; Roderburg, C.; Saffrich, R.; Faber, A.; Krause, U.; Schubert, M.; Benes, V.; Eckstein, V.; Maul, H.; Ho, A. Adhesion of hematopoietic progenitor cells to human mesenchymal stem cells as a model for cell-cell interaction. Exp. Hematol. 35:314–325; 2007. 72. Weiss, L. The hematopoietic microenvironment of the bone marrow: an ultrastructural study of the stroma in rats. Anat. Rec. 186:161–184; 1976. 73. Wynn, R.; Hart, C.; Corradi-Perini, C.; O‟Neill, L.; Evans, C.; Wraith, J.; Fairbairn, L.; Bellantuono, I. A small proportion of mesenchymal stem cells strongly expresses functionally active CXCR4 receptor capable of promoting migration to bone marrow. Blood 104:2643–2645; 2004. 74. Yang, M.; Li, K.; Ng, P. C.; Chuen, C. K.; Lau, T. K.; Cheng, Y. S.; Liu, Y. S.; Li, C. K.; Yuen, P. M.; James, A. E.; Lee, S. M.; Fok, T. F. Promoting effects of serotonin on hema -topoiesis: ex vivo expansion of cord blood CD34+ stem/progenitor cells, proliferation of bone marrow stromal cells, and antiapoptosis. Stem Cells 25:1800–1806; 2007. 75. Yoshikubo, T.; Inoue, T.; Noguchi, M.; Okabe, H. Differentiation and maintenance of mast cells from CD34(+) human cord blood cells. Exp. Hematol. 34:320–329; 2006. 76. Zangi, L.; Margalit, R.; Reich-Zeliger, S.; Bachar-Lustig, E.; Beilhack, A.; Negrin, R.; Reisner, Y. Direct imaging of immune rejection and memory induction by allogeneic mesenchymal stromal cells. Stem Cells 27:2865–2874; 2009. CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation 77. Zhang, J.; Niu, C.; Ye, L.; Huang, H.; He, X.; Tong, W. G.; Ross, J.; Haug, J.; Johnson, T.; Feng, J. Q.; Harris, S.; Wiedemann, L. M.; Mishina, Y.; Li, L. Identification of the haematopoietic stem cell niche and control of the niche size. Nature 425:836–841; 2003. 78. Zhang, W.; Ge, W.; Li, C.; You, S.; Liao, L.; Han, Q.; Deng, W.; Zhao, R. Effects of mesenchymal stem cells on differentiation, maturation, and function of human monocyte-derived dendritc cells. Stem Cell Dev. 12:263-271; 2004. 79. Zhao, L.; Duan, W.; Reyes, M.; Keene, C.; Verfaillie, C.; Low, W. Human bone marrow stem cells exhibit neural phenotypes and ameliorate neurological deficits after grafting into the ischemic brain of rats. Exp. Neurol. 174:11-20; 2002. 80. Zipori, D.; Duksin, D.; Tamir, M.; Argaman, A.; Toledo, J.; Malik, Z. Cultured mouse marrow stromal cell lines, II. Distinct subtypes differing in morphology, collagen types, myelopoietic factors, and leukemic cell growth modulating activities. J. Cell. Physiol. 122:81-90; 1985. CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation Table 1 Animal experiments of MSC co-injection on HSCT MSC source Human BM MSC Fetal lung-derived MSC Placenta MSC Monkey BM MSC BM MSC (CD271+) Allogeneic MSC Syngeneic MSC Source of HSC Human HSC Human UCB-derived HSC Human UCB HSC Monkey BM-derived CD34+ HSC Human CD133+ HSC Murine BM-derived HSC Murine BM-derived HSC Animal model Human → sheep Human → NOD-SCID mouse Human → NOD-SCID mouse monkey → non-human primate Human → NOD-SCID mouse Mouse → mouse Mouse → mouse Outcome Enhance engraftment Enhance engraftment Enhance engraftment Enhance engraftment Enhance engraftment Promote graft-rejection Induce engraftment Ref. no. 36 48 24 43 32 46 46 Abbreviations: BM = bone marrow; HSCT = hematopoietic stem cell transplantation; HSC = hematopoietic stem cell; MSC = mesenchymal stem cells; NOS-SCID = non-obese diabetic severe combined immunodeficient mice; Ref. no. = reference number; UCB = umbilical cord blood CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation Table 2 Clinical trials of MSC infusion for enhancement of HSCT engraftment BMT type Disease HSC Source MSC Source Outcome Ref. no. Autologous MPC Autologous HSCT Allogeneic HSCT Allogeneic HSCT Double UCBT UCBT UCBT Hematological malignancy Breast cancer (PI-II) Hematological malignancy (PI-II) Hematological disorders (PI-II) Hematological disorders Hematological disorders (PI-II) Hematological disorders (PI-II) BM PB BM PB UCB UCB UCB BM BM BM BM BM BM BM UCBT + third-party donor HSC Hematological disorders (PI-II) UCB + PB BM No adverse events Enhance hematopoietic recovery Prevent GvHD Prevent graft rejection No adverse effects Enhance hematopoietic recovery No effect on engraftment; GvHD prevention No effect on engraftment and GvHD 33 30 34 4 28 39 6 20 Abbreviations: BM = bone marrow; BMT = bone marrow transplant; GvHD = graft versus host disease; HSCT = hematopoietic stem cell transplantation; HSC = hematopoietic stem cell; MSC = mesenchymal stem cells; MPC = mesenchymal progenitor cells; NOS-SCID = nonobese diabetic severe combined immunodeficient mice; PB = peripheral blood; P = phase of study; Ref. no. = reference number; UCB = umbilical cord blood; UCBT = umbilical cord blood transplantation. CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation FIGURE LEGENDS Figure 1. Phase-contrast photographs and hematopoietic differentiation of murine placenta-derived stem cells (PDSCs). (A) PDSCs show a fibroblast-like morphology in culture (20X objective). (B) Induction of cobblestone formation illustrate the hematopoietic differentiation of murine hematopoietic stem cells (HSCs) after coculture on PDSC feeder layer. Phase contrast microscopic analysis demonstrates that from the HSCs in direct cell-cell contact with the PDSC layer cells, a dull cobblestone-like area was formed. Black arrow head indicates cobblestone area (20X objective). Figure 2. The proposed dual mechanisms have illustrated that MSCs could be niche cells to maintain HSCs function via immunomodulatory or hematopoietic mediated mechanism. Through direct cell-cell contact, paracrine factors, extracellular matrix scaffold, BM homing capability, and endogenous metabolites, MSCs can escape alloreactive immune cell recognition, enhance engraftment, and to accelerate hematopoietic recovery. Abbreviations: MSCs = mesenchymal stromal cells; HSCs = hematopoietic stem cells; NKs = natural killer cells; ECM = extracellular matrix. CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation Figure 1 CT-2435 Cell Transplantation Epub Copyright © 2012 Cognizant Communication Corporation Figure 2 CT-2435 Cell Transplantation Epub 1